Symptoms and treatment of tick-borne encephalitis
Tick-borne encephalitis is seasonal and appears only in the spring-summer period - the time of activation of tick activity. The carrier lives in grass and treetops, has very low mobility and does not have the ability to pursue its prey.
The tick clings to a person or animal located in close proximity to it and parasitizes on it for several days. They choose the least noticeable place for attachment - axillary and inguinal folds, knee bends, head, neck, so detecting a tick in the first days is very difficult. It can be detected several days later, after it increases in size several dozen times.
The ixodid tick itself is not a source of the virus - it becomes infected with it from sick animals. The total number of infected ticks is approximately 20%, so an arthropod bite does not always lead to infection.
What it is?
Tick-borne encephalitis (spring-summer tick-borne meningoencephalitis) is a natural focal viral infection characterized by fever, intoxication and damage to the gray matter of the brain (encephalitis) and/or the membranes of the brain and spinal cord (meningitis and meningoencephalitis). The disease can lead to persistent neurological and psychiatric complications and even death of the patient.
According to statistics, six ticks out of a hundred are carriers of the virus (at the same time, from 2 to 6% of people bitten can get sick from an infected individual).
How does infection occur?
The main reservoir and source of infection are ixodid ticks. How does the tick-borne encephalitis virus enter the insect's body? 5–6 days after the bite of an infected animal in a natural outbreak, the pathogen penetrates all organs of the tick and concentrates mainly in the reproductive and digestive systems, and the salivary glands. The virus remains there for the entire life cycle of the insect, which is from two to four years. And all this time, after a tick bites an animal or person, tick-borne encephalitis is transmitted.
Absolutely every resident of an area where there are outbreaks of infection can become infected. These statistics are disappointing for humans.
- Any animal can be a natural reservoir of infection: hedgehogs, moles, chipmunks, squirrels and voles and about 130 other species of mammals.
- Depending on the region, the number of infected ticks ranges from 1–3% to 15–20%.
- Some species of birds are also among the possible carriers - hazel grouse, finches, thrushes.
- According to epidemiology, tick-borne encephalitis is widespread from Central Europe to Eastern Russia.
- The first peak of the disease is recorded in May-June, the second - at the end of summer.
- There are known cases of human infection with tick-borne encephalitis after consuming milk from tick-infected domestic animals.
Routes of transmission of tick-borne encephalitis: transmissible, during a bite by an infected tick, and nutritional - after eating contaminated foods.
Spring “gifts”: borreliosis and encephalitis
Seasonal tick activity increases with rising temperatures and is typically observed between March and November, but peaks in April-May and August-September. Small insects can cause serious diseases - for example, tick-borne viral encephalitis is often very severe, even fatal. At the initial stages of development, it is similar to other dangerous pathologies: tick-borne borreliosis, acute poliomyelitis, serous meningitis. Therefore, early differential diagnosis is vitally important, because it allows you to accurately determine the cause of increasing symptoms. The need to differentiate viral encephalitis and borreliosis is also due to the fact that these two diseases occur in the same regions and they appear after a tick bite.
What to do if you are bitten by a tick?
- Remove the tick as quickly as possible . You can do this yourself or go to a surgery/emergency room/otolaryngologist if the tick is in the ear.
- Examine the tick for borreliosis . Deliver the tick to the DILA laboratory and find out whether it was a carrier of Borrelia burgdorferi sensu lato infection.
- Get yourself tested for borreliosis . The study is carried out to identify damage to the body by the causative agent of Lyme disease - Borrelia, or to ensure the absence of the disease.
If the DNA test result of the tick is positive, this means that the insect was infected with the causative agent of borreliosis. You should immediately contact your family doctor or infectious disease specialist, who will prescribe emergency prevention - it is most effective within the first 5 days after the tick is detected.
An antibody test is recommended to be carried out 2-4 weeks after the bite if DNA testing of the tick has not been performed or it turns out that the insect was a carrier of Borrelia. If the result is positive or doubtful, you should immediately consult a doctor: if treatment is not started in the early stages, the disease can affect the skin, joints, muscles, nervous system and heart.
What is borreliosis and tick-borne encephalitis?
Among the many diseases that ticks carry, you can become infected with two without leaving Ukraine – tick-borne encephalitis and borreliosis (Lyme disease). These infectious diseases are often confused, although they are completely different. Tick-borne encephalitis is caused by a virus, and borreliosis is caused by bacteria. Both diseases lead to damage to the central nervous system, but Lyme disease also affects the joints, heart muscle, and skin. And, if the course of encephalitis is predominantly acute, then borreliosis occurs in a chronic form. After encephalitis, stable and long-lasting immunity remains, while Lyme disease causes a slowed immune response of the body with a cascade development of autoimmune reactions, so re-infection is possible after 7 years. As each disease develops, it is accompanied by its own distinct clinical manifestations.
Every year more than 2 thousand new cases of Lyme disease are recorded in Ukraine. It is diagnosed mainly in adolescents and young people under 45 years of age. Tick-borne encephalitis is less common, with 569 cases identified between 1955 and 2008. Therefore, the most pressing problem for our country is borreliosis.
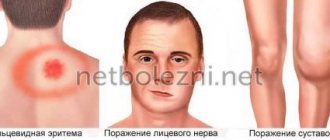
Borreliosis (Lyme disease)
Borreliosis is the most common tick-borne disease caused by spirochetes (spiral-shaped bacteria). Three species of these gram-negative spirochetes are common in Ukraine - Borrelia afzelii, Borrelia burgdorferi and Borrelia garinii. Immediately after entering the body, borrelia are attacked by the immune system, so they quickly “go” to places where immune activity is not so high - in the heart, tendons, and nerve tissues. It is for this reason that Lyme disease, unlike viral encephalitis, often does not have an acute stage. The main symptom is migratory ring-shaped erythema - a bright red spot at the site of the tick bite, which slowly grows, forming a ring. Peeling of the skin begins and necrosis occurs. It is also possible that secondary allergic erythema may appear on other parts of the body. The disease can also occur without skin lesions, but with fever and intoxication.
They carry spirochete-like bacteria, including Borrelia and ixodid ticks, which also spread encephalitis. Of the entire population of these arthropods, only 0.5-4% are carriers of the virus, and 15-20% are carriers of Borrelia. In the case of borreliosis, the pathogen does not live in the insect’s saliva, but in the digestive system, so infection does not occur immediately after the bite. This gives a certain amount of time - if you remove the tick correctly, there is a high chance of not getting sick. If infection does occur, borreliosis is also treatable. The main thing is to prevent the disease from progressing to the disseminated (widespread, scattered) or chronic stage. Patients are prescribed antibacterial drugs, the use of which practically guarantees complete recovery.
The symptomatic picture of borreliosis depends on the stage of the disease.
Stage I (early local infection) . The primary manifestation of infection is erythema migrans around the bite site. The redness is accompanied by general flu-like symptoms such as fever, chills, headache and vomiting. Sometimes lymphadenopathy (benign cutaneous lymphadenosis) may occur. The outcome of stage I can be either spontaneous recovery or the development of the disease into a generalized form.
Stage II (early disseminated borreliosis). The second stage is characterized by damage to the nervous system (in the form of serous meningitis, neuritis of the cranial nerves, radiculoneuritis), and the cardiovascular system (myocarditis, pericarditis). Mild manifestations of irritation of the meninges may appear early, when erythema is still present, and pronounced neurological symptoms often appear several weeks after infection, when erythema, a marker of tick-borne borreliosis, has already passed. Approximately 30% of patients exhibit moderate manifestations in the form of insomnia, decreased concentration, memory impairment, increased excitability, and emotional disorders.
Stage III (late chronic borreliosis). At this stage, the joints are affected. It begins 2 months after the onset of the disease and later, sometimes after 1-2 years. The disease often affects large joints, especially the knees. Sometimes arthritis appears, relapsing over several years and becoming chronic; it can progress to the destruction of bone and cartilage tissue.
The chronic stage of Lyme disease occurs with alternating periods of remission and relapse. Lesions of the skin (atrophic acrodermatitis - cyanotic-red spots on the elbows and knees), nervous system (chronic encephalomyelitis and polyneuropathy) and psyche (insomnia, speech disorders, memory impairment) are observed. Long-term and chronic course of borreliosis sometimes leads to partial or complete loss of ability to work.
Lyme disease is not transmitted from person to person, however, transplacental transmission is possible: through the placenta from a pregnant woman to the fetus. This explains the fact that the disease is periodically detected in infants.
Tick-borne encephalitis
Tick-borne encephalitis is a viral disease that affects the central and peripheral nervous system. Severe complications of an acute infection can result in paralysis and even death. As a viral infection develops, it leads to gradual, often irreversible changes in the blood vessels and membranes of the brain. During the first 14 days the disease occurs without pronounced symptoms, by the 20th day the following appear:
- heat;
- headache;
- nausea;
- loss of appetite;
- muscle pain.
In approximately 25% of patients, these manifestations occur even later – a month after infection. As the disease progresses, the pain intensifies. Convulsions, paralysis of the limbs, disorientation in space, loss of consciousness, and coma occur. If left untreated, it will be fatal. Tick-borne encephalitis in general is also treatable, but in this case the list of drugs and methods is much wider.
Important! An undoubted feature that unites tick-borne borreliosis and encephalitis is the importance of prompt diagnosis. Both of these diseases cannot be underestimated - they lead to serious complications that can cause disability and even death. A test for borreliosis is prescribed when a tick is detected and to assess the effectiveness of treatment if the disease does occur. Laboratory diagnostics makes it possible to exclude the disease with lesions of the skin, nervous system and heart, and with arthritis of unknown etiology.
Features of laboratory diagnostics
It is not easy to detect the causative agent of tick-borne borreliosis in the body. Borrelia are present in the affected tissue or in liquid - for example, on the skin at the edges of erythema or in the cerebrospinal fluid, but the effectiveness of such studies is low. The simplest and most accurate diagnostic method is serological tests. Venous blood is taken from the patient and tested for the presence of antibodies to the spirochete.
The following studies are available in DILA:
- Borreliosis, Borrelia, IgM antibodies. Class M immunoglobulins (IgM) appear in the blood first (1-3 days after infection), but they can be detected at a later date - after 2-3 weeks. After approximately 6 weeks, these antibodies reach a maximum and then slowly decline. IgM immunoglobulins are best suited to diagnose recent infection. If the result is positive or questionable, then another study needs to be performed - Western blotting (immunoblot).
- Borreliosis, Borrelia, IgG antibodies. They can be detected in the blood a few weeks after infection, and they reach their peak after 4-6 months. Thus, immunoglobulins G are suitable for later diagnosis of tick-borne borreliosis. In doubtful cases, immunoblotting is used to confirm the results of ELISA studies.
- Borreliosis, IgM/IgG screening (immunoblot for doubtful/positive). A screening study aimed at confirming infection in case of a positive or doubtful result.
- Examination of a tick for borreliosis, Borrelia burgdorferi, PCR - quality. Examination of a tick makes it possible to detect DNA fragments of the causative agent of the disease in the tick. The insect is delivered to the laboratory immediately after extraction in a test tube or container for biomaterials. It does not matter whether the tick is alive or dead.
Determining antibodies is the main way to confirm the diagnosis, but it is important to carry it out at the right time. The accuracy of the study is 95%, the number of false positive results does not exceed 5%. To exclude errors or confirm the diagnosis, an immunoblot is prescribed - this study increases the accuracy of diagnosis in patients with symptoms of Lyme disease, but with negative immunoassay results.
Studies are most revealing two weeks after infection. First, IgM antibodies are detected in the blood, then IgG. They reach peak concentrations after 3 months. It is impossible to detect borreliosis based on one study - the process of disease development is too complex, so no single method can be called exclusive. If negative results are obtained, it is recommended to repeat the test after a few weeks, since in the early stages of the disease, half of the patients have a low level of antibodies, which does not exclude infection.
In parallel with examining the tick for borreliosis and immunoassay, it would not be amiss to donate blood for encephalitis, because ticks can be carriers of both diseases at the same time.
If you find a tick on your body, you need to immediately conduct laboratory tests of the biomaterial, and if the result is positive, take emergency measures within the next 5 days after the insect bite by contacting an infectious disease specialist or therapist. Treatment in the early stages can shorten the duration of the disease and associated symptoms. Antibacterial therapy during the incubation period in the early stages (up to 5 days after tick ingestion) makes it possible to prevent the development of the infectious process in almost all patients. In addition, timely treatment will help prevent the progression of the disease and the development of late, prognostically unfavorable stages.
Other news
08.10.2021
Dila's work schedule on holidays
06.10.2021
Important information for clients of the branch in Kiev at 15 Goloseevsky Avenue
06.10.2021
Allergy to mold
0 0
Forms of the disease
Symptoms after an encephalitis tick attack are very diverse, but in each patient the period of the disease traditionally proceeds with several pronounced signs.
In accordance with this, there are several main forms of tick-borne encephalitis:
- Feverish. The tick-borne encephalitis virus does not affect the central nervous system; only symptoms of fever appear, namely high temperature, weakness and body aches, loss of appetite, headache and nausea. Fever can last up to 10 days. The cerebrospinal fluid does not change, there are no symptoms of damage to the nervous system. The prognosis is most favorable.
- Meningoencephalitic. It is characterized by damage to brain cells, which are characterized by impaired consciousness, mental disorders, convulsions, weakness in the limbs, and paralysis.
- Meningeal. The virus penetrates the meninges, infecting neurons. In this case, a focal form of the disease develops. In addition to fever, symptoms of encephalitis include severe headache, vomiting, and photophobia. Signs of involvement of the meninges in the inflammatory process develop—stiff neck muscles. When performing a lumbar puncture in the cerebrospinal fluid, you can see signs of inflammation: plasma cells appear, the level of chlorides decreases, etc.
- Poliomyelitis. It is characterized by damage to the neurons of the cervical spinal cord and resembles polio in appearance. The patient has persistent paralysis of the muscles of the neck and arms, which leads to disability.
A special form of tick-borne infection has a two-wave course. The first period of the disease is characterized by febrile symptoms and lasts 3–7 days. The virus then penetrates the meninges and neurological signs appear. The second period lasts about two weeks and is much more severe than the febrile phase.
Monoritis ehrlichiosis of man
a tick-borne infection that affects the liver, skin, central nervous system, and bone marrow. It is difficult to make an accurate diagnosis due to nonspecific symptoms. The incubation period is 1-29 days, with an average of 13 days.
Symptoms:
- Increase in temperature to 38-40°, chills;
- Headache;
- Weakness, malaise;
- Joint and muscle aches;
- Sore throat, dry cough, nasal congestion.
The disease is characterized by the formation of ulcerative rashes and enlargement of the liver. It is more often diagnosed in children and adults over 40 years of age.
Tick-borne encephalitis - symptoms
The incubation period for transmissible transmission lasts 7-14 days, for nutritional transmission - 4-7 days.
The Far Eastern subtype of tick-borne encephalitis is characterized by a rapid course with high mortality. The disease begins with a sharp increase in body temperature to 38-39 ° C, severe headaches, sleep disturbances, and nausea begin. After 3-5 days, damage to the nervous system develops.
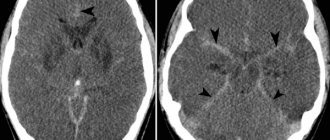
The clinical picture of symptoms of tick-borne encephalitis of the European subtype is characterized by biphasic fever. The first phase lasts 2-4 days, it corresponds to the viremic phase. This stage is accompanied by nonspecific symptoms, including fever, malaise, anorexia, muscle pain, headache, nausea and/or vomiting. Then comes an eight-day remission, after which in 20-30% of patients there follows a second phase, accompanied by damage to the central nervous system, including meningitis (fever, severe headache, stiff neck) and/or encephalitis (various disturbances of consciousness, sensitivity disorders, motor disorders up to paralysis).
In the first phase, leukopenia and thrombocytopenia are detected in the laboratory. A moderate increase in liver enzymes (ALT, AST) in a biochemical blood test is possible. In the second phase, pronounced leukocytosis is usually observed in the blood and cerebrospinal fluid. The tick-borne encephalitis virus can be detected in the blood starting from the first phase of the disease. In practice, the diagnosis is confirmed by the detection of specific acute-phase IgM antibodies in the blood or cerebrospinal fluid, which are detected in the second phase.
Tick-borne borreliosis (Lyme disease)
the most common disease carried by ticks. It is transmitted to humans through the saliva of an infected ixodid tick during a bite. It is characterized by a long-term chronic course with damage to several body systems. The incubation period is from 2 to 35 days, on average 14 days.
The initial stages of the disease proceed similarly to other diseases, so it is quite difficult to recognize borreliosis. In this regard, we again return to the importance of laboratory examination of the attached tick.
Symptoms:
- Redness of the skin at the site of the bite up to 10-20 cm;
- Temperature rises to 38-39°;
- Headache;
- Pain in muscles and joints;
- Vomiting, nausea;
- Enlarged lymph nodes;
- Sore throat, runny nose (in rare cases).
Early diagnosis of the disease and timely measures taken to stop it can prevent the development of later stages. If time is missed, the infection spreads through the blood to various internal organs and causes inflammation.
Possible consequences include damage to systems and important functions of the body:
- Nervous system;
- Lymphatic system;
- Joints;
- Heart;
- Spleen;
- Leather;
- Eyes ears.
After the necessary treatment, you can donate blood for borreliosis. The analysis determines whether infection occurred from a bitten tick and whether the therapy helped get rid of the pathogen. Such blood samples are taken 20 days after the onset of the disease or 30-40 days after the bite.
What should I do if bitten by a tick?
If a tick has embedded itself in a person's skin, it should be removed in a medical facility. It is not recommended to do this on your own, as you can damage its body and not remove it completely. If there are no hospitals nearby, but you urgently need to remove a tick, you need to do the following:
- the skin is generously lubricated with Vaseline or oil (to stop the flow of oxygen to the tick)
- then it is grabbed with tweezers and carefully rotated counterclockwise and removed from the human skin
- after extraction, it is necessary to go to the hospital on the first day after the bite for vaccination - specific donor immunoglobulin is injected intramuscularly, 3 ml.
Diagnostics
Tick-borne encephalitis can be suspected in the case of trips to nature in endemic areas, with tick bites, in the presence of fever, headache, and neurological symptoms. But the clinic does not make a diagnosis.
To accurately confirm the diagnosis, it is necessary to determine specific antibodies -
- immunoglobulin class M for encephalitis (IgM) – the presence indicates an acute infection,
- IgG - the presence indicates contact with an infection in the past, or the formation of immunity.
If both types of antibodies are present, this is a current infection.
The virus is also determined in the blood by PCR and PCR of the cerebrospinal fluid is performed. In addition, another infection in the blood is determined in parallel - tick-borne borreliosis.
Relapsing tick-borne typhus
an acute infectious disease transmitted primarily by argasid mites. The duration of the incubation period is 3-16 days.
Symptoms:
- Induration and purple spot at the site of the bite;
- Fever;
- Sharp headaches;
- Insomnia;
- Temperature increase;
- Increased heart rate;
- Rash all over the body.
This disease is characterized by a two-phase course. After a few days, the first wave ends, and the patient’s condition improves. After 2-8 days, symptoms return - the second phase of the disease begins. Therapy is carried out with antibacterial drugs. The main danger of relapsing tick-borne typhus lies in complications: disruption of the liver, spleen, development of acute heart failure.
Tick-borne encephalitis - treatment
All sick people are required to be hospitalized in a hospital. They are shown strict bed rest. Patients should be kept in intensive care wards or under the constant supervision of medical personnel due to the unpredictability of the pathology. If complications develop, patients are transferred to the intensive care unit.
Drug treatment of tick-borne encephalitis is as follows:
- infusion therapy - solutions of glucose, Ringer, Trisol, Sterofundin;
- etiotropic therapy (directly aimed at destroying the pathogen) - specific donor immunoglobulin, homologous donor polyglobulin, leukocyte donor interferon, reaferon, laferon, intron-A, neovir, etc.;
- glucocorticosteroids (methylprednisolone, prednisolone) - drugs in this group prevent damage to the brain and spinal cord, reduce their swelling;
- antipyretic drugs - paracetamol, infulgan. It is forbidden to use acetylsalicylic acid due to possible complications on the liver;
- decongestants – mannitol, furosemide, l-lysine escinate;
- anticonvulsant therapy – sodium hydroxybutyrate, magnesium sulfate, sibazon;
- substances that improve microcirculation in the brain - thiotriazoline, trental, dipyridamole, actovegin;
- neurotrophics – complex B vitamins (neurorubin, milgamma);
- hyperbaric oxygenation.
During the recovery period, exercise therapy procedures, therapeutic massage, and classes with a rehabilitator are indicated.
Features of the use of immunoglobulin
As for the use of immunoglobulin against tick-borne encephalitis, its administration is considered as an emergency prevention drug, immediately after a parasite bite. It provides protection against the development of the disease, or contributes to its easy tolerance.
The drug interrupts the cycle of viral development in the initial route of infection and prevents its reproduction. The antigenic structures of immunoglobulin recognize the virus, bind antigen molecules and neutralize them (0.1 g of serum can neutralize about 60,000 lethal viral doses).
The effectiveness of the drug has been proven when administered within the first 24 hours after a tick bite. Further, its effectiveness drops sharply, since with prolonged exposure to the virus, the cells of the body are already affected, and cell walls are an insurmountable barrier for our molecular guardians.
If more than 4 days have passed after contact with a tick, it is dangerous to administer the drug throughout the entire incubation period of the virus; this will only complicate the disease and will not prevent its development.
Babesiosis
an acute infectious disease that occurs with fever, jaundice, and anemia. The causative agents are protozoa of the genus Babesia. The incubation period is 10-15 days.
Characteristic symptoms:
- Temperature rise up to 40°;
- Increased sweating;
- Weakness, fatigue;
- Increased size of the liver and spleen.
In humans, babesiosis develops against a background of reduced immunity (elderly, patients with cancer or AIDS, who have undergone complex operations). In other cases, the disease is quite mild. With timely initiation of antibiotic treatment, the prognosis is favorable. In particularly severe cases, a blood transfusion is necessary.