Behavioral therapy in the treatment of overactive bladder and urinary incontinence
The International Continence Society (ICS) defines overactive bladder (OAB) as a condition in which the patient experiences a sudden urge to urinate that is difficult to control, often accompanied by frequent urination during the day and/or night.
OAB is not a disease, it is a complex of symptoms (syndrome), which in themselves are not life-threatening, but significantly reduce the patient’s quality of life. This diagnosis is established by excluding other possible conditions that have similar manifestations and require specialized treatment (for example, urinary tract infection).
According to modern data, about 16% of the adult population suffers from OAB. This disease occurs equally often in both women and men. However, in women, OAB is more often accompanied by urinary incontinence. The incidence of OAB and the severity of symptoms increase with age.
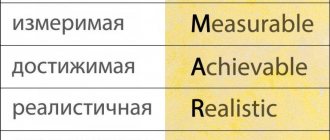
Today, there are many different treatments for OAB. According to the recommendations of the American Urological Association from 2012 (revision from 2014), all available treatment methods are divided into 5 groups depending on the ratio of benefits to the patient, as well as the invasiveness of treatment, the severity of possible complications and their reversibility.
The first line of treatment for overactive bladder is behavioral therapy. This type of therapy has no side effects, and its effectiveness is not inferior to therapy with M-anticholinergics, therefore it is recommended for all patients with OAB. However, to achieve maximum results, the patient is required to have the right attitude towards treatment, free time that the patient can devote to training, as well as periodic visits to a doctor or specially trained nurse for the purpose of correction and evaluation of the effectiveness of therapy.
“Behavioral therapy” is a collective term, it refers to a number of methods aimed at changing the patient’s habits or his environment. In most cases, these methods are used in combination with each other, which increases the effectiveness of therapy. There are two approaches to treating OAB using behavioral therapy. The first is to change bladder function by influencing urination patterns. In this case, a method called “bladder training” is used. In the second case, attention is paid to the pelvic floor muscles (exercises for the pelvic floor muscles to strengthen them and improve urinary retention, as well as teaching the patient techniques for suppressing the imperative urge to urinate).
Next, the main behavioral therapy methods used in the treatment of OAB will be presented.
Bladder training
The patient urinates at regular intervals. The initial interval is set based on the urination diary data and subsequently the interval between urinations gradually increases by 15-30 minutes.
*Bladder training is always combined with the technique of suppressing the imperative urge to urinate!
Suppressing the urgency to urinate
Against the background of an imperative urge to urinate, the patient makes rapid contractions of the pelvic floor muscles until the urge subsides. It is important to know that during an urgent urge you should not rush to the toilet. Motor activity against the background of an imperative urge only increases intra-abdominal and, consequently, intravesical pressure, which in turn strengthens the imperative urge. In addition, visual cues such as the bathroom or toilet can trigger urinary incontinence. During an imperative urge, you should sit down, if possible, relax the muscles of the body and perform a series of rapid contractions of the pelvic floor muscles aimed at suppressing the imperative urge. Only after the imperative urge to urinate has passed can you safely go to the toilet.
Exercises for the pelvic floor muscles
The patient performs 8-12 full voluntary contractions of the pelvic floor muscles. Each contraction is held for 6-8 seconds, after which the muscles relax. Rest between contractions is also 6-8 seconds. Upon completion of the exercise, 5-10 rapid contractions of the pelvic floor muscles are performed (without rest). This complex is performed 5 times a day.
Obesity
Based on clinical work, the positive effect of weight loss on urinary incontinence has been shown.
Smoking
To date, there are no studies proving the positive effect of quitting smoking on urinary incontinence. Nevertheless, this recommendation is quite logical: quitting smoking reduces the risk of developing bladder cancer. This recommendation is also appropriate in case of urinary incontinence, which manifests itself mainly when coughing.
Coffee
Consuming large amounts of caffeine contributes to the development of OAB.
Limiting fluid intake
This recommendation is appropriate for both patients with stress urinary incontinence and patients with OAB. In the first case, the positive effect is due to the fact that during physical activity, urine loss becomes significantly less when the bladder is not full. In the second, slower filling of the bladder associated with limited fluid intake leads to a reduction in the risk of involuntary contraction of the bladder muscle and, as a consequence, urgency.
*Applicable to patients with normal/high drinking regime. The drinking regime is established on the basis of a urination diary.
Frequent urination in women reasons or why frequent urination
The causes of an overactive bladder may be an excessive number or sensitivity of nerve endings (receptors) or dysfunction of the muscular wall of the bladder due to chronic cystitis, hormonal imbalance, etc.
To correctly diagnose an overactive bladder, it is necessary to exclude other urological diseases that may manifest as detrusor overactivity syndrome, such as chronic cystitis, urolithiasis, and bladder tumors. Cystoscopy plays a decisive role in making the correct diagnosis , which allows not only to assess in detail the condition of the bladder wall, but also to determine its functional capacity.
Consequences and treatment
It is known that the occurrence of this symptom causes severe anxiety in dystonics. Even if a person is sure that he does not have any organic disease, anxiety about frequent urination is still present, since the symptom negatively affects many aspects of life. Some individuals begin to deliberately drink less fluid, hoping that this will make them visit the toilet less often, but such behavior is extremely erroneous. Firstly, such actions will not lead to the desired result, and secondly, the health condition may worsen - a person needs to drink enough water daily. Anxiety caused by frequent urination during VSD, in turn, can lead to the following manifestations:
- various sleep disorders;
- headache;
- depressive states;
- decreased self-esteem;
- avoidance of social interaction.
Additionally, in some cases, people with polyuria develop a condition where they simply feel like they need to empty their bladder. As a rule, very little liquid comes out in this case. In this case, symptoms such as severe nervousness, anxiety, an obsessive desire to empty the bladder as quickly as possible, and fear of not being able to go to the toilet appear.
It is strictly not recommended to delay treatment of the disease. First of all, a person suffering from these manifestations needs to see a psychotherapist and put his nervous system in order. Self-help may include several items.
- Conducting breathing exercises and relaxation techniques. Meditation is an excellent tool.
- Proper distribution of work and rest.
- Hardening the body, contrast shower, healthy sleep.
- Avoiding stressful situations.
- Taking mild sedatives (Valerian, Motherwort, Hawthorn).
- Positive emotions.
Frequent urination with VSD is a symptom that negatively affects various aspects of life. A person, realizing that frequent visits to the toilet is simply inevitable, may not only refuse exciting trips and promising work, but also begin to avoid social interaction
It is necessary to pay close attention to this problem and promptly seek professional help. Various unpleasant symptoms, as a rule, cease to bother the patient when his nervous system becomes more resistant to stressful situations
Frequent urination is a symptom of vegetative neurosis. This problem bothers the patient during the crisis and after it
It is worth paying attention to this manifestation of the disease when visiting a doctor. Let's figure out what this symptom means and how to get rid of it
How to treat cystitis due to nerves
An integrated approach is used in treatment. Antibacterial therapy, diuretics and anti-inflammatory drugs are prescribed. It is recommended to enhance the effect of drugs using physiotherapy methods for chronic cystitis: for example, magnetic therapy procedures on the Avantron chair.
In order to help the body cope with the disease and prevent recurrences, the following measures are recommended:
- Restoring a healthy lifestyle, which includes long hours of sleep, a healthy diet, alternating periods of rest with exercise, daily leisurely walks in the fresh air or gentle exercise
- Avoiding or exiting a stressful situation; it may be necessary to change jobs or stop communicating with people who cause nervous tension; if you are nervous, try to distract yourself with pleasant things or thoughts
- Spa treatment or a vacation trip: this will allow the whole body to relax and strengthen
If urgently needed, your doctor may prescribe antidepressants or herbal anti-anxiety medications to help the body break the vicious cycle of stress.
Traditional medicine will also not be superfluous. For example, chamomile decoction has an anti-inflammatory effect and calms the nervous system. And mint tea improves sleep and reduces pain due to inflammation.
Features of the pathological process
Initially, the specialist will need to find out whether there are any physiological reasons causing difficulty in urinating. Indeed, due to various pathological processes and kidney problems, a person may experience stagnation of urine. To treat, you will have to eliminate the factor that caused the problem and take diuretics (diuretics).
With bladder neurosis, there are no physiological disorders and the urinary tract is without pathologies. The essence of the problem lies in the malfunction of the nervous system, so doctors classify this pathology as a disease caused by a mental disorder.
The outflow of urine occurs thanks to 2 sphincters in the bladder, which relax and contract as needed. The process is controlled by the autonomic nervous system (ANS), that is, a person cannot consciously control the process.
The following sections of the ANS are responsible for the work of sphincters in the bladder:
- Sympathetic. It serves to contract muscles and, accordingly, to close the sphincter. Thanks to the sympathetic department, a person can retain urine in the body;
- Parasympathetic. It is designed to relax muscle tissue, including the sphincter. It is the parasympathetic department that serves to remove urine from the body.
If a person experiences malfunctions in these departments, then all the blame lies with bladder neurosis and you need to know its symptoms and methods of treatment, especially when the problem occurs in children.
Causes of dysuria in VSD
Often, as a crisis develops, urination becomes abundant and frequent. Urination is controlled by the somatic and autonomic nervous systems. A decrease or increase in urination is associated with changes in drinking habits, ambient temperature, and the use of certain medications.
With VSD, the functioning of the nervous system is disrupted, and this often affects the functioning of the bladder.
If the tone of the sympathetic parts of the NS increases, the renal arterioles, under the influence of adrenaline released in large quantities, narrow, and the activity of vasopressin increases. This hormone is an antidiuretic, it reduces urine filtration and excretion.
Increased urination occurs due to activation of the parasympathetic parts of the nervous system. The work of these centers changes under the influence of stressful situations. That is, the reason for frequent and copious urination during VSD is episodic or chronic stress.
- When a vegetative crisis is provoked by an unexpected psycho-emotional shock, copious urine output occurs for several hours.
- With chronic stress, dysfunction of the autonomic nervous system constantly develops, and this leads to the fact that the sick person constantly experiences discomfort from the need to frequently visit the toilet.