The most valuable thing in the life of each of us is children, which is why their health should be monitored from birth, so as not to encounter numerous problems and complications that worsen the lives of children and parents. Pseudocyst of the brain in newborns, according to experts, is the safest complication that can appear during childbirth. Approximately one in 100 cases is diagnosed with this disease.
The appearance of such a formation does not entail serious consequences, but requires close monitoring by doctors. The pathology detected in infants is not reflected in the functioning of the brain. Moreover, it does not affect mental abilities or the appearance of mental problems.
The concept of pseudocyst
Formations of the cystic type are peculiar cavities, characterized by a round shape and having a small size. They are filled with cerebrospinal fluid (exudate or other substances). The bulges are concentrated on one or both sides at the same time. The mechanism of development of this pathology in infants has not been fully studied to this day. It may happen that, in the presence of alarming prognosis, a baby is born absolutely healthy, and a second newborn is born with damage to the nervous system, with completely normal prognosis.
With the rather rapid intrauterine development of the brain, the vacated territory located in the area of the choroid plexuses is filled with a special fluid (cerebrospinal fluid). These are the processes that are observed during the development of a pseudocyst. It is safe for the life of the baby and is most often detected during an ultrasound scan of the fetus in the womb.
A large percentage of cystic formations resolve before birth. If this does not happen, then experts explain this by the presence of a herpes infection in the mother.
Causes of cerebral pseudocysts
Scientists were unable to establish the etiological factors of cystic intracerebral cavities. Verification of provoking mechanisms of development in children has been established by practice. Pathology is most often formed due to problems passing through the birth canal. Prenatal ultrasound does not indicate pseudocysts.
True cysts can be detected up to 28 weeks. Then they regress on their own.
Problems arise in children due to cerebral hemorrhage, hypoxic conditions, and cerebral circulatory pathology.
Subepindymal pseudocysts in newborns and infants are associated with the birth process, but are not congenital. Complications arise due to concomitant hemorrhages.
Pseudocyst of the choroid plexus of the right lateral ventricle
The development of cystic cavities of the choroid plexus is observed at 13-18 weeks. By this time, a mesh structure is formed inside the choroid. After filling the formation with liquid, cavities with the presence of cerebrospinal fluid are visible on ultrasound. By the twenty-eighth week of pregnancy, the cysts disappear on their own. Pseudoformations of the right ventricular plexus after birth are found during complicated pregnancy:
- Hypoxia of fetal brain tissue;
- Infections (herpes, chlamydia, cryptococcal).
The choroid plexuses in the fetus form in the sixth week. In the absence of nerve cells, fluid formation abnormalities may occur. Drops of cerebrospinal fluid after contact with the structures of the choroid plexuses lead to the formation of additional cystic cavities.
Pseudoformations of the left and right sides are equally likely to develop. Most of it resolves by 28 weeks. The pathology is formed at the beginning of intensive fetal development, when there are temporary disturbances in embryogenesis. By birth, brain function is normalized. If the formations persist after birth, the nosology usually disappears within a year.
The danger comes from the combination of pseudocysts with other brain changes:
- Diaphragmatic hernia;
- Trisomy 18 chromosomes;
- Diaphragmatic hematoma;
- Micrognathia;
- Omphalocele;
- Hydrocephalus;
- Cystic hygroma;
- Neural tube defects;
- Hammer feet.
In the presence of combined disorders, amniocentesis is performed - this is the removal of amniotic fluid for subsequent study of chromosomes. Pseudocysts with additional stigmas of disembryogenesis develop in a number of hereditary diseases (Down, Edward).
Amniocentesis is considered safe for the child, but the procedure is invasive, so it is performed according to indications.
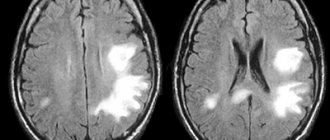
A comprehensive examination involves the use of additional neuroimaging methods:
- Neurosonography;
- Magnetic resonance imaging (MRI);
- Computed tomography (CT).
Ultrasound examination is possible in full-term infants, when the fontanelles are covered with thin bone tissue. In newborns, the lumens are open to ultrasound rays. MR and CT angiography methods are used to examine cerebral vessels after intravenous administration of a contrast agent.
Diagnostics
Ultrasound is most often used to confirm the presence of a false mass in the brain area. This method is the most popular, but it does not provide the opportunity to conduct a thorough inspection of the walls, as well as the internal space of the existing cavity. The emphasis is on specific areas where false benign formations most often form.
Particular attention is paid to the cerebral hemispheres. Also, emphasis is placed on the lateral ventricles, the area where the head of the nucleus (caudate) is located and some other areas. Features of the location of the pathology make it possible to distinguish it from a true cyst.
The presence of formations is confirmed by echo signs of a subependymal pseudocyst in the area of the right as well as the left ventricle. The use of ultrasonic waves is effective only in cases where the baby’s age has not reached 1 year. In this case, the fontanel located on the head is not covered by bones.
A newborn is examined for the presence of a pseudocyst if:
- the child was born prematurely,
- the birth was accompanied by serious complications,
- observation of insomnia, excessive tearfulness and anxiety in a newborn,
- the presence of convulsive muscle contractions, dizziness and other neurological signs.
When conducting research, the following methods for identifying the disease can be used:
- Doppler encephalography.
- Neurosonography.
- MRI and computed tomography.
- Cerebral scintigraphy and some other techniques.
If there is a suspicion that the fetus has genetic disorders, a chromosomal analysis of the fluid (amniotic fluid) may be prescribed. This intervention is invasive and is therefore used in very rare cases.
What is a subepindymal cyst?
In newborns, hemorrhages from the damaged vessel wall, localized under the ependyma, are not multiple. Usually one or two cavities containing blood are found. Gradually, the blood clots dissolve, and the vacated space is filled with cerebrospinal fluid (CSF). Formations are recorded by neurosonogram until the fontanelles close after the birth of the child.
Minor hemorrhages do not affect the functionality of the brain. There is no infection of the formations. Multiple subependymal pseudocysts do not cause neurological disorders.
Some doctors consider early closure of the fontanelles of the skull in an infant to be the reason for the long-term persistence of pseudocysts. For this reason, the child is contraindicated in taking vitamin D3, which accelerates the calcification of cartilage tissue. Physiologically, the closure of the large fontanel occurs by twelve months.
Most experts do not consider the relationship between fontanelles and brain cysts to be real. There are no objective studies confirming the presence of a relationship between nosologies.
Subepindymal pseudocysts are small (up to 4 millimeters), medium and large (about 10 mm) in size. Small cavities in children disappear on their own by the age of one year. Medium and large formations can provoke irritation of the nearby parenchyma, and therefore persist for a long time (up to 6 years). If electroencephalography reveals increased excitability of the cerebral cortex, medications are prescribed.
The localization of the subependymal cyst determines the clinical picture:
- A space-occupying formation in the back of the head is characterized by damage to the visual centers;
- Cerebellar cavity – dysfunction of the motor sphere;
- Cyst of the temporal region - hearing damage;
- Pituitary pseudocyst – endocrine imbalance.
The side of the lesion determines the location of the lesion - right or left.
What is the difference between a pseudocyst and a cyst?
A cavity formation containing cerebrospinal fluid in the central part, which occurs after the birth of a child, in adults causes clinical symptoms and is capable of progression.
Pseudocysts form in utero or directly during childbirth. The soft bones of the baby's skull, when moving along the birth canal, can cause excess pressure on the brain tissue. Lack of oxygen supply (hypoxia) leads to the formation of cystic cavities as a result of rupture of blood vessels. Gradually, such cavities resolve.
False cystic cavities are formed under the influence of the following etiological factors:
- No genetic predisposition;
- Multichamber cavities of the lateral ventricles arise due to abundant vascular ruptures;
- Pseudoformations are localized between the caudate nucleus and the optic thalamus.
The absence of damage to the tissue of the lateral ventricles and periventricular space is not accompanied by clinical symptoms.
Difference between cyst and pseudoplasm
False formations that appear in the brain area have significant differences from the true ones. They are distinguished by:
- Place of appearance. In most cases, pseudoformation is located in the zone of the subcortical nuclei, or rather between them. The pseudocyst is localized near the lateral ventricles or in the area of the cerebral hemispheres.
- Reason for appearance. The disease can be secondary or acquired. An accurate diagnosis is made through instrumental diagnostics. If a specialist has directed you to undergo an examination, you should not abandon this step, since timely detection of pathology will prevent the occurrence of serious violations.
Types of true brain cysts
There are several types of cerebral cystic cavities:
- Pathological manifestations of cystic cavities of the retrocerebellar space arise due to damage to the thickness of the brain tissue. Damage to the cerebral parenchyma occurs due to circulatory disorders, inflammatory processes (encephalitis, meningitis), after surgical interventions. Retrocerebellar cavities increase with repeated infections and bleeding;
- Arachnoid cysts are localized between the membranes. In children, education may have a congenital etiology. In adults, it forms after injury or inflammation. The danger of the arachnoid cavity lies in compression of the brain parenchyma, which is accompanied by an increase in intracranial pressure;
- The pineal cystic cavity is localized between the hemispheres. Damage to the area of the pineal gland is accompanied by disturbances in hormonal metabolism. The cause of the nosology is duct blockage, echinococcal damage;
- Subarachnoid intracerebral cyst has a congenital etiology. The clinical picture of the formation is characterized by intracranial pulsation, a feeling of instability, and muscle cramps. Diagnosis of formation is carried out using magnetic resonance imaging;
- An epiphyseal cyst of the brain is accompanied by drowsiness, disorientation in space, and double vision of objects. The symptoms are varied, but signs of damage to the pineal gland predominate. An abnormal structure is detected using magnetic resonance imaging. If the cavity is large, surgery is required to decompress the brain structures;
- Choroid plexus cyst is a type of pseudocyst. Detected by neurosonography of a pregnant woman;
- The lacunar cyst is located in the pons and subcortical structures. The main cause in older people is atherosclerosis of the arteries of the brain;
- Pineal cystic cavity is an etiological factor in the disorder of metabolic processes and motor activity. Pathology causes encephalitis and hydrocephalus;
- A limited cerebrospinal fluid cavity is located between the meninges. Etiological factors of nosology are injuries, inflammatory processes, strokes. The formation causes leg paralysis, muscle cramps, psychosis, and a gag reflex;
- Porencephalic cystic cavity is the result of past infections. The nosology is dangerous due to the development of hydrocephalus and increased intracranial hypertension. Some scientists argue about the hereditary etiology of education, as it is found in children after birth.
The described types differ from pseudo-formations on tomograms by establishing a specific location of the cavities.
Is a pseudocyst dangerous and why?
The existing pseudocyst in the head of a newborn in all cases has a second cause of development. The following reasons may act as a catalyst for the appearance:
- lack of oxygen,
- problematic childbirth,
- presence of injury.
A false cyst in an infant is not dangerous to health. This pathology should cause alarm in cases where the formation rapidly increases in size.
There is no need to perform any specific therapeutic procedures in the treatment of pseudocysts in infants. All that is necessary is to regularly visit a neurologist and carry out restorative therapy designed to combat the emergence of possible complications that often appear against the background of injury.
If after 12 months the formation and the baby have not gone away, doctors diagnose a true cyst. In such situations, you should be observed by a neurologist throughout your life.
Features of symptoms of pseudocysts in adults and newborns
In an adult, multiple cystic cavities rarely form. Single cavities do not pose a health hazard if they are not infected, and there is no increase during follow-up. True cysts in adults are diagnosed more often, which is caused by skull injuries, infectious diseases, and inflammatory processes.
Features of pseudocysts in a newborn baby
Diagnosis of pseudocystic formations is carried out in one child out of a hundred. After birth, an ultrasound examination (ultrasound) is prescribed for all premature babies, in case of complicated childbirth, or difficulties passing through the birth canal.
Oxygen starvation of the brain in utero develops after a woman experiences stress during pregnancy, infections, or the use of medications while bearing a child.
Pseudocysts of the choroid plexus are detected at 14 weeks of intrauterine development. To preliminarily identify and carry out dynamic monitoring of formations, ultrasound is performed in the first trimester of pregnancy.
Why are choroid plexus cysts dangerous in a child?
The first signs of the formation of the hemispheres during embryogenesis are the formation of choroid plexuses. The process of formation of restricted cerebrospinal fluid within the structures has not been studied. Pseudocysts do not pose a health hazard and therefore do not require urgent treatment. Dynamic observation and maintenance therapy accelerate the process of spontaneous resorption of cavities.
In most cases, pseudocysts are not dangerous. The absence of an increase in size during dynamic observation leads to positive prognosis. Growing formations that arise after heavy bleeding are dangerous. Such structures belong to the type of true cysts.
Treatment
The course of pathology observed in a newborn child should be monitored by a pediatric neurologist. The following techniques can be used during therapy.
Medicines
As a rule, doctors prescribe a number of drugs to children, the action of which is aimed at improving blood circulation in the brain, and also prescribe antihypoxants:
- Mexidol,
- Cytoflavin,
- Vitamins belonging to group B,
- Mildralex.
If hyperactivity is observed, the use of drugs such as:
- Glycine,
- Pantocalcin, as well as Pantogam.
To strengthen the musculoskeletal system, you should attend massage sessions, but only if they are recommended by your doctor.
If the false cyst was not subject to resorption during the first year of the child’s existence, and it increases in size, surgery will be required. Removal of the formation is carried out through craniotomy using endoscopy and shunting techniques.
When should I delete it?
If the formation is characterized by a tendency to increase (growth) or after a year there is no positive dynamics, then additional research is carried out for the purpose of differential diagnosis. In most cases, a diagnosis of a true brain cyst is made. If it increases in dynamics, displaces the structures of the central nervous system, and leads to functional disorders, including periodic tonic-clonic convulsions, then removal of the formation is required. It is carried out using several surgical techniques:
- microneurosurgical access;
- endoscopic surgery;
- shunt technique (fluid is discharged from the cyst into the subarachnoid space).
The choice of technique is made by a neurosurgeon individually, depending on the location, size of the formation, as well as the technical capabilities of the clinic.
Forecast
An infant with a cerebral pseudocyst develops normally during the first year of life. All indicators of maturation of the structures of the central nervous system do not differ, the child does not lag behind his peers in growth and physiological development. In most cases, when a pseudocyst is detected, the prognosis is favorable. Parents have no reason to worry. During the first year of life, dynamic monitoring by a pediatric neurologist is required. If, after a control ultrasound examination, resorption of cavity formations is noted, then a child older than one year is removed from the dispensary register.
Pseudocyst of the brain is one of the “minor” malformations of intrauterine development, which are provoked by various negative factors. Usually, when a formation is detected, special therapeutic measures are not required.