Belkina Yulia Borisovna
Speech therapist
Pinchuk Elena Anatolyevna
Deputy chief physician for medical work, kmn, neurologist, doctor of physical and rehabilitation medicine
Lipovka Nadezhda Sergeevna
Head of the Department of Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Ermakova Elena Vladimirovna
Speech therapist
Yakimova Anna Sergeevna
Speech therapist
Sobolev Arkady Igorevich
Doctor of physical and rehabilitation medicine, neurologist
Swallowing is an important and complex process that involves the functioning of a wide variety of muscle groups and cranial nerves. And impaired swallowing or dysphagia is one of the key problems in organizing nutrition in patients who have suffered a stroke.
It is worth noting that swallowing disorder refers to any, even minor, difficulty or discomfort when moving food into the stomach. Dysphagia includes:
- inability to swallow;
- disturbances in food movement;
- unpleasant disorders associated with food retention, etc.
Moreover, the degree and nature of the disorders may be different for each patient. Doctors note that even with serious illnesses, complete inability to swallow is quite rare. In most cases, patients have difficulty swallowing, etc.
Symptoms of dysphagia
Symptoms of dysphagia in patients also vary from person to person. Here you can find:
- restriction of tongue movements
- weakness of the oral muscles
- salivation;
- inability to form a food bolus;
- slow onset of the swallowing reflex;
- choking;
- retention of food in the mouth, etc.
In most cases, after a stroke, patients have problems taking in liquids or liquid foods. In some cases, patients even have to learn to eat again.
I would like to note that the reason for such difficulties may lie in the fact that in case of various types of violations, incl. strokes, the nervous system suffers, as a result of which sensitivity may be impaired. For example, patients may feel the presence of food in the oral cavity on only one side of the mouth, which causes difficulty chewing and swallowing. In some cases, pathologies of the central nervous system can lead to loss of taste or problems with saliva production.
Among the main complications of dysphagia are:
- penetration of food into the respiratory tract;
- breathing problems;
- pneumonia;
- dehydration;
- exhaustion.
How is diagnosis carried out and methods of working with swallowing problems after a stroke selected?
Dysphagia is diagnosed using several methods. Video fluoroscopy, fiberoptic endoscopy, ultrasound, manometry, and finger method are used. The main task of these methods is to determine at what phase of swallowing the patient has problems. Only by determining this can you solve the nutrition problem, take safety measures and work on the process of restoring the functions of all organs involved in the process. In a situation where the swallowing process is impaired after a stroke, a decision may be made to insert a probe for the first time.
This decision is made on the basis of certified screening tests that help determine whether this patient can be fed through a tube or not, since this may pose a risk of aspiration. The probe and tracheotomy tube are placed temporarily. No more than a month. Because the probe, no matter what “friendly” plastic it is made of for the human body, as a result of constant contact can form bedsores in the nasopharynx, esophagus, and cause damage to the mucous membrane. And constant irritation of the mucous membrane leads to the separation of protective secretions, which can interfere with the process of classes with a speech therapist.
The probe is placed for safety reasons and allows you to solve the power issue. If swallowing is restored, the probe is removed and the person begins to swallow on his own. Then the speech therapist, together with the nutritionist, determines exactly how to feed such a patient - use mixtures, specially crushed food, thickeners (since water is sometimes more difficult to swallow than, for example, puree).
But if swallowing has not been restored within a month, a gastrostomy tube is placed. It has a larger diameter than the probe, which allows, unlike a probe, to freely feed the patient not only with special mixtures, but also with coarser food. It is important that it is possible to clean it.
Sometimes a gastrostomy tube is placed to make swallowing exercises easier. Because doing this with a probe is much more difficult. Therefore, a gastrostomy tube can last a lifetime or as long as needed to restore the swallowing process.
Treatment
Stroke with impaired swallowing in patients is a fairly common occurrence in modern medical practice. As a rule, the swallowing reflex begins to recover approximately 2 or 3 weeks after the attack. The period of complete recovery, as doctors note, is individual for each patient. Some minor disturbances may remain for a very long time.
When feeding patients with swallowing disorders, certain rules should be followed. In this case, patients should regularly perform exercises, the purpose of which is to improve swallowing function and its complete restoration.
Before carrying out any therapeutic actions, it is necessary to adequately assess the patient’s capabilities. First, it is necessary to determine whether the patient can lift and hold his head. The patient should then be asked to cough and swallow saliva. After this, the patient can be given a spoonful of water. In cases where water flows freely from the mouth and the patient does not attempt to swallow it, you should continue feeding the patient through a special tube and wait a little while trying again.
What is a probe
A nasogastric tube is also commonly called a feeding tube. It is inserted directly into the patient's stomach through the nasal passage and esophagus. It is essentially a hollow tube with rounded ends to prevent tissue damage during insertion. The tube is made of light, elastic and absolutely hypoallergenic material. There is a special funnel on the outside. Through it, food is supplied to Zhane using a syringe. In the normal state, the hole is protected by a special cover, which prevents foreign objects from entering the probe. Employees of the patronage service know all the intricacies of feeding a patient through a tube.
Tips for caring for patients with swallowing disorders:
- You should not give a large amount of food at once; it is better to break the feeding into several small portions;
- choose rougher food because... the likelihood of it entering the respiratory tract is minimal;
- food should be aromatic and appetizing;
- do not feed a lying patient;
- serve drinks strictly before or after, but not during the main meal;
- do not tilt the patient’s head back;
- Try to allocate as much time as possible for feeding.
Clinical Brain Institute Rating: 4/5 — 19 votes
Share article on social networks
Swallowing problems after stroke
Home › Articles › Swallowing disorders after stroke
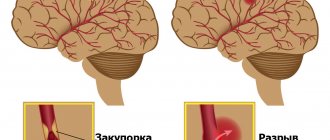
A stroke can cause difficulty swallowing called dysphagia. In this condition, there is a risk of obstruction of the esophagus and aspiration (penetration of the contents of the esophagus into the respiratory tract). To diagnose dysphagia, an examination is performed, including an X-ray examination of the esophagus. The doctor will prescribe treatment and give the necessary recommendations on what nutrition should be and how to eat.
How to eat
To make it easy to swallow without fear that food will linger in the esophagus, dishes must have a certain consistency and thickness. Thicker foods can be mixed with liquid foods, making swallowing safer. If eating by mouth is unsafe, you will need another route of nutrition. Tube feeding is often used. The doctor will discuss these questions with you and your loved ones.
Assessment of swallowing function and its disorders
Swallowing is a complex biomechanical process involving the work of various groups of muscles and cranial nerves. If any part of this complex system stops working, it can cause patients to have difficulty drinking and drinking.
Patients with stroke often have a problem with impaired swallowing - dysphagia. Dysphagia can cause aspiration, the penetration of foreign bodies into the lungs. Aspiration can cause suffocation, the development of infectious diseases of the respiratory tract, and pneumonia. Aspiration may not be noticeable (no cough). Aspiration pneumonia is the result of bacteria from the oral cavity entering the lungs.
To prevent aspiration, it is very important to maintain oral hygiene after eating and regularly clear it of food and saliva accumulation.
Some warning signs and symptoms of dysphagia:
•difficulty chewing; •poor oral hygiene; •drooling and inability to swallow saliva; •sloppy eating behavior, food falling out of the mouth while eating; •slurred speech; •coughing or clearing your throat before, during or after eating; •change in voice quality during or after swallowing (“gurgling” voice, hoarseness, temporary loss of voice); •regurgitation; • difficulty breathing, suffocation; •increased body temperature; •weight loss; •loss of interest in food, poor appetite or refusal to eat; •increasing the duration of meals; •a feeling that food or liquid is getting stuck in the throat when swallowing; •anxiety about eating or drinking.
If the patient does not have swallowing dysfunction, then he can be fed, strictly following practical feeding recommendations.
Feeding patients with impaired swallowing
Features of the patient's position that ensure the most effective and safe swallowing:
• Feeding is carried out only in a sitting position (with support under the back). • Head tilt forward. • Turn to the healthy side at the time of swallowing.
Principles of nutritional change:
• food should look appetizing; • food should be warm enough, since patients with dysphagia need a long time to eat it. If the patient does not feel warm food in his mouth, he should be fed food at room temperature; • Offer solid and liquid foods at different times. In this case, the liquid will not push solid food down the throat, and the patient will not swallow poorly chewed food or choke on liquid; • semi-hard foods are best tolerated: casserole, thick yogurt, pureed vegetables and fruits, thin porridges; • it is necessary to select the consistency of food (soft food, thick puree, liquid puree) and liquid (consistency of mousse, yogurt, thick jelly, syrup, water). It should be remembered that with thinner food or drink it is more difficult to take a safe (without aspiration) sip; • it is necessary to exclude from the diet foods that often cause aspiration (food entering the upper respiratory tract): liquids of normal consistency (water, juices, tea), bread, cookies, nuts, etc.; • when feeding, food is placed on the unaffected side of the mouth in small portions; • control over the need to use dentures is needed; a thorough inspection of the oral cavity after finishing feeding (the remaining food can be aspirated); • after feeding, the patient remains in an upright position for 45-60 minutes. • after feeding, the patient remains in an upright position for 45-60 minutes.
Need to remember:
• only a small amount of food can be given at a time; • do not give drinks with food (drinks should be given before or after food); • you cannot feed a lying person; • do not tilt the patient's head back during feeding; • teeth and dentures must be brushed at least 2 times a day to ensure the cleanliness of the oral cavity.
Care Tips
Consult your doctor about any nutritional problems that concern you. Try to create a meal plan taking into account the patient's dietary preferences.
More detailed information about the nutritional habits of a stroke patient, feeding through a nasogastric tube, as well as methods for restoring swallowing can be found in the electronic training course “Rehabilitation after a stroke at home.”
Feeding process
The procedure is carried out according to the following algorithm:
- The patient's body is given a semi-sitting position;
- The outer part of the probe is lowered below the patient’s neck and compressed with a special clamp;
- The funnel is connected to the syringe, it rises to a level of up to half a meter above the stomach, after which the clamp is removed.
- Food is served slowly, with virtually no pressure; no more than 150 ml should be administered in 5-6 minutes.
- After finishing feeding, it is necessary to rinse the area by applying 30-50 ml of water through it.
- Next, the tube is clamped again, lowered, and the inlet is closed with a plug.
Tube is a modern and effective way of feeding seriously ill patients. It has a lot of advantages. Unlike intravenous nutrition, in this case atrophy of the gastric mucosa is not allowed, the gastrointestinal tract system remains in working order. The enteral system can be used for a long time. The probe is installed for three weeks. The administration procedure must be carried out by a doctor, and he must also give his recommendations regarding the feeding procedure and diet.
Main indications for use
Eating through a tube is carried out in cases where the patient is not able to do this on his own. His swallowing function is depressed, there is no clear consciousness, or there are serious lesions in the throat and oral cavity. The probe is most often installed in the following cases:
- After a stroke, if we are talking about damage to the areas of the brain that control the swallowing reflex, the function may be partially or completely inhibited. A return to normal eating habits is possible after completion of rehabilitation. In case of extensive damage and advanced age of the patient, enteral nutrition can be permanent.
- For physical injuries - head injuries, severe swelling of the tongue and larynx.
- If the patient is in a coma or unconscious.
- With the development of psychological disorders, when the patient refuses to eat.
- Neurological diseases (multiple sclerosis, Parkinson's, Alzheimer's), accompanied by corresponding disorders.
- During surgical interventions in the gastrointestinal tract.
Enteral feeding is prescribed in cases where the traditional form of eating is impossible or difficult, if the patient may choke, or if incoming food may infect damaged tissues and organs.