INFLUENCE OF EXERCISES ON CHILDREN’S HEALTH
Therapeutic exercise has a positive effect on the body, muscles begin to work, tissues become stronger. During exercise, metabolic processes are regulated, the functioning of the brain and cardiac system improves.
The treatment course for cerebral palsy should include:
- Massage;
- exercise therapy;
- Manual therapy;
- Hardening.
The program is developed for each child on an individual basis. Activities such as: playing with a ball must be present; relaxation exercises; in a sitting and lying position. Stimulating exercises are also carried out.
Positioning Goals
Children with cerebral palsy require external postural support (positioning) in a variety of positions. This allows them to develop more normal ways of moving and avoid secondary complications. This widespread practice is based on clinical and research evidence.
Positioning goals include:
- Normalization of tone or reduction of its abnormal effects on the human body.
- Maintaining correct body position in space.
- Prevention or elimination of bone deformities.
- Providing a basis for the implementation of functions.
- Promoting increased tolerance for the desired situation.
- Providing comfort and relaxation.
- Promoting normal movement patterns or managing abnormal movement patterns.
- Preventing the development of bedsores.
- Reduced fatigue.
- Improving the functioning of the autonomic nervous system (control of the functioning of the cardiac, digestive and respiratory systems).
- Promoting maximum functionality with minimal pathology.
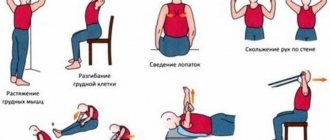
COMPLEXES OF EXERCISES
Exercise therapy programs for children with cerebral palsy include activities such as:
- Position. Fixing legs and arms in splints;
- Muscle stretching. Swinging of legs and arms with gradual acceleration;
- Muscle relaxation. Fixing the limbs one by one. As a result, the increased tone is weakened and the number of involuntary movements and twitches decreases;
- Walking;
- Flexion and extension of joints with simultaneous muscle massaging;
- Climbing along an inclined surface (instructor helps). The exercise trains the child’s abs and legs and teaches the body well to maintain balance;
- Endurance training.
When diagnosed with spastic diplegia, exercises should be accompanied by continuous movement.
THE ROLE OF MASSAGE IN MEDICINE
Massage for cerebral palsy in children is used as an assistant, but not the main treatment. This is an important element in exercise therapy for children, helping to normalize blood flow, normalize metabolic processes, and relieve spasms. There are 3 types of massage to treat the musculoskeletal system:
- Classic
- Segmental
- Spot.
After familiarizing yourself with each method in the exercise therapy program, the baby’s parents can do it themselves at home. This massage is also taught in courses.
Basically, there are several manipulations that have a beneficial effect on the child’s body.
- Stroking without interruptions – relaxes the muscles;
- Felting – affects large areas;
- Skating is effective for the hip and shoulder joints;
- Intermittent stroking – maintains tone;
- Rubbing with the “outer” palm – stimulates the muscles on the back, buttocks, and thighs;
- Effleurage.
Children with cerebral palsy constantly undergo rehabilitation courses, using different methods in different centers. How are they different from each other? While understanding the methods of rehabilitation of cerebral palsy, Miloserdie.ru correspondent Sofya Bakaleeva collected so much material that it did not fit into one article.
The methods presented here are only tools for the rehabilitation and adaptation of a child with cerebral palsy. It is important that they fall into the hands of a competent specialist. In the hands of a professional rehabilitation therapist who understands his competence and takes into account and respects the interests of his patient, all these techniques become a way to give the patient with cerebral palsy sometimes independence, sometimes freedom of movement, but always self-confidence.
The main thing: every intervention, every new round of rehabilitation must have a goal. Not distant and not abstract - “to be healthy” or “to be like everyone else.”
Let's look at the right column and see the abbreviation - SMART (“smart”). The concept of SMART goals has long been used in business and in private life to solve specific problems, including in rehabilitation. It has proven its effectiveness.
1) Physical therapy (not to be confused with physiotherapy)
Age: any
Author: The first mention of the effective use of massage, manipulative techniques and gymnastics is considered to be 1813, when the father of Swedish gymnastics, Per Henrik Ling, founded the Royal Central Institute of Gymnastics (RCIG). However, the official birthday of the specialty “physical therapist” is considered to be 1894, when four British nurses united in a society to use therapeutic massage and gymnastics in their clinical practice. The World Confederation of Physical Therapy (WCPT) was founded in 1951 and today has 106 member countries.
What it is based on: the method is based on a scientific approach and the principles of evidence-based medicine.
Who is it suitable for: patients with a wide variety of diseases and conditions in the field of neurology, traumatology, orthopedics, cardiology, palliative medicine, with a very different course and prognosis.
Goal: To restore and maintain a person's ability to move and be independent to the maximum extent possible, develop functional movements, prevent or limit the development of complications such as contractures, deformities, bedsores, help the client control pain and maintain the functions of the respiratory and cardiovascular systems.
Objectives: the focus of physical therapy is movement, and the most active one, which is initiated by the patient himself. Physical therapists consider its restoration and maintenance to be the main goal of their activity. Any of our activities is connected with it, it helps to communicate with people, establish social contacts, and express feelings. In any of our movements, physical, social and psychological factors are inextricably intertwined.
The essence of the method: physical therapists use physical (natural) methods of influence on the client, based on movement, manual influence, massage, reflexology and the action of heat, light, high frequencies, ultrasound and water. But he considers mechanical force and movement to be the main ones. The result of the work of a physical therapist is the most active and correct movements, which are planned, initiated and performed by the client (patient) himself within the framework of his motor potential.
Method: the intervention of a physical therapist is:
— specially selected physical exercises: training strength, balance, movement components, etc. taking into account the client’s violations and a number of other factors;
— techniques that help the client perform a particular movement;
— selection and formation of the correct postures (body positions) that alleviate the human condition and/or prevent the occurrence of complications;
— techniques and techniques for properly moving patients;
— selection and adaptation of technical aids for rehabilitation;
— training clients and those who help them (if they have to move the patient) in correct motor behavior.
Principles: Currently, physical therapists, occupational therapists, and many other professionals use what is called a problem-oriented approach. The process consists of the following steps: assessment, intervention planning, the intervention itself, and evaluation of the effectiveness of the intervention.
The physical therapist's work begins with assessing all the client's structures and functions that may affect movement, mobility, and other functionality. Then the specialist, together with the client and/or his loved ones, sets clear and understandable intervention goals for the client and his family members.
Forms of work: a physical therapist participates in the work of an interdisciplinary team, that is, a group of specialists that includes doctors, nurses, speech therapists, psychologists, teachers and other specialists. In each specific case, the team is formed only from those specialists whose help a particular person and/or his family really needs. Team work is based on partnerships between specialists, all decisions are made jointly by them after discussions, but at the same time, each team member bears professional responsibility for their work. In addition to professionals, the team includes the client himself and, quite often, his relatives or other people close to him. Cooperation with the client, members of his family or people from his immediate environment is an essential condition for successful assistance.
Contraindications: no
Duration of the course: there is no idea of course therapy, the intervention is carried out to achieve a specific goal
2) Occupational therapy
Age: any
What it is based on: a scientific approach and the principles of evidence-based medicine. The term "occupational therapy" was adopted as the Russian equivalent of the generally accepted term "Occupation Therapy". As a specialty, occupational therapy was formed after the Second World War, when society was faced with the problem of mass disability of people of working age and the need to rehabilitate them.
Suitable for: anyone who has suffered an illness/injury or who has developmental disabilities from birth and who, for this reason, find themselves dependent on outside help.
Goal: to help restore a person’s ability to live independently to the maximum extent possible.
Objectives: to help people with various physical and mental disabilities actively carry out everyday activities, for example, caring for themselves (dressing, undressing, washing, eating, etc.), participating in productive activities - playing, working, as well as spending leisure time, for example , master hobbies, and thus achieve maximum independence in all aspects of daily life. Occupational therapy also prevents a decrease in the client’s activity, aggravation of disorders and deterioration of his condition.
The essence of the method: Occupational therapists work with clients who, due to their impairments, are limited in areas such as self-care, productive activities and leisure time. They not only analyze the impact of disorders on different types of activities, but also take into account the effect of personal and environmental factors (social, physical, economic) on the functioning of each client in specific situations. In general, the occupational therapist uses those activities that are important to the client and aimed at achieving the highest possible level of functioning, independence in daily life and, therefore, improving the quality of life. For example, for a child these may be the skills of dressing, eating independently, playing, and planning free time.
Method: occupational therapist intervention is:
— specially selected methods of training the client and/or his relatives and people caring for him;
— techniques that help the client complete one or another component of the selected activity;
— techniques for modifying and adapting the task facing the client, facilitating its implementation;
— various techniques for developing and training the functions of the arm and hand;
— techniques and techniques for the correct movement of patients, care and assistance in performing all necessary activities;
— use of various methods of environmental adaptation;
— selection and adaptation of technical rehabilitation aids.
Principles: Problem-based approach: assessment, intervention planning, intervention itself, and evaluation of intervention effectiveness.
The work of an occupational therapist begins with assessing the types of activities that are important and necessary for the client, the quality of their implementation, the client’s current capabilities and analysis of factors that hinder or help to do something effectively, including the features of the environment and the state of all structures and functions of the client. Then the specialist, together with the client and/or his loved ones, outlines specific goals for the intervention.
Forms of work: Occupational therapists work directly with individuals, groups of people or communities, helping them to do what they want, feel compelled or obliged to do, and adapt the activity and/or environment so that people can more effectively carry out worthwhile activities. they have a task ahead of them.
Contraindications: no
Duration of the course: there is no idea of course therapy, the intervention is carried out to achieve a specific goal
3) Bobath therapy
Age: any
Authors: a married couple from London - neurophysiologist Karl Bobath and physiotherapist Bertha Bobath - developed a system of special classes in the 40s of the twentieth century, which was called Bobath therapy. Nowadays, the Bobath concept is implemented as neurodynamic rehabilitation.
What it is based on: the brain’s ability to undergo neuroplasticity in changing environmental conditions, which encourage the improvement of motor behavior. During the existence of the technique, the focus of its application has shifted from trying to influence the restoration of the damaged nervous system to normalizing the patient’s movements. An important discovery was that it is not the muscles, but the brain that controls how the patient performs a movement or is in a static position. This means that the therapist can change the patient’s movements to more correct ones, using some specific sensory stimulation techniques.
Suitable for: people with movement disorders resulting from damage to the central nervous system
Goals: increasing the patient's functional activity, maximizing the efficiency of movement within the patient's capabilities (rather than restoring movement to normal levels), increasing his participation in social life.
Objectives of therapy: stimulation of normal motor development and prevention of contractures and deformities, work with muscle tone to improve the quality of movement.
The essence of the method: Using technologies for controlling and directing the patient's movements with carefully graded stimulation, the therapist strives to give a normal feeling of active movement, which is translated into the sphere of purposeful action. Bobath therapy is a neurodevelopmental therapy that does not have canonical exercises or complexes. Each time it is carried out individually. Bertha Bobath argued that the therapist in this method is obliged to “do what works best.” The therapist seems to “sculpt” the correct movement in his patient and strives for the most normal movement (posture) and maximum independence of the patient.
Method: The therapist combines techniques called sensory stimulation, inhibition and facilitation:
— inhibition is the inhibition of pathological movements, body positions and reflexes that interfere with the development of normal movements;
— facilitation is the facilitation of correct (normal) movements and body positions;
— stimulation is tactile and kinesthetic stimuli necessary for the child to better feel the correct movements and position of his own body in space.
As a result, a person’s usual sensations from movements and static holding of a pose change. And this makes it possible to correct postures and movements.
Principles of motor learning: active participation of the patient, skill training, setting goals that are meaningful to the patient. With Bobath therapy, the physical therapist must include his patient in joint activities, the child must consciously perform this or that action, which excludes a negative reaction on his part. If it is, the therapist’s actions are initially incorrect and cannot lead to any improvements.
Contraindications:
Epilepsy during active seizures
Severe mental disorders
Acute inflammation and febrile conditions
4) Vojta therapy
Age: any
Author: Czech professor of medicine Vaclav Vojta (1917-2000). From 1948 to 1956 he worked at the neurological clinic of Charles University in Prague. Since 1956 - Head of the Department of Child Neurology at the Clinic of the Faculty of Medicine of the University of Prague. In 1961, he was entrusted with the management of the clinic of the Faculty of Child Neurology in Prague. After the entry of troops into Czechoslovakia in August 1968, he found refuge in Germany, at the Orthopedic University Clinic in Cologne. In 1975 he became the head of the rehabilitation department of the Munich Children's Center.
What it’s based on: according to Voight’s theory, if you consolidate movements at the reflex level, the central nervous system will use them, spontaneous motor activity will appear in the form of developed movement, improving ergonomics in general. Professor Vojta theorized that by repeatedly inducing these “reflex-like” movements in the patient, the functionally blocked nerve networks between the brain and bone marrow were “unblocked” or “rewired.”
Who is it suitable for: the method is used to correct disorders in the musculoskeletal system, both in infants and older children. Vojta therapy is especially effective in infants, as they have not yet developed replacement movement patterns. Children aged 5-6 years and older have already developed such models, so experts focus on activating and maintaining physiological motor forms.
Goals: through the use of reflex locomotion, the elementary components of human straightening and movement should become accessible and applicable again, that is:
- body balance during movements (“postural control”),
- straightening the body against gravity,
- purposeful grasping and stepping movements of the limbs (“phasic mobility”).
Objectives: development of motor skills appropriate to the child’s age.
The essence of the method: inducing reflex motor acts (reflexolocomotion) by stimulating certain skin areas with the simultaneous application of a strictly oriented pressure vector. The procedure does not apply to the method of physical therapy. This is not physical training of movements, but an indirect effect on the central nervous system. The brain retains a program of “normal,” physiological movements, rather than learning substitute directions.
Method: the therapist applies pressure to certain areas of the body of a person who is in the initial position lying on his stomach, back or side. Irritations reflexively cause one of two complexes: reflex crawling on the stomach or reflex turning over from a position lying on your back or on your side through a position on your stomach to a standing position on all fours.
Principles: The procedure itself should in no case cause pain or fear. The activated state that therapy is aimed at achieving in infants during the procedure is often expressed in the form of a cry. Screaming is a means of responding to unusual activation in patients of this age. At an older age, when children can express themselves using language, they no longer scream.
Contraindications:
Acute infectious pathology
10 days after vaccination
Problems with the cardiovascular system
Osteogenesis imperfecta, glass bone disease, phosphate diabetes
Exacerbation of other chronic diseases
Convulsions of various origins
The following materials were used in preparing the review:
E.V.Semenova, E.V.Klochkova, A.E. Korshikova-Morozova, A.V. Trukhacheva, E.Yu. Zablotskis. Rehabilitation of children with cerebral palsy. Review of modern approaches to help rehabilitation centers M., 2018
K. A. Semenova Restorative treatment of children with perinatal damage to the nervous system and cerebral palsy M., 2007
https://physrehab.ru website of the ANO “Physical Rehabilitation” https://www.vojta.com website of the International Vojta Society
The review will continue.
Illustrations: Oksana Romanova
Author of the article: Sofia BAKALEEVA
Source: Mercy.ru
Share to VK Share to Facebook Share to Twitter Share to Goodle+
POOL FOR CHILDREN WITH Cerebral Palsy
Children love water and a baby with cerebral palsy is no exception. Water procedures should not last more than 30 minutes. Muscles do not need overwork. Classes should be regular, preferably on the same day. One-time visits to the pool will not bring any results. All exercises in water are carried out gradually, in combination with other elements.
In any exercise therapy program for children with cerebral palsy, there is a lesson on interaction with water. Tactile sensation is important because babies learn new things.