What does an MRI of the brain look like?
A classic example of an MRI scan of the brain is shown in the pictures below. Magnetic resonance imaging is performed in the transverse (or axial - figure below) and longitudinal (or sagittal - figure above) planes.
The study is performed in several modes. The main ones are T1 and T2. Images obtained in these modes are often also called T1-weighted or T2-weighted images. The images shown above were taken in T1 mode.
The main difference between these modes is how liquid and air are displayed in the pictures. In T1 mode, tissues containing a large amount of water have a darker color, while in T2 mode they are bright, light. This is easy to understand by looking at the pictures above - the eyeballs are visualized in the form of light paired rounded formations; on one side they are bright and light, on the other - dark. Therefore, the picture on the right was taken in T1 mode, the picture on the left in T2. There is also a difference in how the gray matter of the brain is displayed in these modes. In T2 mode it is lighter than white matter.
In fact, there are many more modes - FLAIR, DWI, STIR and so on. One mode is used to suppress the signal from fat-rich tissues, another is used to study the distribution density of protons in tissues, and a third is used to evaluate the Brownian motion of water molecules. That is why a full course of MRI diagnostics for doctors lasts more than one month.
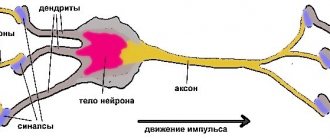
Hypomelinization of cerebral white matter
It belongs to a group of disorders in which the formation of the myelin sheath is impaired or delayed, and its images resemble those of newborns with immature myelination. On T2-weighted images, white matter characteristically appears as widespread hyperintensity that is faint compared with the cortex. If white matter lesions are not consistent with hypomyelination of cerebral white matter, it is necessary to determine whether they are confluent or multiple. 2) Confluent white matter lesions are usually caused by inherited white matter degeneration (leukodystrophy) and in most cases are bilaterally symmetrical. Several white matter lesions are usually asymmetrical and acquired. Confluent white matter lesions are further subdivided into categories 2–7 below.
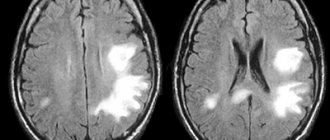
Normal and abnormalities on MRI of the brain
How do you know if there are signs of disease in the pictures? The most important thing is to remember what the brain of a healthy person looks like. The doctor, studying the photographs of patients, constantly compares them with normal photographs stored in his head. To understand how this happens, look at the pictures below:
Here are two pictures taken in the same mode. The photo below is normal. What disease, in this case, is in the top picture? To understand this, you need to compare these images. The difference is clearly visible - in the top image there is a tumor on the right side of the brain. The difference is even more noticeable if you compare the left and right sides of the same photo.
Let's mark it with a red circle. Visually, it is a node, heterogeneous in color and different from the gray and white matter of the brain. In such cases, in order to accurately determine the boundaries of the tumor and determine its type, the study is repeated with contrast. The introduction of a contrast agent into the blood through the cubital vein leads to the accumulation of the contrast agent in the tumor tissues - normal healthy tissues practically do not accumulate it. And we get the following picture, shown in the figure on the right. The bright color of the tumor corresponds to the accumulated contrast - now you can not only tell where the tumor is, but also roughly determine that it is a benign tumor, since it has clear boundaries (malignant tumors grow into surrounding tissues, which is why the boundaries will be blurred and not so clear ).
Thus, interpretation of the results of MRI of the brain is carried out by comparing the obtained images with the norm. If there are no differences, we can say that the patient whose images are examined by the doctor is most likely healthy. Everything is compared - shape, size of anatomical structures, localization, symmetry, amount of cerebrospinal fluid in the cavities of the brain, and many other parameters. Each disease, be it stroke or multiple sclerosis, has its own characteristic symptoms.
Methods of combating pathology
Irreversible consequences of brain damage require an integrated approach to treatment and fundamental changes in the usual lifestyle:
- Rejection of bad habits;
- Physical activity - walking and swimming to strengthen the heart muscle;
- Dieting - table number 10 - limiting salt, fatty and spicy foods. Mostly boiled or steamed food;
- Maintaining a rest regime - in case of brain pathologies, it is necessary to increase sleep by several hours;
- Avoidance of stress – an unstable emotional state directly affects the causes of many diseases.
Drug therapy is aimed at eliminating cognitive disorders and treating the underlying disease, which causes changes in brain tissue:
- Drugs to improve blood supply (help replenish oxygen deficiency in tissues);
- Analgesics (pain relief);
- Antiepileptic drugs (relief of convulsive syndrome);
- Beta-blockers (blood pressure control to exclude hypertensive crises);
- Non-steroidal anti-inflammatory drugs;
- B vitamins (restoration of the nervous system);
- Antidepressants (for anxiety disorders);
- Nootropic drugs (restoration of cognitive abilities).
For minor lesions, it is possible to slow down the progressive process by following the neurologist’s instructions and undergoing an annual re-examination of the cerebral vessels.
Preventive measures aimed at maintaining a healthy lifestyle and annual scheduled examinations with a neurologist can minimize the risk for people predisposed to vascular pathologies.
Dysfunctional brain disorders affect the quality of life and the course of the disease, leading to death in cases of extensive damage to brain tissue. Timely treatment does not eliminate the pathology, but it is possible to slow down the atrophic processes and improve fading vital functions.
How to Read Brain MRI Results
Now let’s try to read the MRI report of the brain with a transcript of the images using the following example:
- Scanning technique – lists the modes in which the study was carried out;
- A series of tomograms reveal small foci of ischemia - areas of the white matter of the brain experiencing oxygen deficiency (age-related changes). Any focal changes, regardless of location, are pathology;
- The following describes the cerebral cortex - slight atrophy of the frontotemporal lobes is also an age-related change (the study was carried out in an elderly person);
- Then the system of the ventricles of the brain is described - the cavities in which cerebrospinal fluid circulates - if they are not dilated and have a normal shape, then everything is normal.
- The corpus callosum, cerebellum and brain stem are unchanged;
- Next comes a description of the pituitary gland - a gland located at the base of the brain (a slight flattening is possible normally), the area of the optic chiasm, the sinuses of the internal carotid artery - also without changes, since there is no asymmetry, their contours are clear and even;
- Then comes a description of the eyeballs and the contents of the orbits - without pathological signals, i.e. fine;
- The area of the cerebellopontine angle—the origin of the auditory or vestibulocochlear nerve responsible for hearing—is unchanged, the nerve is identified on both sides;
- The paranasal sinuses are described - there is a cyst in the right maxillary sinus - the remaining sinuses are normal, pneumatization is normal (contain air, not pus or liquid);
- Next comes a study of cerebral vessels or MR angiography - no changes in caliber, symmetry, no displacement or narrowing of the lumen - the norm. Slight narrowing is allowed;
- Then venography is performed - no changes and normal caliber - normal.
In conclusion, only pathological changes are identified - in this case, these are foci of ischemia, atrophy of the frontotemporal regions, and a maxillary sinus cyst. In general, the picture corresponds to the patient’s age – 65 years. MRI signs of vascular encephalopathy - the final diagnosis will be determined by the attending physician. Please note that normally the images show no changes, focal or diffuse (evenly distributed), cysts, tumors, neoplasms, or areas of pathological hyper or hypointensity of the signal. The anatomical formations have clear, even contours, are not displaced, and are symmetrical. The vessels are symmetrical, without signs of narrowing of the lumen, with normal course and caliber, the intraluminal signal (actually blood in the vessel) is homogeneous, which indicates the absence of blood clots in the lumen of the artery or vein.
In a similar way, images are deciphered and described in any clinic. However, the accuracy of the conclusion made depends on the qualifications of the MRI diagnostic physician.
Forms of the pathological process
Depending on the damage caused by disturbances in the functioning of blood vessels and the delivery of nutrients to the brain tissues, there are:
- Discirculatory nature of the damage;
- Focal changes in the brain substance of a dystrophic nature.
Not only older patients are at risk. The pathological process in the brain structures also occurs with concomitant diseases not related to the vascular system:
- Age over 50 years;
- Metabolic disorders (obesity);
- Hypertension;
- Sedentary lifestyle (phenomena of stagnation in the vascular bed);
- Alcohol and tobacco abuse;
- Atherosclerosis;
- Diabetes;
- Vegetovascular dystonia;
- Osteochondrosis;
- Heart rhythm disturbances (bradycardia, tachycardia);
- Rheumatoid arthritis.
Discirculatory disorders
The dyscirculatory form of the pathological process is the slow development of lesions of vascular origin and has a chronic course. The initial stage does not lead to significant disruptions in the nervous system and is felt as overwork or depression; it is extremely difficult to diagnose the developing pathology.
The proliferation of vasogenic lesions leads to tissue death and is expressed by mental instability and the appearance of headaches. Extensive tissue necrosis leads to irreversible changes, the person becomes incapacitated (motor activity and intellectual abilities are impaired).
Dystrophic changes
Lack of cellular nutrition leads to focal changes in the brain of a dystrophic nature; the damaged area can be single or have a large area.
Necrotic areas can be in the form of single inclusions or have multiple foci of dead tissue. Pathological changes have a genetic predisposition and manifest themselves in the presence of unfavorable factors.
Causes:
- Traumatic brain injuries;
- Neoplasms (tumors, cysts);
- Consequences of degenerative changes (scars on brain tissue after injury);
- Osteochondrosis of the cervical spine;
- Vascular aneurysm.
The manifestation of symptoms occurs already in severe forms of the disease and an extensive focus of necrosis. The initial stage is expressed by a depressive state that is not relieved by antidepressants.
Damage to the frontal and temporal lobes of the brain results in decreased memory and concentration. The progressive process leads to degenerative changes (cannot recognize objects, speech is impaired).
Demyelinating disorders are added, expressed in disorders of the musculoskeletal system (staggering gait, lack of coordination). The development of paresis of varying intensity (tremor of the hands, head, lack of facial expressions) leads to dysphagia (inability to eat due to impaired swallowing).
The person becomes unable to control emotions (laughing or crying for no reason), changes also affect the vocal cords (nasal voice).
Sources
- Van der Knaap MS, Valk J. Classification of myelin disorders. In Van der Knaap MS, Valk J, eds. Magnetic resonance of myelination and myelin disorders. 3rd ed. Berlin: Springer, 2005, 20-24.
- Schiffmann R, van der Knaap MS. An MRI-based approach to the diagnosis of white matter disorders. Neurology 2009; 72: 750-759
- Takanashi J. Diagnostic imaging of white matter disorders. Journal of the Japan Pediatric Society 2007; 111: 1243-1254. [In Japanese]
- Van der Knaap MS, Breiter SN, Naidu S, et al. Defining and categorizing leukoencephalopathies of unknown origin: MR imaging approach. Radiology 1999; 213: 121-133.
Translated and published by: radiologist, Ph.D. Vlasov Evgeniy Aleksandrovich Full or partial reprint of this article is permitted by installing an active hyperlink to the original source
Subcortical predominance
In these disorders, lesions occur predominantly in the subcortical white matter, including U-fibers. Disorders with this pattern include L-2-hydroxyglutaric acid (Figure 6), galactosemia, Kearns-Sayer syndrome, propionic acid in the blood, urea cycle disorders, and early Canavan disease.
Figure 6. A 40-year-old woman with L-2-hydroxyglutaric aciduria. T1- and T2-weighted images revealed lesions in the subcortical white matter, including U-fibers (image courtesy of Dr. Katsumi Hayakawa, Department of Radiology, Kyoto City Hospital).
Damage with limited diffusion
In both demyelination and hypomyelination, the underlying pathology of white matter, there is a decrease in the amount of myelin that limits diffusion, and a corresponding increase in extracellular fluid results in a hyperintense T2 signal with a high diffusion coefficient (ADC). It is rare for white matter disorders to have a high T2 signal and a low ADC, and therefore this combination has high diagnostic value. Disorders characterized by intramyelin edema in the myelin sheath and in the spaces between the myelin sheaths demonstrate low ADC. These include: maple syrup urine disease, methionine adenosyltransferase I/III deficiency (Figure 9), phenylketonuria, nonketotic hyperglycinemia, and Canavan disease. Krabbe disease and metachromatic leukodystrophy may also exhibit low ADC in some white matter lesions, as intramyelin edema may occur during the acute phase of demyelination.