Correspondence consultation
The key to successful rehabilitation in our clinic is targeted action on the affected areas in combination with modern drug therapy.
There is a considerable amount of truth in the hackneyed phrase “All diseases come from nerves.” Polyneuropathy (“disease of many nerves” - Greek) is manifested by many symptoms - from the effect of “running goosebumps” or burning sensation to swelling, sometimes inexplicable attacks of pain, trembling of the limbs, muscle weakness, sweating, shortness of breath, palpitations. Polyneuropathy itself is the result of other diseases, including diabetes, various injuries, and exposure to toxins.
We effectively work with all types of polyneuropathy, preventing its severe consequences - decreased muscle tone, muscle atrophy, loss of a person’s ability to move independently, and self-care.
Given the complexity of this neurological disease, patients require extensive rehabilitation along with basic treatment, which begins with consultation and examination by an experienced neurologist.
After assessing reflexes, muscle tone, limb mobility and analyzing information about concomitant diseases, he will select a personal rehabilitation program for you.
Also, experienced professionals - physical therapy doctors, physiotherapists, massage therapists - will work together with neurologists to solve your health problem.
Using a unique and powerful electroneurophysiological station, specialists will not only conduct an initial diagnosis, but will also evaluate all changes in the functional state of the nervous system during the rehabilitation process. The accuracy of this device is such that not a single slightest deviation in the indicators will escape the attention of our specialists.
In our rehabilitation department, we have collected everything necessary for comprehensive rehabilitation aimed at overcoming polyneuropathy - exercise equipment, walking tracks, modern physiotherapeutic complexes. Along with manual massage, during the rehabilitation of patients with polyneuropathy, modern chivamat therapy (massage with a pulsating electrostatic field), modern computer stations for the functional restoration of the limbs (with biofeedback), installations that simulate the support load of the feet, electromyostimulators, installations for magnetic therapy, etc. .P.
“The key to successful recovery from polyneuropathy is continuous, comprehensive rehabilitation with the construction of an individual program under the supervision of a team of professionals.”
— Alexey Alekseevich Kudryashov, head of the neurology department.
Content:
- The essence of the disease
- Causes of leg damage
- Clinical symptoms, examination methods
- Treatment
Alcohol “hits” absolutely all structures of the body. One of the most sensitive is nervous tissue. It is because of its defeat that pathologies arise that, as it may seem, have nothing to do with the nervous system. These include leg failure due to alcoholism.
The essence of the disease
Ethyl alcohol and its metabolites (in particular, acetaldehyde) negatively affect both the neurons themselves and their membrane. In the first case, the function of the cells suffers, in the second the degree of protection deteriorates - they are damaged by pathological factors, and as a result, normal physiological processes in neurons are disrupted.
What category of diseases does leg failure in alcoholism belong to? What is it called according to terminology? Its presence indicates polyneuropathy - multiple damage to peripheral nerve endings.
Please note: Legs fail in every tenth alcoholic, according to other data - in every third. In the “chronicles,” even in the absence of symptoms, disturbances in nerve cells were observed in 9 out of 10 patients.
Males are affected more often.
Causes of leg damage
What is the mechanism of development of alcoholic polyneuropathy? It is caused by a violation of the sheath of the fibers that innervate the structures of the lower extremities. If the shell is absent, then the speed of impulse transmission through the neuron decreases by 5-24 times.
The immediate causes of alcoholic polyneuropathy of the lower extremities are:
- damage to nerve fibers by ethyl alcohol and its metabolite acetaldehyde;
- insufficient blood supply to neurons, which entails a deficiency of oxygen, proteins, fats, carbohydrates, mineral compounds and vitamins;
- lack of vitamin B1 in alcoholics. It, in turn, is provoked by poor nutrition (alcoholics often belong to socially disadvantaged segments of the population), failure of digestive processes and impaired liver function, which are observed in persons who abuse alcohol;
- compression of nerve fibers due to the fact that an alcoholic often sleeps in unnatural positions. If it is prolonged (more than 1 hour), then the blood supply to the nervous tissue is disrupted, it does not receive oxygen and nutrients, and in severe cases it can even become dead.
Foot massage
Basic movements for neuropathy, massage of the lower extremities
- Rub your palms over the ribs of your feet.
- Press the middle of the foot with your fist and help with your palm on the other side.
- Rub the base of your feet with your palms.
- Rotate your foot left and right while holding your heel.
- Rotate the limb left and right
- Use your thumb to massage the sole, pressing with your fingers on the upper side.
- Circular movements of the fingers on the heels.
- We move our thumbs from the heel to the toes along the sole.
- Circular movements of the toes at the top of the foot.
Please note that the massage should be done for about five minutes, and the exercises should be done in short, smooth approaches several times a day.
Clinical symptoms, examination methods
The symptoms of alcoholic neuropathy are as follows:
- pain;
- hypoesthesia (decreased sensitivity of soft tissues);
- weakness in the legs;
- paralysis - inability to move;
- reduction in the volume of the legs;
- decrease in their tone.
The patient constantly complains that his feet are cold.
Pain is one of the typical symptoms. Their characteristics are as follows:
- by location - on the back surface of the legs;
- by nature - aching, twisting;
- by severity - depending on the duration and severity of the lesion. The pain becomes more intense, the back of the leg is squeezed;
- by occurrence - first episodic, then constant, intensifying over time.
Violations are also recorded during an objective examination - using physical, instrumental and laboratory methods.
Physical examination consists of inspection and palpation (palpation).
Upon examination the following is revealed:
- swelling of the lower extremities;
- pallor or bluishness of the skin;
- dark areas on the skin are the result of the accumulation of melanin pigment.
On palpation:
- detect increased sweating (usually in the feet);
- confirm the presence of edema;
- identify soreness of the calf muscles (they are located on the back of the lower leg).
An objective examination also reveals a violation of tendon reflexes.
Instrumental methods are used to carry out differential diagnosis with other diseases whose clinical picture is similar to the disease being described. Conducted:
- ultrasound examination of the vessels of the lower extremities;
- angiography;
- CT angiography (computed tomography combined with angiography)
and others.
Laboratory methods are less informative in identifying and assessing alcoholic polyneuropathy, but they can complement the overall diagnostic picture. At the same time, they do a general blood test, a blood sugar test, and others.
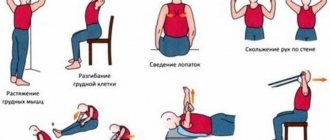
The benefits of exercise therapy for polyneuropathy
To provide effective care to a patient with lower extremity neuropathy, it is important to recognize its symptoms. A characteristic manifestation of the disease is acute nerve pain, which resembles a burning sensation. In some cases, it may not be pain, but a sensation reminiscent of swelling, in which goosebumps begin to run in the form of tingling.
With a progressive form of neuropathy, atrophy of the lower muscles and increased weakness of the lower extremities are possible. When such symptoms appear, it becomes difficult for a person to move and his gait changes. In the most complicated cases of polyneuropathy, muscle spasms, cramps and paralysis can be observed, and both legs can be paralyzed at once.
Studies have shown that exercise therapy for polyneuropathy can improve the condition of muscle tissue and eliminate unpleasant symptoms in the form of pain. In addition, performing special exercises has a positive effect on sugar levels in the human body.
Treatment
What kind of intervention does leg failure in alcoholism require? Alcoholic polyneuropathy is treated on an outpatient or inpatient basis. The main principles of treatment are:
- refusal of alcohol;
- good nutrition;
- drug therapy;
- physiotherapy.
is based on the use of drugs such as:
- vitamins;
- antidepressants;
- anticonvulsants;
- antioxidants.
If a patient experiences leg failure, it is extremely important to use B vitamins - B1 in combination with B6 or B12. They stimulate processes as a result of which nerve fibers are restored. As a result, the normal structure of neurons is restored, impulses are transmitted through them without delay, and fiber nutrition improves.
After treatment, the patient undergoes a rehabilitation course. In this case, the following are involved:
- massage;
- acupuncture;
- electrophoresis;
- magnetic therapy;
- mud therapy - it is carried out in the form of mud wraps or applications;
- contrast baths;
- hyperbaric oxygen therapy;
- physical activity. Physical therapy and swimming are effective.
According to indications, sanatorium-resort treatment is prescribed in specialized sanatoriums.
Since the nerve tissue is affected, treatment takes a long time. Its success depends on whether the patient has stopped drinking alcohol. Therefore, it is of great importance to rid him of alcohol addiction. This will require the intervention of highly qualified specialists who successfully practice in addiction medicine.
Since patients often seek help late, it is not possible to cure alcoholic neuropathy, and disability occurs.
DISEASE OF MANY NERVES: WHAT YOU NEED TO KNOW ABOUT IT
Anna Borisovna, what is polyneuropathy and how common is this disease? — From Greek, the name of this disease is translated as “disease of many nerves.” This very accurately defines the essence of the disease. After all, polyneuropathy is a pathological process that represents multiple lesions of the peripheral nervous system.
The disease occurs frequently. Thus, according to European registers, the overall prevalence of peripheral neuropathies in populations averages 2,400 per 100 thousand, and among elderly people reaches 8,000 per 100 thousand people. The primary incidence of neuropathies usually does not exceed 40 cases per 100 thousand per year.
In Russia, the diagnosis of “polyneuropathy” is made in at least 60% of patients with signs of damage to the peripheral nervous system.
How does this disease manifest itself? — Clinical manifestations of polyneuropathy are usually diverse and have varying degrees of severity.
Many patients complain of weakness of the upper and lower extremities, difficulty breathing, and some have difficulty chewing and speaking.
A frequent manifestation of polyneuropathy is disturbances in urination (especially often in the form of urinary incontinence), erection and digestion in the form of constipation.
Decreased sensitivity and discomfort in the limbs in the form of pins and needles, burning and swelling can also be symptoms of polyneuropathy.
Often patients are bothered by a number of vegetative symptoms. For example, orthostatic hypotension. It manifests itself as a sharp decrease in pressure when changing body position. Naturally, this immediately causes weakness and dizziness, even to the point of fainting.
Also with polyneuropathy, there is trembling of the fingers, involuntary muscle twitching, pallor and sweating, which does not depend on temperature and physical effort, shortness of breath, rapid heartbeat accompanied by arrhythmia, impaired coordination of movements and even slow healing of wounds.
Are there any painful sensations? — Pain due to polyneuropathy is a classic example of neuropathic pain syndrome. And this pain is not associated with a malfunction of any organ. It manifests itself against the background of damage to the nerve fibers of certain parts of the central or peripheral nervous system. Because of this, incorrect signals are sent to pain centers. A clear example of neuropathic pain is phantom syndrome. This condition is characterized by the fact that the amputated limb continues to hurt.
Neuropathic pain always causes persistent and very intense pain. And at the same time, it is practically not relieved by traditional analgesic medications. Such persistence of neuropathic pain naturally causes a lot of negative emotions in patients. Periodically recurring attacks become so painful that they provoke emotional imbalance and depression. There are often cases when polyneuropathy leads to partial loss of ability to work and even disability.
Are the causes of polyneuropathy known? — Based on their occurrence, there are seven main groups of neuropathies:
- Inflammatory and infectious polyneuropathies. They occur against the background of diphtheria, HIV or other diseases.
- Toxic polyneuropathy - most often are the consequences of chronic poisoning with alcoholic beverages, chemical compounds, incl. household, and even medications, if they are used for other purposes.
- Post-traumatic polyneuropathy. First, damage occurs due to cuts, bruises and fractures. Then scar processes occur in the area of wound healing, which compress the nerves.
- Hereditary polyneuropathies (Charcot-Marie-Tooth polyneuropathy, etc.) are systemic diseases that are characterized by damage to several organ structures.
- Autoimmune polyneuropathies are formed against the background of autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, etc.
- Diabetic polyneuropathy of the lower extremities occurs in people suffering from diabetes mellitus for a long period of time.
- Paraneoplastic polyneuropathy. This diagnosis is made against the background of an existing cancer of any location.
Which doctor and for what symptoms should you contact? — At the first manifestations of sensitivity disorders, pain and weakness in the limbs, you should contact a neurologist or neurologist-algologist. Let me remind you that an algologist is a specialist who studies and, above all, treats pain and pain syndromes. This area of medicine is still relatively young, but pain treatment centers are already operating in a number of clinics.
What diagnostic methods are used? — The examination plan is always drawn up individually depending on the specific clinical case. But in any case, the examination of a patient with polyneuropathy begins with a consultation with a neurologist, during which the doctor analyzes complaints and collects an anamnesis of the disease, assesses the neurological status.
The main method of instrumental diagnosis of peripheral nerve damage is electroneuromyography . Using this method, the fact of nerve damage is not only confirmed, but its nature is also determined.
In complex diagnostic cases, the doctor may recommend ultrasound of peripheral nerves, MRI of the plexuses, diagnostic lumbar puncture, morphological examination of the nerve (biopsy) , etc.
To clarify the reasons that caused widespread damage to peripheral nerves, a thorough examination is necessary, incl. comprehensive laboratory blood test (general and biochemical blood test, study of hormones, vitamins, etc.).
If hereditary polyneuropathy is suspected, molecular genetic analysis and consultation with a geneticist are necessary.
Also, to identify the underlying disease, which can cause damage to peripheral nerves, an instrumental general somatic examination , incl. cancer screening (CT lung, ultrasound of the mammary glands, mammography, ultrasound of the prostate and scrotum, esophagogastroduodenoscopy of the digestive system, colonoscopy, ultrasound of the abdominal and pelvic organs, etc.).
What treatment is given? — Only comprehensive treatment can help cope with polyneuropathy. It should include therapy for the underlying disease, auxiliary drug symptomatic therapy with drugs of various groups and non-drug treatment methods (physiotherapeutic treatment, physical therapy, reflexology, balneotherapy, psychotherapy, etc.). This approach in practice makes it possible to achieve highly effective treatment.
In modern neurology, based on many years of experience, treatment for the painful form of peripheral polyneuropathy has been developed. In particular, along with drug therapy, the possibilities of non-drug treatment methods are widely used. transcranial magnetic stimulation and cognitive behavioral therapy have proven to be the best , followed by exercise therapy .
What is transcranial magnetic stimulation? — Transcranial magnetic stimulation is used in the treatment of neuropathic pain syndrome. This procedure is based on the rhythmic effect of a magnetic field on the peripheral nervous system. It allows you to achieve positive health results completely painlessly. Magnetic influence is carried out using alternating current, it affects the cerebral cortex, after which it affects the central nervous system.
What treatment methods are used in pain centers? — The multidisciplinary team of specialists at pain treatment centers also have other methods of rehabilitation treatment in their arsenal: magnetic therapy, electrotherapy, massage in an electrostatic field, breathing exercises, oxygen inhalation, dry carbon dioxide bath, hyperbaric oxygen therapy (a method of saturating the patient with oxygen under high pressure in hyperbaric chambers). hyperbaric chambers), aromatherapy.
It is good when the treatment of a patient with chronic neuropathic pain syndrome is divided into three stages.
- The first stage begins with a consultation with a neurologist-algologist, who conducts a comprehensive diagnosis and identifies the cause of pain, makes a diagnosis and prescribes drug and non-drug therapy, and, if necessary, refers rehabilitation specialists (physiotherapist, physical therapy doctor, reflexologist) to consultations.
- In addition to the first stage of treatment, the neurologist-algologist determines indications and contraindications for the second stage of treatment using interventional methods. This is local drug injection therapy (therapeutic and diagnostic blockades), which are performed together with an anesthesiologist-resuscitator.
- The third stage could be spinal neurostimulation. It is carried out using a small device - an electrical pulse generator, which is implanted subcutaneously in the spinal cord.
Is it possible to use folk remedies for polyneuropathy? - Definitely, “No”! At the first symptoms, a consultation with a neurologist is necessary to prescribe a comprehensive examination to identify the causes of polyneuropathy and prescribe further therapy.
Will lifestyle changes help? - Yes, sure. After identifying the main cause of polyneuropathy, the attending physician will give recommendations for lifestyle correction depending on the underlying disease.
What can be recommended as prevention? — Prevention is possible for some diseases that may be complicated by polyneuropathy. For example, diabetes. Adequate blood glucose control will reduce the risk of diabetic polyneuropathy or slow its progression.
What consequences and complications do polyneuropathy lead to? — It depends on the type of polyneuropathy and the disease that causes it. Sometimes the consequence of polyneuropathy is complete paralysis of the limbs or respiratory organs. In addition, progressive polyneuropathy causes excruciating pain and severe sensory disturbances. People lose the ability to walk and care for themselves; the resulting helplessness, in turn, leads to anxiety and depression. The functioning of internal organs may also be disrupted.
But all this can be avoided if treatment is started in a timely manner.
Can polyneuropathy become a trigger for other diseases? — Most often, damage to peripheral nerves is itself a consequence of the serious diseases described above. But polyneuropathy can also become a provocateur. For example, psychosomatic manifestations. In addition, pain syndrome, which often occurs against the background of damage to peripheral nerves, can negatively affect the condition of the cardiovascular system.
What mistakes do patients who have signs of polyneuropathy make? — The biggest mistake is that many do not pay attention to the first manifestations of the disease (numbness, tingling, etc.), but come to a specialist already in the advanced stage of the disease, when excruciating pain begins to bother them. But it’s no secret that it’s easier to cope with any illness at the very beginning of its development.
How important is treatment adherence? - Extremely important! Often, an adequate analgesic effect can only be achieved with a combination of drugs for the treatment of chronic neuropathic pain. This requires the neurologist-algologist to be highly qualified to select the dose and monitor this treatment regimen, and for the patient to strictly adhere to the doctor’s prescriptions.
Can COVID-19 cause polyneuropathy? — As with any other severe viral infection, COVID-19 can affect the peripheral nervous system. Although, of course, at the moment there is not enough information about the coronavirus and no hasty conclusions can be drawn. It is possible that the appearance of polyneuropathy during the treatment of COVID-19 is also caused by the toxic effects of drugs used in therapy.
Well, those who already have a history of “polyneuropathy” need to be especially careful in protecting themselves from possible infection.
Literature:
- Basic polyneuropathies: Guillain-Barre syndrome, CIDP, alcoholic, diabetic and other polyneuropathies: textbook / Kodintsev A. N., Volkova L. I., Oshurkov P. A. [et al.]; Federal State Budgetary Educational Institution of Higher Education "Ural State Medical University" of the Ministry of Health of the Russian Federation, Department of Nervous Diseases, Neurosurgery and Medical Genetics, MAU City Clinical Hospital No. 40, Yekaterinburg, Medico-Pharmaceutical. — Ekaterinburg: LLC “Tip. For you", 2019. - 64 p.
- Classical neurology: a guide to the peripheral nervous system and chronic pain syndromes / Silantiev Konstantin. - Volgograd: Panorama, 2006 (Volzhsky: Alliance Yugpoligraphkombinat, Volzhsky polygraphkombinat). — 399 p.
- Private neurology: a textbook for students of medical universities / [G. O. Andreeva and others] ; edited by M. M. Same. — Moscow: Med. information agency (MIA), 2009. – 574 p.