What to do if MRI shows signs of focal lesions?
The question of what to do in the presence of focal changes in the brain substance on MRI is most troubling to those people who do not have any significant neurological symptoms at all. This is understandable: for hypertension or atherosclerosis, treatment has most likely already been prescribed, but if there are no symptoms, then what and how to treat?
The foci of changes themselves are not treated; doctors’ tactics are aimed at the main cause of the pathology - high blood pressure, atherosclerotic changes, metabolic disorders, infection, tumor, etc.
For age-related dystrophic and dyscirculatory changes, experts recommend taking medications prescribed by a neurologist or therapist (hypotensives, statins, antiplatelet agents, antidepressants, nootropics, etc.), as well as lifestyle changes:
- Adequate rest and night's sleep;
- A balanced diet with a limit on sweets, fatty, salty, spicy foods, coffee;
- Elimination of bad habits;
- Physical activity, walks, feasible sports activities.
It is important to understand that existing focal changes will not disappear anywhere, however, through lifestyle, monitoring blood levels and pressure, you can significantly reduce the risk of ischemia and necrosis, progression of dystrophic and atrophic processes, while prolonging active life and performance for years.
Diagnostics
The doctor conducts a thorough history taking, examines the skin and mucous membranes, and palpates the patient’s lymph nodes and abdominal cavity. Prescribes a standard set of laboratory tests that help identify or exclude the causes of fever.
In the process of collecting anamnesis, increased attention is paid to the subject’s recent travels (especially to epidemiologically disadvantaged areas), contacts with people who exhibited similar symptoms, and contacts with animals. The patient is asked to talk in detail about what medications he is taking, the presence of diseases, family history, surgical interventions, injuries, immunizations.
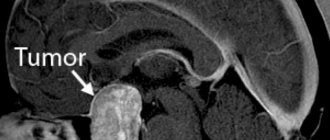
The decision to conduct additional tests is based on the results of the initial assessment and laboratory diagnostic results. An important role is played by serological and virological studies, as well as instrumental diagnostics - radiography, ultrasound, CT, PET, MRI, echocardiography, which can help identify inflammatory processes, malignant tumors, abscesses, diffuse lesions of connective tissue and blood vessels. If necessary, gastroduodenoscopy, bronchoscopy, and biopsy (lymph nodes, bone marrow, liver) may be prescribed.
Bibliography
- John Conklin, Frank L. Silver, David J. Mikulis, Daniel M. Mandell. Are acute infarcts the cause of leukoaraiosis? Brain mapping for 16 consecutive weeks. Annals of Neurology, 2014; DOI: 10.1002/ana.24285.
- Hachinski VC, Potter P, Merskey H: Leuko-araiosis, Arch Neurol. 1987; 44: 21-23.
- Revista Habanera de Ciencias Médicas, versión On-line ISSN 1729-519X.Rev haban cienc méd vol.12 no.3 Ciudad de La Habana jul.-set. 2013, CIENCIAS CLÍNICAS Y PATOLÓGICAS.
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”
Natural degeneration during aging
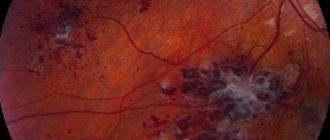
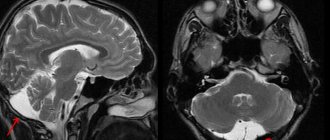
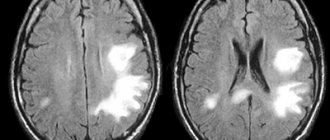
Focal changes in the brain substance of a dystrophic nature against the background of age-related involution are represented by MRI signs:
- Periventricular (around the vessels) “caps” and “stripes” - found outside the lateral ventricles, arising due to the breakdown of myelin and expansion of the perivascular spaces, proliferation of glial cells under the ependyma of the ventricles;
- Atrophic changes in the hemispheres with expansion of the grooves and the ventricular system;
- Single focal changes in the deep white matter.
Multiple focal changes of a discirculatory nature have a characteristic deep location in the white matter of the brain. The described changes will be more pronounced, and the symptoms of encephalopathy will progress with age-related hypertension.
changes in the brain with age (younger → older): leukoaraiosis around the ventricles of the brain, atrophy, focal changes
Depending on the prevalence of age-related changes, the following are distinguished:
- Mild degree - single focal changes in the white matter of point sizes in the deep parts of the brain;
- Middle - drainage pockets;
- Severe - large confluent, scattered foci of damage to nervous tissue, mainly in deep sections against the background of vascular disorders.
Causes
LNG can be caused by infectious diseases, the development of an inflammatory or malignant process, or systemic connective tissue diseases.
The most common reasons:
- infectious diseases - malaria, tuberculosis, aspergillosis, herpes, borreliosis, tick-borne encephalitis, abdominal-pelvic abscesses, prostate abscess, cholecystitis, dental infections, endocarditis, osteomyelitis, sinusitis, cytomegalovirus, Epstein-Barr virus, HIV, genitourinary infections, opportunistic infections ;
- autoimmune diseases - inflammatory bowel disease, rheumatoid arthritis, adult Still's disease, polymyalgia rheumatica, Reiter's syndrome, vasculitis, systemic lupus erythematosus, rheumatic fever;
- malignant tumors - renal cell carcinoma, hepatoma, colon cancer, pancreatic cancer, sarcomas, lymphomas, chronic leukemia, metastatic cancer.
Other reasons include:
- drug-induced fever (hypersensitivity reaction to certain medications);
- hepatitis (granulomatous, lupus, alcoholic);
- complications of liver cirrhosis;
- deep vein thrombosis;
- gout;
- Behçet's disease;
- Felty's syndrome;
- sarcoidosis;
- thyroiditis, Crohn's disease, familial periodic fever, cyclic neutropenia (rare).