...a cyst is not a tumor...
The most common type of brain cyst, occurring in 4% of the population, an arachnoid cyst is a cerebrospinal fluid (CSF)-filled sac located in the arachnoid membrane of the brain. At the site of the cyst, the tissue of the arachnoid membrane is divided into two layers with accumulation of fluid between them.
Get an MRI of the brain in St. Petersburg
It is important to remember that a cyst is not a tumor and in most cases is either asymptomatic or with minor manifestations and very rarely requires surgical intervention.
By origin, arachnoid cysts can be divided into:
- Primary, formed during intrauterine development;
- Secondary, arising as a result of injury or trauma, inflammatory processes occurring in the brain or bleeding.
According to the dynamics of development, there are cysts:
- Progressive. This type of cyst is characterized by a gradual increase in symptoms associated with the fact that the cyst, increasing in volume, increases its pressure on the brain.
- Frozen. These formations are stable and usually do not cause concern, often occur without symptoms, and some are detected only by chance during brain imaging caused by other reasons.
Classification
According to the International Classification of Diseases (ICD-10), pathology is assigned code Q04.6.
The classification of the disease is related to the location of the pathology, and the following types are distinguished:
- Arachnoid - located between the three membranes of the brain; in children, this neoplasm can provoke hydrocephalus and an increase in the volume of the skull. When diagnosing a cyst in adults, treatment is most often not required, of course, if there is no growth of pathology.
- Retrocerebellar - localized inside the organ, this neoplasm can lead to the death of brain cellular structures.
- Subarachnoid is a congenital neoplasm that can cause unsteadiness in gait, convulsions and pulsating sensations inside the skull.
- Arachnoid cerebrospinal fluid cyst - occurs in people of an older age group or those with atherosclerotic changes.
In accordance with the causes of the pathology, arachnoid cystic pathologies are divided into:
- congenital - their development occurs during the period of fetal growth in the mother’s womb, as well as during asphyxia of the child.
- acquired - develop after certain diseases, as well as under adverse environmental influences.
There is a classification of cysts according to symptoms: progressive - clinical signs increase, which is mainly due to an increase in the volume of the cystic cavity; frozen - are in a latent state and do not increase in size.
Important! To choose the correct and most effective therapy, it is very important to correctly classify the cyst.
Second opinion for arachnoid cyst
Despite the fact that MRI diagnostics using a contrast agent provides the doctor with the necessary information, there is still a risk of error. It is associated primarily with the doctor’s lack of residual experience in interpreting MRI results and identifying cysts. Not a single patient is immune from such errors, and they happen both in large cities and in small towns. In this situation, the only way to eliminate an error or at least significantly reduce its likelihood is to obtain a second opinion from a highly qualified specialist
The National Teleradiological Network (NTRS) offers you the opportunity to receive consultations from the country's leading specialists in the field of MRI diagnostics, who have extensive experience in analyzing tomographic images of various diseases. To get a consultation, you just need to upload the scan results to our server and within a day you will receive an alternative opinion to the opinion of your doctor.
Perhaps it will be the same as the first medical opinion, perhaps it will differ from it, but the second opinion will definitely allow you to reduce the risk of misdiagnosis and incorrect treatment to almost zero.
Dimensions and norm
Patients are often interested in the question of the normal size of the cyst and the volume at which surgical intervention is necessary.
It must be said that we can speak of normality only in the absence of a cystic neoplasm; if there is a cyst, then this is already an anomaly, and its size essentially does not matter much.
This type can have different sizes, but the cyst still cannot grow very much. Brain fluid resists its growth. If the size of the cyst is 1-2 mm, it is considered small; if the neoplasm grows to 1 cm, it is considered medium; cysts larger than 1 cm are considered large.
When diagnosing small cysts, doctors, as a rule, do not prescribe treatment, but choose a wait-and-see approach and simply monitor changes in the volume of the tumor. Large cysts are treated surgically; surgery is also indicated for medium-sized tumors when symptoms appear.
Treatment
Frozen arachnoid cysts with a subclinical course do not require therapy. Patients are recommended to be monitored by a neurologist and undergo an annual MRI to dynamically monitor the size of the cyst. Progressive arachnoid cysts, cysts accompanied by epilepsy and/or a significant increase in intracranial pressure that is not controlled by conservative methods of therapy are subject to surgical treatment. To decide on the advisability of surgical treatment of an arachnoid cyst and the choice of the optimal method for its implementation, a consultation with a neurosurgeon is carried out. If there is hemorrhage in the area of the arachnoid cyst or if it ruptures, complete excision of the cyst is indicated. However, this method of treatment is highly traumatic and requires a long recovery period. Therefore, in the absence of complications, preference is given to endoscopic intervention with the so-called fenestration of the cyst. The operation is performed through a burr hole and involves aspiration of the contents of the cyst, followed by the creation of holes connecting the cyst cavity with the cerebral ventricle and/or subarachnoid space. In some cases, shunt surgery is used - cystoperitoneal shunting, as a result of which cerebrospinal fluid from the cyst cavity flows into the abdominal cavity, where it is absorbed. The disadvantage of such operations is the likelihood of disruption of the shunt patency. Prevention of congenital arachnoid cysts, as well as the prevention of other intrauterine developmental defects, includes correct management of pregnancy and compliance by the pregnant woman with a special protective regime that excludes harmful effects on the fetus. Prevention of acquired arachnoid cysts is the correct and timely treatment of injuries, inflammatory and vascular cerebral diseases.
Source
Causes
Primary (congenital) cysts are formed due to abnormalities in the developing fetus, most often this occurs under the influence of the following factors:
- intoxication of the fetus with narcotic substances, alcohol, nicotine, medications that have a teratogenic effect;
- intrauterine infection of the fetus with viruses;
- irradiation;
- severe overheating of the body during pregnancy.
In addition, the formation can occur with Marfan syndrome - this is an anomaly of connective tissue, as well as with pathologies of the corpus callosum.
Secondary pathologies can develop when:
- brain injuries;
- pathological processes in the brain, for example, degenerative;
- in the presence of infections;
- deterioration of cerebral circulation.
In addition, pathology can be observed after surgery.
The mechanism of development of this neoplasm is quite complex and is associated with impaired circulation of the cerebrospinal fluid. As a result, a cavity filled with cerebrospinal fluid is formed.
Classification of brain cysts in adults.
By localization:
- Sylvian fissure (temporal lobe) 49%.
- Cerebellopontine angle 11%.
- Craniovertebral junction 10%.
- Cerebellar vermis (retrocerebellar cyst of the brain) 9%.
- Sellar and parasellar 9%.
- Interhemispheric fissure 5%.
- The convexital surface of the cerebral hemispheres is 4%.
- Slope areas 3%.
A retrocerebellar cyst of the brain can simulate Dandy-Walker syndrome, but the cerebellar vermis is preserved and the cerebrospinal fluid does not drain into the fourth ventricle.
Types of Sylvian fissure cyst.
I. is small in size, located in the region of the pole of the temporal lobe, does not cause compression, the cerebrospinal fluid flows into the subarachnoid space. II. covers the proximal and middle parts of the Sylvian fissure, almost rectangular in shape, the cerebrospinal fluid does not completely drain into the subarachnoid space. III. covers the entire Sylvian fissure, there may be a protrusion of the temporal bone, minimal drainage into the subarachnoid space, the operation often does not lead to straightening of the brain (a transition to type 2 is possible).
Certain types of congenital cysts.
- Transparent partition;
- Verge;
- Intermediate sail.
A cyst of the transparent septum of the brain is a cavity between the sheets of the transparent septum filled with cerebrospinal fluid.
It is a stage of normal development that does not last long after birth. Therefore, almost all premature babies have a cyst. Occurs in approximately 10% of adults as a congenital asymptomatic developmental anomaly that does not require treatment. A cyst of the cerebral septum can communicate with the third ventricle.
Verge's cyst is localized behind the cavity of the transparent septum and often communicates with it. Very rare.
The intermediate velum cyst forms between the thalami above the third ventricle as a result of separation of the crura of the fornix. Present in 60% of children under 1 year of age and 30% between 1 and 10 years of age. As a rule, it does not cause any changes in the clinical condition, but a large cyst can lead to occlusive hydrocephalus. In most cases, no treatment is required.
Symptomatic manifestations
This cystic neoplasm is characterized by an asymptomatic course .
Most often, such neoplasms are detected during a patient examination for neurological pathologies with similar symptoms.
The clinical signs of the cyst are nonspecific; their severity depends on the size of the tumor and its location. Patients may complain of general cerebral symptoms, which are associated with compression of brain areas. A focal clinical picture is observed in rare cases, and is most often caused by the presence of hygroma or rupture of the cystic cavity.
The main features are:
- dizziness , which are not associated with pregnancy, taking certain medications, severe fatigue, iron deficiency, and so on;
- vomiting , which is also not associated with gastrointestinal poisoning, taking medications, and so on;
- mental disorders, hallucinations ;
- convulsive syndrome;
- loss of consciousness;
- hemiparesis , decreased sensitivity in the limbs;
- failure to coordinate the activity of the body muscles;
- headaches that are not relieved by painkillers;
- a feeling of fullness , pressure, compression and increased pulsation in the affected area;
- visual and hearing problems;
- extraneous sounds in the ears;
- heaviness in the skull;
- painful or uncomfortable sensations when turning the head.
Reference! Secondary arachnoid cystic neoplasms may be accompanied by symptoms of injury or primary disease, which served as an impetus for the development of the disease.
Characteristics by location
The cyst in question may be located:
- in the temporal lobes;
- in the parietal part;
- in the frontal region;
- in the region of the cerebellum;
- in the spinal canal;
- in the spinal column;
- in the lumbar region.
In the posterior cranial fossa
This cyst in the posterior cranial fossa (posterior cranial fossa) is accompanied by symptoms:
- persistent headaches;
- vomit;
- failure to coordinate movements;
- intermittent paralysis of body parts;
- convulsive syndrome;
- mental disorders;
- hallucinations.
According to statistics, tumors of this type are more often observed in men, in addition, the increase in the volume of the cystic cavity in men occurs more actively than in women. With a very large cyst, speech defects, hearing loss, and temporary memory problems may occur.
In the sacral canal
An arachnoid type cyst in the sacral region is a cavity. In it, the spinal membrane forms web-like walls. If the cyst size is more than 1.5 cm, the patient may complain of:
- lower back pain with increased loads;
- numbness, paresis, impaired functionality of the limbs;
- headaches, blood pressure surges, dizziness;
- if the cyst is located at the S2 level, sexual function is impaired, and intestinal problems also arise.
In the temporal lobe
A cyst in the temporal lobe is most often observed on the left side. This is due to the more delicate structure of the left-sided meninges and their increased sensitivity to infections. A person with a cyst in this area experiences:
- unsteady gait;
- lack of motor coordination;
- deterioration of sensitivity of the limbs;
- convulsions;
- blackouts;
- mental disorders.
These symptoms are caused by hydrocephalus - the accumulation of fluid in the skull. A cyst of the right frontal lobe is accompanied by a similar clinical picture.
Symptoms of brain arachnoiditis
Symptoms of arachnoiditis are usually caused by intracranial hypertension , in more rare cases by liquor hypotension , as well as manifestations reflecting localization affecting the meningeal processes. Moreover, general or local symptoms may predominate, depending on this, the first symptoms and the clinical picture changes.
The initial subacute course of the disease can eventually turn into a chronic form and manifest itself in the form of general cerebral disorders:
- local headaches , the most intense - in the first half of the day can cause nausea and vomiting ;
- development of the jumping symptom , when pain occurs locally during jumping or an awkward, unabsorbed movement with landing on the heels;
- dizziness of a non-systemic nature;
- sleep disorders;
- memory impairment;
- mental disorders;
- the occurrence of causeless irritability, general weakness and increased fatigue.
Focal disorders primarily depend on the location of the development of the pathology and can manifest themselves in the form of symptoms of damage to the trigeminal, abducens, auditory and facial nerves. Besides:
- With convexital (convex) arachnoiditis, inflammatory processes affect areas of the central gyri and anterior parts of the cerebral hemispheres, while the phenomena of irritation of brain structures predominate over manifestations of loss of functions, which are expressed in the form of anisoreflexia , central paresis , generalized and Jacksonian epileptic seizures , impaired circulation of cerebrospinal fluid, disorders of sensitivity and movement ( mono- or hemiparesis ).
- With inflammation of the basal sections (optic-chiasmatic, cerebellopontine and in the region of the postcranial fossa), general cerebral symptoms most often occur and the functions of the nerves of the base of the skull are disrupted.
- Optico-chiasmatic arachnoiditis is manifested by a decrease in visual acuity and changes in fields, resembling optic neuritis and combined with autonomic dysfunction - severe dermographism , increased pilomotor reflex, profuse sweating, acrocyanosis , sometimes thirst , increased urination, hyperglycemia , adiposogenital obesity , decreased sense of smell.
- Pathology affecting the region of the cerebral peduncles causes pyramidal symptoms, as well as signs of damage to the oculomotor nerves and meningeal signs.
- Arachnoiditis of the cerebellopontine angle causes headaches in the occipital region, tinnitus, neuralgia , paroxysmal dizziness, sometimes with vomiting, unilateral cerebellar disorders - when the patient staggers or supports weight on one leg, the fall occurs on the affected side; a thorough examination can reveal an ataxic gait , horizontal nystagmus , pyramidal symptoms, dilatation of the veins of the fundus, provoked by disturbances of the venous outflow.
- If the large (occipital) cistern is affected, the disease develops acutely with fever, obsessive vomiting, pain in the back of the head and cervical region, which intensifies when coughing, trying to turn the head or make a sudden movement.
- Localization of inflammatory processes in the area of IX, X, XII pairs of cranial nerves leads to nystagmus , increased tendon reflexes, pyramidal and meningeal symptoms.
- Arachnoiditis of the posterior cranial fossa can affect the V, VI, VII, VIII pair of cranial nerves and cause intracranial hypertension with meningeal symptoms, cerebellar and pyramidal disorders, for example, ataxia , asynergia , nystagmus , adiadochokinesis , headache becomes a constant symptom, one of the earliest .
- Diffuse damage is provoked by general cerebral phenomena and uneven expansion of the ventricles, which is expressed in the occurrence of frontal, hypothalamic, temporal, midbrain and cortical syndrome; the pathology initiates a disruption of the normal exchange of cerebrospinal fluid, vague pyramidal symptoms, and can affect individual cranial nerves.
Retrocerebellar type formation
This is a fairly rare pathology, which is diagnosed in 5% of the population.
This neoplasm combines several types of neoplasms that differ in location:
- arachnoid,
- intracerebral - can form in any part,
- inferior retrocerebellar.
This cyst is spoken of when the tumor is localized only in the cerebellum. In this case we observe:
- migraine;
- vomit;
- paralysis and paresis;
- problems with balance;
- the image before your eyes becomes unclear;
- decreased concentration;
- deterioration of character;
- loss of consciousness;
- twitching of the eyeballs;
- deterioration of thinking;
- violation of orientation in space and time;
- decreased muscle tone.
In children
In children, this neoplasm is diagnosed based on symptomatic manifestations and the child’s medical history.
The specialist will find out whether the child has had injuries or operations in the brain, whether he or she also suffered from meningitis, or whether there have been hemorrhages.
After this, a neurological examination is performed, and a CT or MRI is also prescribed.
It must be said that this pathology is dangerous for the child. It consists in provoking persistent neurological disorders and epileptic seizures.
Under no circumstances should parents independently treat their child, much less let the disease take its course. The baby urgently needs to be shown to a doctor who will prescribe the correct treatment regimen. If the clinical picture is pronounced, surgical intervention may be required.
Clinical picture in a newborn baby:
- strong pulsation in the fontanel region;
- limbs are flaccid;
- unoriented look.
One of the clearest signs of a cyst in a newborn is severe regurgitation during or after feeding.
Useful video on the topic:
Additional facts
An arachnoid cyst of the brain is a limited accumulation of cerebrospinal fluid (CSF) in the thickness of the membranes covering the brain. The cyst received its name due to its localization in the arachnoid cerebral membrane. At the site of cyst formation, the arachnoid membrane is thickened and has a duplication, i.e., it is divided into two layers, between which cerebrospinal fluid accumulates. As a rule, cysts have a small volume, but when a large amount of cerebrospinal fluid accumulates in them, they have a compressive effect on the underlying cerebral cortex. This leads to the manifestation of clinical manifestations of an intracranial (intracranial) space-occupying formation. Arachnoid cysts of the brain can have different locations. Most often, such cysts are located in the area of the cerebellopontine angle, the Sylvian fissure and above the sella turcica (suprasellar). According to available data, about 4% of the population have arachnoid cysts, but not everyone has any clinical manifestations. Males are more susceptible to developing cysts.
Diagnosis and treatment
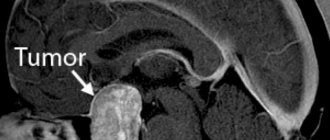
Diagnosis consists of CT or MRI.
Based on the results of these studies, it is possible to accurately determine the presence of a cyst, its size and location.
Since the cyst is considered a consequence of other pathologies, the following is prescribed:
- blood test to detect viruses, infections and autoimmune pathologies;
- prothrombin index;
- blood test for cholesterol levels;
- Doppler of cerebral vessels;
- ECG;
- monitoring blood pressure.
Small and medium cysts are treated conservatively and are prescribed:
- drugs that resolve adhesions - Longidaza, Karipatin;
- means that improve metabolic processes - Gliatilin, Actovegin;
- immunomodulators – Thymogen, Viferon;
- antiviral agents – Amiksin, Pyrogenal.
Complicated cysts, as well as large cysts that provoke an acute clinical picture, are removed surgically. This is, as a rule, an endoscopic intervention - piercing the wall of a cystic neoplasm and pumping out liquid contents from it. If such an operation is impossible, bypass surgery or microneurosurgery is performed.
Treatment with folk remedies
The use of traditional medicine for brain cysts only has a supporting effect, so I use them only when the pathology is asymptomatic. Most often used:
- hemlock;
- Caucasian Dioscorea;
- yeast elixir.
You must understand that it is impossible to cure pathology using traditional methods; they are aimed at cleansing and dilating the blood vessels of the brain, stopping inflammation and having a positive effect on brain function.
Diagnostics
The clinical picture of an arachnoid cyst has no specific manifestations and corresponds to the clinical picture common to most space-occupying brain lesions. The latter include intracerebral and meningeal hematomas, primary and metastatic brain tumors, brain abscess, and intracerebral cyst. An examination by a neurologist and a primary neurological examination (electroencephalography, rheoencephalography and echo-encephalography) make it possible to establish the presence of an intracranial formation with intracranial hypertension and existing convulsive activity of the brain. To clarify the nature of the space-occupying lesion and its localization, it is necessary to conduct an MRI, SCT of the brain or CT. The optimal diagnostic method for recognizing arachnoid cysts is MRI of the brain with contrast. The use of contrast agents makes it possible to differentiate a cyst from a brain tumor. The main criterion for an arachnoid cyst, which distinguishes it from a tumor, is the lack of the ability to accumulate contrast. Using MRI, differential diagnosis is made with subdural hematoma, subarachnoid hemorrhage, subdural hygroma, abscess, stroke, encephalitis, and other cerebral diseases.
Development options
Most often, the cyst does not interfere with brain activity. In case of an increase in the volume of the tumor and the appearance of neurological abnormalities, the options for the development of the cyst will depend on the timeliness of diagnosis and correct treatment.
When pressure increases in the head, serious problems with speech, hearing, vision and memory can occur. Persistent neurological disorders may occur. A sharp increase in the size of the tumor can provoke its rupture and death of the patient. If diagnosis and therapy are carried out on time, the prognosis is quite optimistic and after treatment the patient recovers 100%.
Description
Arachnoid cyst of the brain.
A formation filled with cerebrospinal fluid, located between the duplication of the arachnoid membrane. May be of congenital or secondary nature. It often occurs latently, without clinical manifestations. With an increase in volume, the cyst debuts with symptoms of intracranial hypertension, convulsive paroxysms and focal neurological deficit. Diagnosed mainly by MRI of the brain. When clinical symptoms increase, surgical treatment is required - drainage of the cyst, its fenestration, excision or shunting.