They are a dense tangle of dilated vessels, in which the veins are in contact with the arteries without the participation of the capillary network due to its absence. As a result of the deviation, arterial blood is shunted into the system of deep and superficial veins without releasing nutrients and removing carbon dioxide. The size of vascular malformations can be both small and huge.
The causes of the disorder are not fully understood, but it is believed that it is not related to heredity. Symptoms can be vague and nonspecific, as a result of which the AVM is detected during a CT/MRI of the brain or spinal cord for an unrelated reason (for example, a stroke or injury). The mechanisms and consequences of the influence of AVM on human life are unpredictable, so the disease requires adequate treatment.
Causes of vascular malformations
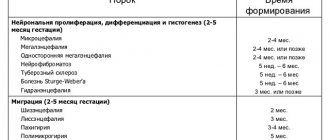
Vascular malformation is a congenital defect in the structure of the blood vessels of the central nervous system. It has a correlation with disorders of intrauterine development of the fetus and birth injuries, but the specific provoking factors for this phenomenon have not been clarified.
Local anomalies in the formation of arteries and veins of the brain occur in the embryo no later than 1-2 months of pregnancy.
To date, no direct relationship has been found between the presence of this anomaly and the age or gender of the patient.
Hemorrhagic stroke
Intracerebral hemorrhages are most common, subarachnoid hemorrhages are less common, and subdural hemorrhages are even less common.
In 60-70% of patients, the cause of hemorrhage was arterial hypertension, in 20% of cases - arterial aneurysm and arteriovenous malformation, in others - various diseases associated with atherosclerosis.
Among the reasons that determine the development of hemorrhagic stroke, the main place is occupied by hypertension and atherosclerosis.
Hemorrhagic stroke develops predominantly acutely, often without warning. It is characterized by a sudden loss of consciousness, sometimes after one or more vomitings. The patient's face becomes bluish-red, the pulse is tense and slow, breathing is loud and bubbling, the body temperature soon rises, the head and eyes are often turned to the side. Focal symptoms are primarily characterized by motor disturbances in the form of paresis and paralysis of the limbs on the side opposite to the hemorrhage, which arise as a result of compression of the internal capsule or vessels supplying it with blood by the hematoma.
Symptoms and clinical picture
An AVM may not make itself felt for many years, so patients often learn about their diagnosis by chance, while undergoing diagnostic tests for related reasons. Malformations that increase in volume can put excess pressure on the brain, and only in this case do neurological (focal) symptoms appear.
The clinical picture of the disorder is nonspecific and therefore requires in-depth differential diagnosis.
In everyday life, AVMs can manifest themselves in the following signs:
• Intracranial hypertension with a characteristic pain syndrome of a pressing or pulsating nature;
• Lethargy, apathy, decreased performance;
• Movement coordination disorder;
• Visible decrease in intellectual abilities;
• Motor aphasia and other speech disorders;
• Suppression of innervation of certain parts of the body;
• Unsteadiness of gait and sudden falls (often on the back or side);
• Muscular hypotonia and convulsive attacks;
• Visual impairment (squint, loss of visual fields, partial or complete blindness);
• Epileptic seizures of varying duration and intensity;
• Paresis of the limbs.
Symptoms of the disease are completely dependent on the location of the malformation (frontal or temporal lobe, cerebellum, base of the brain, spinal cord).
The rupture of pathologically altered vascular tangles also entails certain acute manifestations. This complication leads to internal bleeding into the brain or spinal cord, associated with a sudden disruption of their blood supply. With subarachnoid hemorrhage and the formation of a hematoma in the brain, the manifestations of the pathology become distinguishable.
The patient may complain of the following symptoms:
• A sharp and sudden attack of severe headache;
• Nausea and intense vomiting without objective reasons (the eruption of gastric contents does not bring relief);
• Syncope;
• Photophobia (pain in the eyeballs when looking at a light source or being in a lit room);
• Immobility of the eyes and visual impairment up to its complete loss;
• Violations of expressive and impressive speech (the patient pronounces inarticulate sounds and fragments of phrases, does not perceive information from outsiders);
• Convulsive seizures;
• Paralysis of limbs.
If you or your loved ones experience the following clinical manifestations of the pathology, seek professional help as a matter of urgency.
In what part of the head are brain AVMs located?
A common location for arteriovenous anomaly is the supratentorial space (upper brain) passing over the cerebellar tent. To make it clearer, let's put it simply: a vascular defect in approximately 85% of cases is found in the cerebral hemispheres. Lesions of the vascular units of the parietal, frontal, occipital, and temporal lobes of the cerebral hemispheres predominate.
In general, AVMs can be located in any pole of the brain, both in the superficial parts and in the deep layers (thalamus, etc.). It is possible to reliably determine the exact localization of the lesion only after undergoing a hardware examination with the ability to visualize soft tissues. The basic principles of diagnosis include MRI and angiography. These methods make it possible to qualitatively assess the order of branching of arteries and the construction of veins, their connection with each other, the caliber of the AVM core, afferents of arteries, draining veins.
Differential diagnosis of AVM
The best specialists in the vascular surgery department in our center organize optimal diagnostic measures to recognize the disease in any form. Differential diagnosis in our department is carried out in accordance with the highest medical standards.
Vascular malformations are determined using the following studies:
1. Assessment of the patient’s current condition, analysis of his complaints, in-depth study of the medical history;
2. Primary neurological examination, during which signs of a specific location of the AVM are identified in accordance with the clinical picture of damage to certain areas of the brain or spinal cord;
3. Computed tomography (CT) and magnetic resonance imaging (MRI), which make it possible to study the structure of the brain layer by layer, visually see the location of the AVM and its volume, and assess the general condition of the organ being studied;
4. Doppler ultrasound, which makes it possible to observe the spatial position of blood vessels in the affected area in real time, as well as differentiate pathology from other modifications of their anatomical structure;
5. Angiography, performed using a contrast agent that is injected into the vascular bed; helps evaluate the condition of veins and arteries using x-rays.
If it is difficult to make a diagnosis, you may need additional consultation with a neurologist and neurosurgeon. Typically, vascular malformation (if the patient has one) is diagnosed immediately.
Intracranial arterial aneurysms
Arterial aneurysms are a limited protrusion of the wall of an arterial vessel, looking like a thin-walled sac, in which a bottom, middle part and neck are distinguished. There is no muscle layer in the wall of the aneurysm, and in the bottom area the wall is noticeably thinner and can rupture. Most aneurysms are located in the arteries of the base of the brain, mainly in the vessels of the arterial circle of the cerebrum (Circle of Willis). The sizes of arterial aneurysms vary - from a few millimeters to giant ones, with a diameter of over 2.5 cm.
During aneurysmal disease, three periods are distinguished: pre-hemorrhagic, hemorrhagic and post-hemorrhagic.
In the pre-hemorrhagic period, which often lasts for years, the course of the disease is asymptomatic or nonspecific transient symptoms appear (headache, sometimes migraine-like in nature, temporary diplopia, dysfunction of the cranial nerves).
During the hemorrhagic period, the aneurysm ruptures with intracranial hemorrhage.
The clinical picture of the hemorrhagic period is largely determined by the size and location of the hemorrhage, repeated hemorrhages, and accompanying local and general symptoms of cerebrovascular accident.
In the posthemorrhagic period, clinical signs of an aneurysm may disappear or their severity may weaken, especially with spontaneous thrombosis of the aneurysm. Often, in the posthemorrhagic period, persistent general cerebral and focal symptoms remain, and a wide variety of visceral disorders are also added.
Repeated ruptures of arterial aneurysms are observed in more than half of patients; they can occur after several months or even years.
Methods of treating the disease
Complete therapy of patients with vascular malformations requires the ability to carry out the main treatment options - embolization, radiosurgery and surgery. Tactics are selected by an experienced specialist. At the same time, the potential risk of complications from the chosen method of therapy is assessed in relation to the risk of spontaneous progression and course of the disease.
Treatment is aimed strictly at obliterating the malformation to eliminate the threat of hemorrhage. The specialist decides how this goal will be achieved, based on the diagnostic results, individual characteristics and age category of the patient.
Surgical treatment is a rather complex procedure during which the AVM is removed from the brain through a burr hole (mechanical opening of the cranial cavity).
Radical extirpation is used in cases of large volume of AVM tangles.
Radiosurgical treatment (where the malformation is excised with a gamma knife using specific radiation) is suitable only in the case of a small vascular tangle.
The endovascular method is not so aggressive and involves blocking the lumen of the AVM through the vessel.
If treatment is ignored, vascular malformation can cause severe complications :
• Hemorrhage in the brain or spinal cord due to rupture of the AVM focus;
• Persistent movement disorders (paresis of limbs and other parts of the body);
• Severe neurological impairment.
If treatment is impossible due to the large size of the AVM, prevention of its rupture should be undertaken.
Patient reviews
Arkady Nosov: For arteriovenous malformation of the brain in my father, the operation was promptly organized, with the participation of Dr. Aronov and coordinator Anastasia, and the operation was performed by neurosurgeon Alexey Vinokurov. They completed their task very well, for which I am grateful to them. Arkady Nosov
Viktor Ivanovich: When I first encountered such a diagnosis, my attending physician Aronov suggested that I form a strong team for surgical treatment so that the chances of a successful operation were maximized. Yes, it was more expensive, but it was worth it. I agreed and now everything is over.
Carotid-cavernous anastomosis
Among the various types of cerebral vascular pathology, carotid-cavernous (carotid-cavernous) connections (ostia) are often found, which are formed as a result of damage to the internal carotid artery in the place where it passes through the cavernous sinus.
Damage to the artery can be caused by traumatic brain injury. Much less often, such compounds arise spontaneously, as a result of an infectious process, atherosclerosis, or vascular abnormalities. Violation of the integrity of the artery occurs in the places of its branches or in the places of attachment of connective tissue strands to it. Blood under high pressure enters the cavernous sinus and further through the veins flowing into the sinus - against the flow of venous blood. Over time, blood circulation shifts more and more towards the pathological connection. Through the veins flowing into the sinus, a retrograde flow of arterial blood occurs into the corresponding veins of the eye. The venous outflow is disrupted, and stagnation forms in the orbit. The sinus itself noticeably stretches and increases in size, the cranial nerves (III, IV, VI and the first branch of the V (trigeminal nerve) pairs passing through it) are compressed.
The carotid-cavernous junction is characterized by headache, dizziness, synchronous pulse noise in the head, often reminiscent of the noise of a train, which is difficult for patients to tolerate. The murmur is heard over the orbit, temporal area and mastoid process. It disappears when the carotid artery is compressed in the neck on the affected side. There are pulsating exophthalmos, which is quite well defined by palpation of the eyeball, and pronounced dilatation of the veins in the forehead and eyelids. Intraocular pressure increases, sometimes acute glaucoma develops, which can lead to decreased visual acuity and blindness. Due to damage to the oculomotor nerves, the range of movements of the eyeball decreases. Cerebrovascular accidents often lead to decreased memory, work ability, and even mental disorders.
Due to increased pressure in the veins flowing into the cavernous sinus, bleeding from the vessels of the eyeball and nose may occur. An ophthalmoscopic examination reveals dilation of the retinal veins, often their pronounced pulsation, and in some cases, swelling of the optic discs and even hemorrhages in the fundus.