The coordinated work of the internal systems of our body and its response to external influences is ensured by the nervous system (NS). The spinal cord and brain form the central nervous system, and the nerves form the peripheral nervous system. Those nerves that leave the brain are called cranial (the outdated name is cranial). They have different lengths and branches, have their own names and are numbered using Roman numerals. Depending on the functions of their constituent fibers, nerves are divided into sensory (providing connections between the brain and sensory organs), motor (innervating muscles) and mixed.
The twelfth (XI) pair - the hypoglossal nerve - is motor and provides movement of the tongue.
Symptoms of damage to the hypoglossal nerve
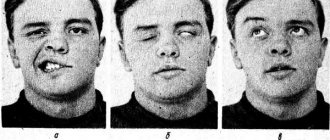
With neuropathy of the hypoglossal nerve, weakness of the tongue appears when speaking and difficulty swallowing. As the disease progresses, tongue weakness increases. Depending on the level of nerve damage, central or peripheral paresis develops. Peripheral damage occurs when the nucleus of the hypoglossal nerve, as well as the nerve fibers emanating from it, is damaged. Hypotonia of the tongue muscles on the affected side is noted, the surface of the tongue becomes wrinkled and uneven; muscle atrophy gradually appears in the tongue. A distinctive feature is fibrillary twitching in the muscles of the tongue. The tongue deviates in the direction of the lesion. Damage to the nerve on both sides is more severe (20%) - glossoplegia (immobility of the tongue) and speech impairment in the form of dysarthria occur.
| Peripheral type lesion of the left hypoglossal nerve | Damage to the left hypoglossal nerve of the central type |
Anatomy and innervation
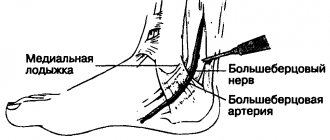
The hypoglossal nerve emerges in the form of several nerve roots from the corresponding nucleus (nerve center), located in the substance of the medulla oblongata. It passes through the hypoglossal canal, where branches are separated from it and go to the dura mater. The nerve then travels down the neck and then up to the muscles of the tongue. In this region, it divides into lingual branches, which innervate the external and internal lingual muscles, with the exception of the palatoglossus (the vagus nerve is responsible for this muscle).
Along the course of the hypoglossal nerve, other branches depart from it, connecting to the vagus nerve node, the trigeminal branch, etc.
The main function of the nerve is to ensure the movements of the tongue and, accordingly, participate in the acts of chewing, swallowing, sucking and licking.
The position of the nerve in the neck may vary. In people with short necks it is located higher than in people with long necks.
Treatment of hypoglossal nerve damage
- Anticholinesterase drugs, B vitamins.
- Oral hygiene.
- Treatment of the underlying disease.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
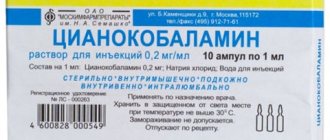
- Prozerin (inhibitor of acetylcholinesterase and pseudocholinesterase). Dosage regimen: orally for adults, 10-15 mg 2-3 times a day; subcutaneously - 1-2 mg 1-2 times a day.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
Causes of lesions and clinical manifestations
Causes of damage to the twelfth pair of cranial nerves include:
- infectious and inflammatory lesions;
- vascular pathologies;
- autoimmune disorders;
- ALS (amyotrophic lateral sclerosis);
- trauma (for example, a fracture of the base of the skull);
- compression by a tumor or aortic aneurysm;
- nerve tumor (neurinoma, neurofibroma);
- exposure to toxic substances (arsenic, lead, carbon monoxide, alcohol, etc.), etc.
Symptoms of hypoglossal nerve damage are determined by the location of the lesion.
Damage to the cerebral cortex leads to the development of central paralysis of the hypoglossal nerve. In this case, the muscles of the side of the tongue opposite the pathological focus are weakened or paralyzed, but do not atrophy. When trying to stick out the tongue, it deviates away from the area of pathology. There is also a speech disorder, without a swallowing disorder.
When the lesion is localized on the peripheral part of the nerve, the protruding tongue moves towards the area of pathology. The muscles of the paralyzed part of the tongue atrophy, it becomes uneven and wrinkled.
With atrophy of the orbicularis muscle of the tongue, it is difficult for the patient to whistle, and his lips become thinner.
The progression of the pathology leads to impairment of speech, up to complete impossibility (anarthria), and swallowing, etc. If nerve damage develops against the background of amyotrophic lateral sclerosis, then twitching and spasms of the tongue are a characteristic manifestation.
Combined damage to the hypoglossal, vagus and glossopharyngeal nerves is called bulbar syndrome. With unilateral damage, paralysis of the soft palate, larynx and epiglottis, nasal and hoarseness of the voice, slurred speech, and swallowing disorders are observed. Bilateral damage leads to death.
Recommendations
A consultation with a neurologist and magnetic resonance imaging of the brain are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Causes of neuralgia of the submandibular and sublingual nodes
The following factors can provoke the development of neuralgia of the submandibular and sublingual nodes:
- physical impact - prolonged or regular hypothermia of the ganglia;
- chronic inflammatory processes in the oral cavity - stomatitis, multiple caries, gingivitis, periodontitis;
- infectious pathologies - viral diseases, sepsis, syphilis, tuberculosis;
- chronic diseases of the digestive system and pelvic organs;
- negative consequences of surgical interventions - removal or prosthetics of teeth;
- foci of infection in nearby organs - sore throat, otitis media, sinusitis.
Often neuralgia can appear due to intoxication of the body with poisons, salts of heavy metals, and low-quality alcohol. It can also develop against the background of allergic and endocrine diseases, and be one of the manifestations of hypovitaminosis.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 | 0 | 0 | 0 | 0.3 | 0.5 | 0.8 | 0.8 |
Symptoms of neuralgia of the submandibular and sublingual nodes
The first manifestations of the disease will be paroxysmal pain (paroxysms) on the side of the inflamed ganglia. The duration of a painful attack varies from several minutes to an hour. The pain syndrome is characterized by intensity and pulsation in the area of localization of the affected ganglia. A distinctive feature of most vegetative ganglionitis of the face and head is a tendency to expand pain. The stronger and more advanced the inflammatory process, the more extensive areas are affected by pain during paroxysm.
Attacks begin from the inflamed node in the area of the root of the tongue and tonsils, then the pain spreads and occupies increasingly larger areas - over the entire half of the head, neck, collarbone, shoulder and arm. The occurrence of pain can be triggered by tension in the facial muscles and thermal effects, that is, during a conversation or eating hot, spicy food.
Neuralgia of the submandibular and sublingual nodes is divided into two stages:
- The initial ganglioneuralgic phase of neuralgia of the sublingual and submandibular ganglia: characterized by the paroxysmal pain described above, may be accompanied by swelling, increased sensitivity of the tongue and mucous membranes of the oral cavity. The pain may migrate to various areas of the head and upper torso.
- The ganglioneuritic phase of ganglion neuralgia is already a transition to a chronic form. At this stage of the development of the disease, dull pain in the affected side is constantly present, disturbances in salivation, trophic ulcers appear, possible decrease in sensitivity and signs of autonomic neurological Bernard-Horner syndrome.
In some cases, during a severe painful attack, patients experience such manifestations of the disease as chills, increased heart rate, increased blood pressure, gastrointestinal spasms, nausea, vomiting, feelings of anxiety and fear. The chronic form of the disease is the most dangerous, fraught with peripheral circulatory disorders, spasms and autonomic changes in nerve endings in the submandibular and sublingual area, as well as in nearby areas.
Clinical picture
The pathology is accompanied by acute pain in the subradicular region of the tongue or one tonsil. The pain can spread to the soft tissues of the palate, ear, pharynx and other organs. Neuralgia has a one-sided short-term course (no more than 3 minutes).
Symptoms intensify while moving the tongue. Against the background of intense pain, the quality of life deteriorates and insomnia appears.
Other characteristic features:
- dryness of the mucous membranes of the oral cavity;
- increased salivation after an attack.
A neurological disorder can enter a stage of exacerbation and remission. Over time, the frequency of attacks increases, and the pain intensifies. Some patients report loss of taste perception.
Treatment methods
It is important to consult a doctor immediately after the first characteristic symptoms appear. Timely treatment increases the chances of a full recovery. Neuralgia requires long-term therapy, the tactics of which are determined depending on the clinical condition of the patient and the course of the disease.
Conservative therapy
The patient is prescribed:
- taking non-steroidal anti-inflammatory analgesics;
- antiepileptic drugs;
- neuroleptics;
- muscle relaxants;
- a complex of vitamins and microelements to strengthen the immune system.
If oral administration is ineffective, the patient is prescribed injections of blockades under the tongue. Anesthetics are used for local treatment of the oral cavity. To increase efficiency, physiotherapeutic procedures (for example, exposure to diadynamic and sinusoidal currents, galvanization) are prescribed in combination with drug treatment.
Surgery
The operation is performed to release the compressed nerve. For this purpose, the method of microvascular decompression is used in the area where the nerve process exits the brain. If indicated, it may be necessary to dissect the hypoglossal ligament and shorten the styloid process.
The manipulation is carried out using endoscopic microsurgical equipment, which minimizes the impact on healthy tissue and prevents negative consequences.
Negative consequences may occur after an incorrectly performed intervention (for example, re-infection or injury to the affected area). Timely treatment and compliance with the recommendations of the attending physician increases the chances of a favorable outcome.
Symptoms of neuralgia of the glossopharyngeal nerve
The disease manifests itself in the form of attacks of pain that cover areas innervated by the glossopharyngeal nerve: the nasopharynx, the back of the tongue, the tonsils, and the ear. Typically attacks last from a few seconds to 3 minutes. As a rule, pain occurs on one side, several times a day, causing you to wake up at night.
Pain may occur or intensify during chewing, swallowing, laughing, coughing, talking.
We will call you back
Message sent!
expect a call, we will contact you shortly
Treatment of neuralgia of the submandibular and sublingual nodes
Complex therapy of the disease is carried out under the supervision of a specialist. The methods, manipulations and drugs used in treatment depend on the degree and form of the disease, as well as the reasons that provoked its occurrence.
- Etiological therapy is the elimination of foci of infection and other causes that provoked the disease. If necessary, treatment is carried out with the involvement of specialized specialists if the cause of the disease is chronic pathologies of internal organs.
- Pathogenic therapy is drug treatment using methods for therapeutic blockade, drugs to improve blood circulation and tissue metabolism, vitamins and antispasmodics. During the treatment, blockers of the cholinergic system, ganglion blockers, and adrenergic blockers are used.
- Sympathetic therapy is the removal of acute painful symptoms for general and mental recovery. For treatment, sedatives and hypnotics are used, and in rare cases, antidepressants.
An important step in the treatment of neuralgia of the submandibular and sublingual nodes will be physiotherapeutic methods and reflexology - laser therapy, cryotherapy, acupuncture, electrophoresis, galvanization, etc.
The success of treatment and the speed of recovery directly depends on the timeliness of contacting a specialist. The reason for contacting may be discomfort and pain in the sublingual and submandibular area, pain and swelling of the tongue, pain when the vocal cords are strained and when eating. At the first appearance of attacks of pain, even if they are observed quite rarely, it is important to make an appointment with a neurologist without delay.
Causes of the disease
Most often, the disease occurs in people over forty years of age. Often it is not possible to figure out what led to damage to the glossopharyngeal nerve. Some possible reasons:
- Compression by bony outgrowths in the lower part of the skull.
- Compression by poorly located arteries, aneurysms.
- Infections of the mouth and throat (for example, chronic inflammation of the tonsils - tonsillitis).
- Tumors of the mouth and throat.
Painful attacks can be caused by dangerous diseases, for example, tumors at the base of the skull. In order to establish the cause, you need to visit a neurologist and undergo an examination.
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.