Leukoaraiosis is a brain disease that develops due to chronic processes of ischemia of the white matter, which leads to changes in tissue structure and determines the strategy for how to treat it. Due to the deterioration of blood supply to the white matter tissue, necrotic processes occur, its density decreases, and neural connections are disrupted.
Zones of leukoaraiosis form in the brain during the development of many diseases. The pathological condition reflects destructive processes occurring in brain tissue and is a characteristic symptom of diseases of the central nervous system - discirculatory encephalopathy (malfunctions of the circulatory system), dementia (dementia), multiple sclerosis (multiple replacement of brain tissue with connective tissue), stroke, Alzheimer's disease (death of neurons) .
Definition
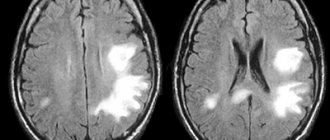
Cerebrovascular diseases are a group of brain diseases caused by pathological changes and focal dysfunction of the brain substance due to insufficient supply of tissues with oxygen and nutrients. There are acute and chronic, ischemic and hemorrhagic processes. In 1987, Khachinsky proposed the concept of leukoaraiosis (from the Greek leuko = white and araios = rarefaction) in order to define abnormalities in the white matter of the brain on CT and MRI scans. Damage can be pinpoint or wider: focal and diffuse. No clinical or pathological relationship has been proposed with this term, so it is merely a term to describe abnormal, fairly common images. That is, we are talking about a type of neuroimage that can be associated with various clinical and pathological situations, heterogeneous in the type of morphological disorders. White matter is nourished by the complex microvascular system of the brain, which consists of small threading arterioles originating from the main arteries of the brain. We are talking about the final arteries of great length and small size. Because of this, the white matter near the ventricles (in the periventricular space) becomes an area of limited vascularity, making it particularly prone to ischemia. The narrowing and reduction of blood flow in the arterioles can lead to a decrease in blood flow to a certain area and, after some time, lead to the appearance of leukoaraiosis. The development of leukoaraiosis usually follows a certain scenario. First, periventricular lesions are observed near the borders of the lateral ventricles (Fig. 1), then, depending on the severity of the problem, new lesions form around the original lesions (Fig. 2).
Fig.1
Fig.2
Degrees of leukoaraiosis at a young age
The formation of pathological foci and ischemic segments near the ventricles has different severity.
Classification of leukoaraiosis by morphology:
- 1st degree – slight loss of coordination, decreased walking speed;
- 2nd degree – development of clinical symptoms of movement disorders, loss of concentration and memory;
- Grade 3 is accompanied by a significant expansion of the ventricular spaces, increasing the manifestations of the disease. Patients require outside supervision;
- Grade 4 is characterized by uncontrolled urination, loss of balance, and suppression of psychomotor activity.
The progression of the pathology takes several years. Morphological changes are irreversible, so it is better to verify first-degree brain disorders, when supportive treatment can be selected.
The child has no clinical symptoms. Diagnosis is carried out due to the impossibility of treating speech disorders.
Degrees and symptoms
As a descriptive term, leukoaraiosis itself has no symptoms, but varying degrees of neuroimaging of these lesions are associated with corresponding symptoms. The main symptoms associated with some degrees of leukoaraiosis are ischemic stroke, cognitive impairment, gait disturbances, mood swings and sphincter disorders. There are the following degrees of leukoaraiosis from 0 to III: – 0 and I degrees are quite mild and without corresponding known specific symptoms. – II and especially III degrees are more severe, this type of leukoaraiosis affects a wider area of the white matter of the brain, damages both hemispheres, lesions are widely distributed throughout the brain, the disease becomes progressive. It is usually found in people with mental disorders that are associated with neurological damage or symptoms of dementia.
Main manifestations
It is known that a disease such as leukoaraiosis of the brain progresses as the nervous tissue is destroyed. The stronger the changes in a particular area, the brighter the signs of pathology become.
With necrosis of the white matter of the frontal part of the cerebral hemispheres, there is a decrease in intellectual abilities, speech impairment, while at the same time motor ability remains at a normal level.
The most characteristic signs of leukoaraiosis are:
- Psycho-emotional disorders;
- Memory impairment, decreased mental activity;
- Speech disorders;
- Impaired coordination of movements;
- Change in gait;
- There are sudden mood swings.
For a long time, these manifestations were considered a consequence of age-related changes. However, modern diagnostic methods have revealed a direct relationship between certain signs and the destruction of nervous tissue in a particular area.
Diagnostics
As we have already mentioned, leukoaraiosis is visible on CT and MRI neuroimages of the brain , with a decreased and increased frequency, respectively. MRI of the brain , including T2 and FLAIR series, is the most common technique for detecting leukoaraiosis. The Fazekas grading scale (Fig. 3) is most often used to determine the degree of white matter lesions on MRI images: – grade 0 : no lesions; – grade 1 : isolated lesions; – degree 2 : lesions are connected to each other; – grade 3 : lesions covering specific areas of the brain.
Fig. 3 Fazekas rating scale.
– According to the Filum System® method:
We often see images of leukoaraiosis in the white matter of the brain in horizontal MRI sections with a T2 signal, most often it is grade 1 and less often grade 2, in patients diagnosed with pathologies included in filum terminale disease or neuro-craniovertebral syndrome. Their number is about 45 % of our entire database and includes all age groups.
Chronic cerebral ischemia
Cerebrovascular diseases are one of the main problems of modern medicine. It is known that in recent years the structure of vascular diseases of the brain has changed due to the increase in ischemic forms. This is due to an increase in the proportion of arterial hypertension and atherosclerosis as the main cause of cerebrovascular pathology. When studying individual forms of cerebral circulatory disorders, chronic ischemia ranks first in prevalence.
Chronic cerebral ischemia (CHI) is a special type of vascular cerebral pathology caused by a slowly progressive diffuse disorder of the blood supply to the brain with gradually increasing various defects in its functioning. The term “chronic cerebral ischemia” is used in accordance with the International Classification of Diseases, 10th revision, instead of the previously used term “dyscirculatory encephalopathy”.
The development of chronic cerebral ischemia is promoted by a number of reasons, which are commonly called risk factors. Risk factors are divided into correctable and non-correctable. Uncorrectable factors include old age, gender, and hereditary predisposition. It is known, for example, that a stroke or encephalopathy in parents increases the likelihood of vascular diseases in children. These factors cannot be influenced, but they help to identify in advance those at increased risk of developing vascular pathology and help prevent the development of the disease. The main correctable factors in the development of chronic ischemia are atherosclerosis and hypertension. Diabetes mellitus, smoking, alcohol, obesity, insufficient physical activity, poor nutrition are the reasons that lead to the progression of atherosclerosis and the deterioration of the patient’s condition. In these cases, the blood coagulation and anticoagulation system is disrupted, and the development of atherosclerotic plaques is accelerated. Due to this, the lumen of the artery decreases or is completely blocked (Fig.). At the same time, the crisis course of hypertension is especially dangerous: it leads to an increase in the load on the blood vessels of the brain. Arteries modified by atherosclerosis are unable to maintain normal cerebral blood flow. The walls of the vessel gradually become thinner, which can ultimately lead to the development of a stroke.
| Drawing. MR angiogram: occlusion of the right middle cerebral artery |
The etiology of CCI is associated with occlusive atherosclerotic stenosis, thrombosis, and embolism. A certain role is played by post-traumatic dissection of the vertebral arteries, extravasal compression due to pathology of the spine or neck muscles, deformation of the arteries with permanent or periodic disturbances in their patency, hemorheological changes in the blood (increased hematocrit, viscosity, fibrinogen, platelet aggregation and adhesion). It must be borne in mind that symptoms similar to those that occur with chronic ischemia can be caused not only by vascular, but also by other factors - chronic infection, neuroses, allergic conditions, malignant tumors and other reasons with which a differential diagnosis should be made . If the described disorders are supposed to have a vascular origin, instrumental and laboratory confirmation of damage to the cardiovascular system is necessary (ECG, Doppler ultrasound of the main arteries of the head, MRA, MRI, CT, biochemical blood tests, etc.).
To make a diagnosis, one must adhere to strict diagnostic criteria: the presence of cause-and-effect relationships (clinical, anamnestic, instrumental) of brain lesions with hemodynamic disturbances with the development of clinical, neuropsychological, psychiatric symptoms; signs of progression of cerebrovascular insufficiency. The possibility of subclinical acute cerebral dyscirculatory disorders, including small-focal, lacunar infarctions, which form symptoms characteristic of encephalopathy, should be taken into account. For the main etiological reasons, atherosclerotic, hypertensive, mixed, and venous encephalopathies are distinguished, although other causes leading to chronic cerebral vascular insufficiency (rheumatism, vasculitis of other etiologies, blood diseases, etc.) are also possible.
The pathomorphological picture of CCI is characterized by areas of ischemically altered neurons or their loss with the development of gliosis. Small cavities (lacunae) and larger lesions develop. With multiple lacunae, the so-called “lacunary state” is formed. These changes are predominantly observed in the area of the basal ganglia and have a typical clinical expression in the form of amyostatic and pseudobulbar syndromes, dementia, described at the beginning of the twentieth century. French neurologist P. Marie. The development of status lacunaris is most characteristic of arterial hypertension. In this case, changes in blood vessels are observed in the form of fibrinoid necrosis of the walls, their plasmatic impregnation, the formation of miliary aneurysms, and stenoses.
The so-called criblures, which are dilated perivascular spaces, are distinguished as changes characteristic of hypertensive encephalopathy. Thus, the chronic nature of the process is pathomorphologically confirmed by multiple zones of brain ischemia, especially its subcortical regions and cortex, accompanied by atrophic changes developing against the background of corresponding changes in the cerebral vessels. Using CT and MRI, in typical cases, multiple microfocal changes are detected, mainly in the subcortical zones, periventricularly, often accompanied by cortical atrophy, dilation of the cerebral ventricles, and the phenomenon of leukoaraiosis (“periventricular glow”), which is a reflection of the demyelination process. However, similar changes can be observed during normal aging and primary degenerative-atrophic processes of the brain.
Clinical manifestations of CCI are not always detected by CT and MRI studies. Therefore, the diagnostic significance of neuroimaging methods cannot be overestimated. Making a correct diagnosis for a patient requires an objective analysis of the clinical picture and instrumental examination data from the doctor.
The pathogenesis of cerebral ischemia is caused by insufficiency of cerebral circulation in its relatively stable form or in the form of repeated short-term episodes of discirculation.
As a result of pathological changes in the vascular wall, developing as a result of arterial hypertension, atherosclerosis, vasculitis, etc., autoregulation of cerebral circulation is disrupted, and there is an increasing dependence on the state of systemic hemodynamics, which also turns out to be unstable due to the same diseases of the cardiovascular system. Added to this are disturbances in the neurogenic regulation of systemic and cerebral hemodynamics. Brain hypoxia itself leads to further damage to the mechanisms of autoregulation of cerebral circulation. The pathogenetic mechanisms of acute and chronic cerebral ischemia have much in common. The main pathogenetic mechanisms of cerebral ischemia constitute the “ischemic cascade” (V.I. Skvortsova, 2000), which includes:
- decreased cerebral blood flow;
- increase in glutamate excitotoxicity;
- calcium accumulation and lactic acidosis;
- activation of intracellular enzymes;
- activation of local and systemic proteolysis;
- emergence and progression of antioxidant stress;
- expression of early response genes with the development of depression of plastic proteins and a decrease in energy processes;
- long-term consequences of ischemia (local inflammatory reaction, microcirculatory disorders, damage to the BBB).
A condition called “oxidative stress” plays a major role in damage to brain neurons. Oxidative stress is an excessive intracellular accumulation of free radicals, activation of lipid peroxidation (LPO) processes and excessive accumulation of lipid peroxidation products, aggravating overexcitation of glutamate receptors and enhancing glutamate excitoxic effects. Glutamate excitotoxicity is understood as hyperstimulation by mediators of excitation of NDMA receptors of N-methyl-D-aspartate, provoking dilatation of calcium channels and, as a consequence, massive influx of calcium into cells, with subsequent activation of proteases and phospholipases. This leads to a gradual decrease in neuronal activity, a change in the neuron-glia ratio, which causes a deterioration in brain metabolism. Understanding the pathogenesis of CCI is necessary for an adequate, optimally selected treatment strategy.
As the severity of the clinical picture increases, pathological changes in the vascular system of the brain intensify. If at the beginning of the process stenotic changes in one or two main vessels are detected, then most or even all of the main arteries of the head turn out to be significantly changed. Moreover, the clinical picture is not identical to damage to the great vessels, due to the presence in patients of compensatory mechanisms of autoregulation of cerebral blood flow. The condition of intracranial vessels plays an important role in the mechanisms of compensation for cerebral circulatory disorders. With well-developed and preserved collateral circulation pathways, satisfactory compensation is possible, even with significant damage to several great vessels. On the contrary, individual structural features of the cerebral vascular system may be the cause of decompensation (clinical or subclinical), aggravating the clinical picture. This may explain the more severe clinical course of cerebral ischemia in middle-aged patients.
Based on the main clinical syndrome, several forms of CCI are distinguished: with diffuse cerebrovascular insufficiency; predominant pathology of the vessels of the carotid or vertebrobasilar systems; vegetative-vascular paroxysms; predominant mental disorders. All forms have similar clinical manifestations. In the initial stages of the disease, all patients complain of headache, non-systemic dizziness, noise in the head, memory impairment, and decreased mental performance. As a rule, these symptoms occur during a period of significant emotional and mental stress, requiring a significant increase in cerebral circulation. If two or more of these symptoms are often repeated or exist for a long time (at least the last 3 months) and there are no signs of an organic nature, instability when walking, or damage to the nervous system, a presumptive diagnosis is made.
The clinical picture of CCI has a progressive development and, according to the severity of symptoms, is divided into three stages: initial manifestations, subcompensation and decompensation.
Stage 1 is dominated by subjective disorders in the form of headaches and a feeling of heaviness in the head, general weakness, increased fatigue, emotional lability, dizziness, decreased memory and attention, and sleep disturbances. These phenomena are accompanied, although mild, but quite persistent objective disorders in the form of anisoreflexia, discoordination phenomena, oculomotor insufficiency, symptoms of oral automatism, memory loss and asthenia. At this stage, as a rule, the formation of distinct neurological syndromes (except for asthenic) has not yet occurred, and with adequate therapy, it is possible to reduce the severity or eliminate both individual symptoms and the disease as a whole.
The complaints of patients with the 2nd stage of CCI more often include memory impairment, loss of ability to work, dizziness, instability when walking, and manifestations of an asthenic symptom complex are less often present. At the same time, focal symptoms become more distinct: revival of reflexes of oral automatism, central insufficiency of the facial and hypoglossal nerves, coordination and oculomotor disorders, pyramidal insufficiency, amyostatic syndrome, increased mnestic-intellectual disorders. At this stage, it is possible to identify certain dominant neurological syndromes - discoordination, pyramidal, amyostatic, dysmnestic, etc., which can help in prescribing symptomatic treatment.
At the 3rd stage of CCI, objective neurological disorders in the form of discoordination, pyramidal, pseudobulbar, amyostatic, and psychoorganic syndromes are more pronounced. Paroxysmal conditions—falls, fainting—are more common. In the stage of decompensation, cerebral circulation disorders are possible in the form of “small strokes” or prolonged reversible ischemic neurological deficit, the duration of focal disorders in which ranges from 24 hours to 2 weeks. At the same time, the clinical picture of diffuse insufficiency of blood supply to the brain corresponds to that of moderate encephalopathy. Another manifestation of decompensation may be a progressive “complete stroke” and residual effects after it. This stage of the process with diffuse damage corresponds to the clinical picture of severe encephalopathy. Focal symptoms are often combined with diffuse manifestations of brain failure.
In chronic cerebral ischemia, there is a clear correlation between the severity of neurological symptoms and the age of the patients. This must be kept in mind when assessing the significance of individual neurological signs that are considered normal for elderly and senile people. This dependence reflects age-related manifestations of dysfunction of the cardiovascular and other visceral systems, affecting the state and functions of the brain. To a lesser extent, this dependence is observed in hypertensive encephalopathy. In this case, the severity of the clinical picture is largely determined by the course of the underlying disease and its duration.
Along with the progression of neurological symptoms, as the pathological process develops in the neurons of the brain, an increase in cognitive disorders occurs. This applies not only to memory and intelligence, which are impaired in the 3rd stage to the level of dementia, but also to such neuropsychological syndromes as praxis and gnosis. Initial, essentially subclinical disorders of these functions are observed already in the 1st stage, then they intensify, change, and become distinct. The 2nd and especially the 3rd stages of the disease are characterized by pronounced impairments of higher brain functions, which sharply reduces the quality of life and social adaptation of patients.
In the picture of CIM, several main clinical syndromes are distinguished: cephalgic, vestibulo-ataxic, pyramidal, amyostatic, pseudobulbar, paroxysmal, vegetative-vascular, psychopathological. A feature of the cephalgic syndrome is its polymorphism, inconstancy, lack of connection in most cases with specific vascular and hemodynamic factors (excluding headaches during hypertensive crises with high blood pressure), and a decrease in the frequency of occurrence as the disease progresses.
The second most common syndrome is vestibulo-ataxic syndrome. The main complaints of patients are: dizziness, instability when walking, coordination disorders. Sometimes, especially in the initial stages, patients, complaining of dizziness, do not notice coordination problems. The results of otoneurological examination are also insufficiently indicative. In later stages of the disease, subjective and objective discoordination disorders are clearly interrelated. Dizziness and unsteadiness when walking may be partly due to age-related changes in the vestibular apparatus, motor system and ischemic neuropathy of the vestibulocochlear nerve. Therefore, to assess the significance of subjective vestibulo-ataxic disorders, their qualitative analysis during a patient interview, neurological and otoneurological examination is important. In most cases, these disorders are caused by chronic circulatory failure in the blood supply of the vertebrobasilar arterial system, so it is necessary to rely not on the subjective sensations of patients, but to look for signs of diffuse damage to the parts of the brain that are supplied with blood from this vascular system. In some cases, in patients with stages 2–3 CCI, ataxic disorders are caused not so much by cerebellar-stem dysfunction, but rather by damage to the frontal-stem pathways. There is a phenomenon of frontal ataxia, or apraxia of walking, reminiscent of hypokinesia in patients with parkinsonism. A CT examination reveals significant hydrocephalus (along with cortical atrophy), i.e., a condition similar to normal pressure hydrocephalus occurs. In general, the syndrome of circulatory failure in the vertebrobasilar system is diagnosed with CCI more often than insufficiency of the carotid system.
A feature of the pyramidal syndrome is its moderate clinical manifestation (anisoreflexia, facial asymmetry, minimally expressed paresis, revitalization of oral automatism reflexes, hand symptoms). A clear asymmetry of reflexes indicates either a previously existing cerebral stroke or another disease occurring under the guise of CCI (for example, large intracranial processes, consequences of traumatic brain injury). Diffuse and fairly symmetrical revival of deep reflexes, as well as pathological pyramidal reflexes, often combined with a significant revival of oral automatism reflexes and the development of pseudobulbar syndrome, especially in old age, indicates multifocal vascular damage to the brain (subject to the exclusion of other possible causes).
In patients with clinical manifestations of circulatory failure in the vertebrobasilar system, paroxysmal conditions are often observed. These conditions may be caused by a combined or isolated effect on the vertebral arteries of vertebrogenic factors (compression, reflex), which is associated with changes in the cervical spine (dorsopathies, osteoarthritis, deformities).
Mental disorders are quite characteristic and varied in form at different stages of CCI. If in the initial stages they are of the nature of asthenic, asthenodepressive and anxiety-depressive disorders, then in the 2nd and especially in the 3rd stage they are joined by pronounced dysmnestic and intellectual disorders, forming the syndrome of vascular dementia, which often comes first in the clinical picture .
Electroencephalographic changes are nonspecific for CCI. They consist of a progressive decrease in the β-rhythm, an increase in the proportion of slow θ- and δ-activity, accentuation of interhemispheric asymmetry, and a decrease in EEG reactivity to external stimulation.
CT characteristics undergo dynamics from normal indicators or minimal atrophic signs in the 1st stage to more pronounced small-focal changes in the brain substance and atrophic (external and internal) manifestations in the 2nd stage to sharply defined cortical atrophy and hydrocephalus with multiple hypodense foci in the hemispheres - in the 3rd stage.
A comparison of clinical and instrumental characteristics in patients with atherosclerotic, hypertensive and mixed forms of CCI does not reveal any clear differences. In severe cases of hypertension, a faster rate of increase in psychoneurological disorders, early manifestation of cerebral disorders, and a greater likelihood of developing lacunar stroke are possible.
Treatment of CCI should be based on certain criteria, including the concepts of pathogenetic and symptomatic therapy. To correctly determine the pathogenetic treatment strategy, one should take into account: the stage of the disease; identified mechanisms of pathogenesis; the presence of concomitant diseases and somatic complications; age and gender of patients; the need to restore quantitative and qualitative indicators of cerebral blood flow, normalize impaired brain functions; the possibility of preventing recurrent cerebral dysgemia.
The most important direction of CCI therapy is the impact on existing risk factors, such as arterial hypertension and atherosclerosis. Treatment of atherosclerosis is carried out according to generally accepted regimens using statins, in combination with correction of the diet and lifestyle of patients. The selection of antihypertensive drugs and the order of their prescription is carried out by a general practitioner, taking into account the individual characteristics of patients. Complex therapy for CCI includes the prescription of antioxidants, antiplatelet agents, drugs that optimize brain metabolism, and vasoactive drugs. Antidepressants are prescribed for severe asthenodepressive manifestations of the disease. Antiasthenic drugs are prescribed in the same way.
An important component of the treatment of CCI is the administration of drugs with antioxidant activity. Currently, the following drugs of this series are used in clinical practice: Actovegin, Mexidol, Mildronate.
Actovegin is a modern antioxidant, which is a deproteinized extract of the blood of young calves. Its main effect is to improve the utilization of oxygen and glucose. Under the influence of the drug, the diffusion of oxygen in neuronal structures significantly improves, which makes it possible to reduce the severity of secondary trophic disorders. There is also a significant improvement in cerebral and peripheral microcirculation against the background of improved aerobic energy exchange of vascular walls and the release of prostacyclin and nitric oxide. The resulting vasodilation and decrease in peripheral resistance are secondary to the activation of oxygen metabolism of the vascular walls (A. I. Fedin, S. A. Rumyantseva, 2002).
In case of CCI, it is advisable to use Actovegin, especially in the absence of effect from other treatment methods (E. G. Dubenko, 2002). The method of application consists of drip administration of 600–800 mg of the drug for 10 days, followed by switching to oral administration.
A constant in the treatment regimen for CCI is the use of drugs that optimize cerebral circulation. The most commonly used drugs are: Cavinton, Halidor, Trental, Instenon.
Halidor (bencyclane) is a drug that has a multidirectional mechanism of action due to phosphodiesterase blockade, antiserotonin action, and calcium antagonism. It inhibits the aggregation and adhesion of platelets, prevents the aggregation and adhesion of erythrocytes, increasing the elasticity and osmotic resistance of the latter. Halidor reduces blood viscosity, normalizes intracellular metabolism of glucose and ATP, affects phosphokinase and lactate dehydrogenase, and enhances tissue oxygenation. It has been proven that the use of this drug for 8 weeks eliminates the clinical manifestations of chronic cerebral vascular insufficiency in 86% of patients. The drug has a positive effect on a person’s emotional environment, reduces forgetfulness and absent-mindedness. Halidor is prescribed in a daily dose of 400 mg for 6–8 weeks.
Instenon is a combined drug with neuroprotective action, including a vasoactive agent from the group of purine derivatives, a substance that affects the state of the ascending reticular formation and cortical-subcortical relationships, and, finally, an activator of tissue respiration processes under hypoxic conditions (S. A. Rumyantseva, 2002; B V. Kovalchuk, 2002).
The three components of instenon (etophylline, etamivan, hexobendine) jointly act on various parts of the pathogenesis of ischemic brain damage.
Etophylline, a vasoactive component of the purine series, activates myocardial metabolism with an increase in stroke volume. The transition from a hypokinetic type of blood circulation to a normokinetic one is accompanied by an increase in cerebral blood flow. An important effect of the component is an increase in renal blood flow and, as a consequence, dehydration and diuretic effects.
Etamivan has a nootropic effect in the form of a direct effect on the processes of memory, attention, mental and physical performance as a result of increased activity of the reticular formation of the brain.
Hexobendine selectively stimulates metabolism based on increased utilization of oxygen and glucose, due to increased anaerobic glycolysis and pentose cycles. At the same time, the physiological mechanisms of autoregulation of cerebral and systemic blood flow are stabilized.
Instenon is used intramuscularly 2.0 ml, course - 5-10 procedures. Then oral administration of instenon-forte continues, 1 tablet 3 times a day for a month (S. V. Kotov, I. G. Rudakova, E. V. Isakova, 2003). A clear regression of neurological symptoms is observed by the 15th–20th day of treatment. A particularly good effect is observed with the combined use of Actovegin (drops) and instenon (intramuscular injections or oral administration). Instenon therapy has a positive effect on cognitive functions, especially on the regulation of mnestic activity and psychomotor functions.
In the complex therapy of CCI, much attention is paid to nootropic drugs that increase the resistance of brain tissue to various adverse metabolic influences (ischemia, hypoxia). The actual “nootropic” drugs include derivatives of piracetam (nootropil, lutetam), encephabol.
Piracetam increases the synthesis of high-energy phosphates (ATP), enhances aerobic metabolism under hypoxic conditions, facilitates impulse conduction, normalizes the ratio of phospholipids of cell membranes and their permeability, increases the density and sensitivity of receptors, improves interaction between the cerebral hemispheres, improves metabolic processes in the central nervous system, facilitates neuronal transfer.
Piracetam improves microcirculation due to its disaggregant properties, facilitates the conduction of nerve impulses, and improves interaction between the hemispheres of the brain. The drug normalizes the ratio of phospholipids of cell membranes and increases their permeability, prevents the adhesion of red blood cells, reduces platelet aggregation, reduces the levels of fibrinogen and factor VIII, and relieves spasm of arterioles. The drug is prescribed in a daily dose of 2.4–4.8 g for 8–12 weeks.
Encephabol is a derivative of pyritinol. The drug increases the density and sensitivity of receptors, normalizes neuroplasticity. It has a neuroprotective effect, stimulates learning processes, improves memory, memorization and concentration. Encephabol stabilizes the cell membranes of neurons by inhibiting lysosomal enzymes and preventing the formation of free radicals, improves the rheological properties of blood, increases the conformational ability of red blood cells, increasing the ATP content in their membrane. For adults, the average daily dose is 600 mg for 6–8 weeks.
Antiplatelet drugs include acetylsalicylic acid and its derivatives (cardiomagnyl, thrombo ACC). Given the presence of contraindications when prescribing acetylsalicylic acid, other drugs with antiplatelet activity (Curantil, Tiklid, Plavix) are often used.
Symptomatic therapy for CCI includes the prescription of drugs that reduce the manifestations of various symptoms of the disease. For all patients with stages 2–3 of the disease, it is advisable to prescribe anti-anxiety or antidepressant drugs. Benzodiazepine drugs are the safest for long-term use.
Grandaxin is an atypical benzodiazepine derivative, a selective anxiolytic. The drug effectively eliminates anxiety, fear, and emotional stress without sedation or muscle relaxation. The drug has a vegetative-corrective effect, which makes it possible to use it in patients with severe vegetative-vascular syndrome.
In neurological practice, a daily dose of 50–100 mg is used, the duration of use is determined individually for each patient.
The prevalence of chronic vascular pathology of the brain, the progression of its course, and the high degree of disability of patients determine the social and medical significance of the problem of CCI therapy. Currently, in clinical practice there is a trend towards increasing the use of non-drug treatment methods. This is due to the absence in patients of the phenomenon of addiction to medicinal substances with a long period of therapeutic aftereffect.
Considering the complexity of the pathogenetic mechanisms of CCI, during therapy it is necessary to achieve normalization of systemic and cerebral circulation, adjust the metabolism in the brain tissue, and the state of hemorheology. Currently, the possibilities for pharmacological correction of the manifestations of CCI are quite extensive; they allow the use of various drugs that affect all parts of the pathogenesis of post-ischemic and post-hypoxic damage to nervous tissue.
Thus, recognizing the causes, identifying risk factors and, therefore, the real possibility of effective targeted treatment and preventing the development of chronic cerebral vascular pathology requires accurate knowledge of the structural, physiological and clinical features of the manifestation of the disease. This becomes possible thanks to a systematic approach to the study of etiology, pathogenesis, clinical picture and modern methods of therapy.
M. V. Putilina , Doctor of Medical Sciences, Professor
RGMU, Moscow
Causes
Currently, the pathogenesis of leukoaraiosis is controversial. Some authors recall that it has not yet been clarified to what extent the mechanisms that provoke small foci of ischemia coincide with those that cause extensive diffuse leukoaraiosis. In addition, it is unknown whether the pathological abnormalities associated with leukoaraiosis are the cause or consequence of lesions in the white matter. There are two main hypotheses: an abnormality in self-regulation of blood flow or a violation of the blood-brain barrier . The most recognized mechanism for the appearance of leukoaraiosis today is chronic ischemia due to damage to penetrating arteries. Hypertension and other pathologies affecting blood flow and oxygen supply to the brain appear to be closely associated with extensive leukoaraiosis. – According to the Filum System® method: Based on the observed association between leukoaraiosis and individual small foci of ischemia on images in patients diagnosed with filum terminale disease and neuro-craniovertebral syndrome , our center has developed a hypothesis for a possible pathogenesis: leukoaraiosis may also be associated with tension of the spinal cord due to too tight filum terminale. In this case, ischemia can appear in all tissues of the nervous system due to the collapse of small-diameter blood vessels.
Stages of development
Leukoaraiosis of the head, as a disease, goes through three stages of development:
- With stage 1 of the disease, a medical examination can reveal revitalization of tendon reflexes, human instability, a reduction in step length when walking, and the ability to move only slowly. Neuropsychological examination reveals suppression of cognitive changes. The person complains of poor attention and memory deterioration, and cognitive activity is significantly reduced.
- At stage 2, the presence of clinical syndromes is clearly visible. The patient notices memory deterioration, and at the same time mental and psychomotor reactions slow down. A person cannot control his actions and notices uncertainty in his own walking. In some cases, the presence of apathy, depression, irritability and lethargy is noted. There is deterioration in the functioning of the genitourinary system - uncontrolled urination at night. A person loses social adaptation, which manifests itself in the form of deterioration in performance and the inability to care for oneself independently.
- At stage 3 , the clinical picture worsens and leads the patient to disability. Behavioral disorders are clearly noticeable (severe lethargy, inability to walk independently, which sometimes ends in a fall, chronic urinary incontinence). At this stage, doctors note pronounced signs of a disorder in the functioning of the cerebellum.
Risk factors
On the one hand, recognized risk factors for cerebrovascular disease relate to hereditary or individual characteristics and lifestyle . On the other hand, the main risk factors for the appearance of leukoaraiosis are: age and hypertension , although it is also associated with diseases such as diabetes mellitus, heart disease or arterial stenosis, which affect the disturbance of the microcirculation of the brain, leading to demyelization of vascular origin, which can provoke the appearance of foci of ischemia. Leukoaraiosis is also associated with older age and senile dementia , although it is often found in relatively young people (approximately 40 years of age) who use drugs such as heroin, tobacco , or are in constant contact with toxic substances . Such people are prone to the appearance of leukoaraiosis of any degree. Arteriosclerosis also considered one of the factors in its appearance. – According to the Filum System® method : Patients with leukoaraiosis in the white matter of the brain and diagnoses of filum terminale disease and neuro-craniovertebral syndrome have a common risk factor: family predisposition . Tension in the nervous system caused by filum terminale (filum terminale disease) can cause disruption of the blood supply to the spinal cord and throughout the nervous system. This is a genetic disease that is inherited.
What is cerebral leukoaraiosis
The absence of an established etiology of the disease requires the identification of provoking factors. The condition is provoked by impaired blood supply, ischemia (insufficient oxygen supply), encephalopathy, Alzheimer's disease, multiple sclerosis. It is detected accidentally after magnetic resonance imaging of the primary nosological form.
The morphological substrate of the disease is destructive changes in nerve fibers with loss of myelin. Loss of the sheath results in a “short circuit” where nerve signal transmission is disrupted. The overlapping of unprotected nerve trunks on top of each other leads to a redistribution of the transmitting impulse, like exposed electrical wires.
Morphological changes in the zone of leukoaraiosis:
- Local intracerebral edema;
- Formation of cysts;
- Expansion of spaces around blood vessels;
- Single lacunar infarctions.
Clinical symptoms of white matter changes do not form. The absence of signs excludes earlier detection of pathology.
Treatment
There are usually several effective treatments to delay the development of leukoaraiosis, which are recommended depending on the disease to which it occurs. The most appropriate treatment to delay the development of leukoaraiosis is to maintain a balanced diet, with foods rich in folic acid, folates and B vitamins. It is recommended to avoid toxic substances and an unhealthy lifestyle. – According to the Filum System® method : Given the fact that leukoaraiosis is common in patients with filum terminale disease, in our center patients who have areas of ischemia in the white matter on brain MRI are recommended to undergo a diagnosis using the Filum System® in order to determine whether there is disease of the filum terminale. If there is tension on the filum terminale, then dissection of the filum terminale is proposed with an exclusive minimally invasive technique. In several cases, a decrease in leukoaraiosis has been observed after cutting the filum terminale, further suggesting that its occurrence may be associated with abnormal tension in the nervous system.
Goals and methods of therapy
The main goal of treatment is to reduce the manifestation of symptoms that are a consequence of disruption of the human brain.
The doctor prescribes medications to the patient whose action is aimed at optimizing metabolic processes and improving blood flow to the brain. Medicines reduce spasms and improve blood circulation and cell nutrition.
For this purpose, one of the following drugs is selected: Piracetam, Oxiracetam, Nitroglycerin, Aspirin, Nimodipine, Cinnarizine, Eufillin.
Self-medication for such a serious illness is not worthwhile. Only a specialist in this matter will be able to correctly calculate the dose and choose the right drug. For this purpose, you should visit the office of a neurologist, who should additionally pay attention to all associated pathologies.
Today, there are methods for treating the disease without the use of medications.
Moderate physical activity promotes rapid recovery. To choose the right load, you should consult with a physical therapy doctor and perform therapeutic exercises yourself at home. Swimming has a positive effect on the body, so the patient is recommended to visit the pool regularly.
Therapeutic massage is used to further strengthen muscle tone. Only a qualified and experienced specialist will be able to correctly navigate the required complex and apply it correctly. To obtain the best result, it is advisable to use all methods in combination.
The patient is advised to completely stop drinking alcohol and smoking. He should eat a balanced diet and exclude fatty foods from the diet. Particular attention should be paid to the consumption of vegetables and fruits, fish. If a person loves meat, then the choice should be a low-fat variety.
A favorable outcome can be expected only if the pathology is detected in a timely manner. With the help of a properly selected integrated approach to therapy, it is possible to significantly slow down the progression of the disease. Therapeutic methods are used not only to eliminate pathology, but also to improve the flow of blood to the brain.
Bibliography
- John Conklin, Frank L. Silver, David J. Mikulis, Daniel M. Mandell. Are acute infarcts the cause of leukoaraiosis? Brain mapping for 16 consecutive weeks. Annals of Neurology, 2014; DOI: 10.1002/ana.24285.
- Hachinski VC, Potter P, Merskey H: Leuko-araiosis, Arch Neurol. 1987; 44: 21-23.
- Revista Habanera de Ciencias Médicas, versión On-line ISSN 1729-519X.Rev haban cienc méd vol.12 no.3 Ciudad de La Habana jul.-set. 2013, CIENCIAS CLÍNICAS Y PATOLÓGICAS.
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”
Preventive measures
To date, there is no vaccine or medicine that could protect against the development of leukoaraiosis in the future.
For preventive purposes, doctors may advise leading a healthy lifestyle. A person should live in a mode of moderate activity and monitor nutrition. It is important to give up bad habits, because they have a detrimental effect on the functioning of the central nervous system.
If there is a cerebrovascular disease, the patient should receive timely treatment. Older people should have their functioning assessed regularly.
Clinical picture
Pervinintercular leukoaraiosis can manifest itself without characteristic symptoms. Clinical manifestations may not be observed for a long time. Signs occur if brain damage is long-lasting . This is also affected by the progression of the disease. The main symptoms include:
- defects, speech disorders;
- disturbance of emotional mood (frequent stress, tendency to depression, chronic form of dysphoria);
- significant memory impairment;
- intellectual abilities decrease.
Each affected person can independently detect characteristic changes. If the disease is detected in time, then within a short time, a person can cure it. Symptoms correspond to a certain stage of pervinticular leukoariasis.
It is worth noting that symptoms may manifest differently in each person. Only a doctor can diagnose the disease after certain diagnostics.