Pharmacological properties of the drug Velaxin
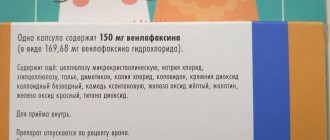
Venlafaxine ((±)-1-[dimethylamino-1-(methoxy-phenyl)-ethyl] cyclohexanol hydrochloride) is an antidepressant with a new chemical structure that cannot be classified as tricyclic, tetracyclic or other known antidepressants. It is a racemic mixture of two active enantiomers. The mechanism of the antidepressant effect of venlafaxine is associated with increased neurotransmitter activity of the central nervous system. Venlafaxine and its main metabolite O-desmethyl venlafaxine (ODV) are potent inhibitors of neuronal reuptake of serotonin and norepinephrine, and also inhibit dopamine reuptake. In addition, both single and chronic administration of venlafaxine and EDV attenuates β-adrenergic reactions. They are equally effective in influencing the reuptake of neurotransmitters. Venlafaxine does not inhibit MAO activity. Venlafaxine has no affinity for opiate, benzodiazepine, phencyclidine, or N-methyl-d-aspartate (NMDA) receptors; it also does not affect the release of norepinephrine from brain tissue. With repeated use of the drug, equilibrium concentrations of venlafaxine and its only active metabolite in the blood plasma are achieved within 3 days. Venlafaxine and EDV have linear pharmacokinetics with total daily doses ranging from 75 to 450 mg. Absorption of venlafaxine after taking a single dose of the drug orally is almost 92%, absolute bioavailability is about 45%. After administration of Velaxin extended-release capsules, maximum plasma concentrations of venlafaxine and its active metabolite EDV are achieved within approximately 6 and 8 hours, respectively. The rate of absorption of venlafaxine released from extended-release capsules is less than the rate of its elimination. Therefore, the average half-life of venlafaxine from the body after taking Velaxin (15±6 hours) is actually the half-life in the absorption phase, and not the half-life in the distribution phase (5±2 hours), which is observed after the use of tablets. After administration of venlafaxine in equivalent doses in tablet or extended-release capsule form, venlafaxine AUC exposure and EDV were similar in both dosage forms, and their plasma concentrations were slightly lower after administration of venlafaxine in capsule form. Thus, extended-release capsules provide slower absorption but the same extent of absorption (i.e., AUC) as Velaxin tablets. Venlafaxine is extensively metabolized during the initial passage through the liver, mainly with the participation of CYP 2D6, with the formation of the main metabolite EDV. It is also metabolized to N-desmethyl venlafaxine and some other metabolites with the participation of CYP 3A3/4. Venlafaxine and its metabolites are excreted mainly by the kidneys. Approximately 78% of the administered dose of venlafaxine is determined in the urine over 48 hours in the form of unchanged venlafaxine, unconjugated EDV, conjugated EDV or other metabolites. In case of renal and hepatic insufficiency, the half-life of venlafaxine and its active metabolite EDV increases. Taking the drug with food does not affect the absorption of venlafaxine and the further formation of EDV. The age and gender of the patient do not affect the pharmacokinetics of the drug. The drug does not accumulate in the body. Velaxin extended-release capsules contain microspheres that, when entering the gastrointestinal tract, slowly release the active component. The insoluble part of these microspheres is excreted in the feces.
Velaxin extended-release capsules 75 mg 28 pcs.
Velaxin capsules should be taken orally with meals. Each capsule must be swallowed whole with sufficient liquid. Capsules should not be broken, crushed, chewed or placed in water. The entire daily dose, consisting of one or more capsules, should be taken in one dose (morning or evening) at approximately the same time each time. For depression, the recommended starting dose is 75 mg once a day every day. In many cases, this dose has a sufficient therapeutic effect. If the doctor considers it appropriate to use a higher dose (for example, for severe depression or conditions requiring hospital treatment), a dose of 150 mg 1 time per day can be immediately prescribed. Subsequently, the daily dose can be increased stepwise by 75 mg at intervals from 4 days to two weeks until the desired effect is achieved. The maximum recommended daily dose is 225 mg, for severe depression - 375 mg. After achieving the desired therapeutic effect, the doctor can gradually reduce the dose to a sufficiently effective level. For generalized anxiety disorders and social phobias, the recommended starting dose is 75 mg once a day daily. In most cases, this dose is sufficient; a positive effect is usually observed after 1 week. If after two weeks of treatment there is no significant improvement, the doctor may increase the daily dose to 150 mg at a time. Maintenance therapy and relapse prevention. Treatment for depressive episodes should be continued continuously for several months. Velaxin is effective with long-term therapy (lasting 6–12 months). For maintenance therapy and to prevent relapse or new episodes, doses effective in treating the initial episode are used. Visit your doctor regularly, at least once every 3 months, to monitor the effectiveness of Velaxin therapy. Special groups of patients. Doses for the treatment of elderly patients and patients with impaired liver or kidney function are usually lower than usual and should be selected individually by the doctor, taking into account the functional state of the kidneys and liver. For patients on hemodialysis, the daily dose of venlafaxine should be halved, and they should take the drug, if possible, after the end of the hemodialysis session. Transferring patients from Velaxin tablets. Your doctor may prescribe you Velaxin extended-release capsules instead of Velaxin tablets. In this case, he will determine which dose of Velaxin extended-release capsules is closest to the total daily dose of Velaxin tablets you are taking. Discontinuation of the drug. After abruptly stopping taking the drug Velaxin, the following symptoms may be observed: fatigue, drowsiness, headache, nausea, vomiting, dry mouth, dizziness, diarrhea, insomnia, restlessness, anxiety, nervous irritability, confusion, pathologically elevated mood, numbness, sweating. These side effects are not dangerous and usually go away spontaneously. However, as with other antidepressants, it is important to gradually reduce the dose before stopping the drug, especially after taking high doses. If high doses have been used for more than 6 weeks, dose reduction should take at least 2 weeks. The duration of the course of treatment is determined by the doctor. Discontinuation of the drug or dose change should be carried out as prescribed and under the supervision of a physician.
Use of the drug Velaxin
Capsules should be taken whole with a meal with liquid. Capsules should not be divided, crushed, chewed or dissolved. The daily dose should be taken in one dose (morning or evening) at the same time. Depression The recommended dose is 75 mg/day in one dose. If, taking into account the course of the disease, a higher dose is necessary, for example, in case of severe depression or inpatient treatment of the patient, the recommended initial dose may be 150 mg/day in one dose. After this, the daily dose can be increased by 37.5–75 mg at intervals of ≥2 weeks, but not less than 4 days until the required therapeutic effect is achieved. The recommended maximum dose of Velaxin is 225 mg/day for moderate depression and 350 mg for severe depression. After achieving the desired therapeutic effect, the dose should be gradually reduced to the minimum effective, taking into account the individual response and tolerability of each patient. When used in high doses, the risk of developing side effects of the drug increases. Generalized anxiety disorders and social anxiety disorders (social phobia) The recommended dose of Velaxin is 75 mg/day in one dose. If after 2 weeks of treatment there is no noticeable improvement in the condition, the daily dose can be increased to 150 mg/day in one dose. When used in a daily dose of 75 mg, an anxiolytic effect is observed after 1 week. Prevention of relapses or new episodes The effectiveness of venlafaxine has been established with long-term therapy (up to 12 months for depression and social phobia; up to 6 months for generalized anxiety disorders). Treatment of acute episodes of depression must be continued for at least 6 months. The doses typically used to prevent a relapse or new episode are similar to those used to treat patients with a primary episode. It is necessary to regularly (at least once every 3 months) examine the patient to monitor the effectiveness of long-term therapy with Velaxin. Transfer of patients receiving therapy with Velaxin in the form of tablets to taking a capsule form of the drug Patients with depression receiving Velaxin tablets in a therapeutic dose can be transferred to taking the drug in the form of long-acting capsules with the appointment of the nearest equivalent dose. Sometimes individual dose adjustment may be required. Renal failure When the glomerular filtration rate is 30 ml/min, no dose adjustment is required. With a glomerular filtration rate of 10–30 ml/min, the dose should be reduced by 50%. Due to the increased half-life of venlafaxine and its active metabolite in these patients, the daily dose should be taken in one dose. It is not recommended to use venlafaxine if the glomerular filtration rate is ≤10 ml/min, since there is insufficient data on therapy in these patients. For patients on hemodialysis, the daily dose of the drug should be reduced by 50% and, if possible, used after completion of the hemodialysis procedure. Liver failure In mild liver failure (prothrombin time ≤14 s), no dose adjustment is required. In case of moderately severe liver failure (prothrombin time - 14–18 s), the dose should be reduced by 50%. It is not recommended to use venlafaxine in severe hepatic impairment (prothrombin time 18 s), as there is insufficient data on this therapy. Elderly patients Caution should be exercised when prescribing the drug to elderly patients (due to the possibility of renal dysfunction), and the drug is prescribed in the minimum effective dose. When increasing the dose, the patient should be under regular medical supervision. Cancellation of Velaxin Abrupt cessation of Velaxin therapy, especially after taking the drug in high doses, can cause the development of withdrawal syndrome, and therefore a gradual dose reduction is recommended before complete discontinuation of the drug. If the drug has been used in high doses for 6 weeks, a dose reduction period of at least 2 weeks is recommended. The length of the period required to reduce the dose depends on the dose size, duration of therapy, as well as the individual sensitivity of the patient.
Velaxin®
Depression increases the risk of suicidal thoughts and suicide attempts. This risk persists until stable remission occurs. Therefore, patients should be under constant medical supervision and should be given only small quantities of the drug capsules to reduce the risk of possible abuse and/or overdose. Velaxin® should not be used in the treatment of children and adolescents under 18 years of age. An increase in the likelihood of suicidal behavior (suicide attempt and suicidal ideation), as well as hostility, was observed more often in clinical trials among children and adolescents receiving antidepressants compared with groups receiving placebo.
Aggressive behavior has been reported while taking venlafaxine (especially at the beginning of treatment and after discontinuation of the drug).
The use of venlafaxine may cause psychomotor restlessness, which clinically resembles akathisia, characterized by restlessness with a need to move, often combined with an inability to sit or stand still. This is most often observed during the first few weeks of treatment. If these symptoms occur, increasing the dose may have an adverse effect and the advisability of continuing to take the drug should be considered.
Like all antidepressants, venlafaxine should be prescribed with caution to patients with a history of mania and/or hypomania, as the drug may cause an increase in their symptoms. In these cases, medical supervision is necessary.
Caution should be exercised when treating patients with a history of seizures. If convulsive seizures occur or their frequency increases, treatment with venlafaxine should be interrupted.
Like selective serotonin reuptake inhibitors, venlafaxine should be used with caution when used concomitantly with antipsychotic drugs, as symptoms resembling neuroleptic malignant syndrome may develop.
Patients should be warned to seek immediate medical attention if rash, hives, or other allergic reactions occur.
Some patients experienced a dose-dependent increase in blood pressure while taking venlafaxine, and therefore regular monitoring of blood pressure is recommended, especially at the beginning of treatment or when increasing the dose.
Isolated cases of orthostatic hypotension have been described while taking venlafaxine. Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
Venlafaxine may cause an increase in heart rate, especially at high doses. Particular caution should be exercised when prescribing the drug to patients with conditions that may be aggravated by an increase in heart rate.
There are insufficient studies of the use of venlafaxine in patients who have recently suffered a myocardial infarction or suffering from decompensated heart failure, so this drug should be used with caution in these patients.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes, so caution is required when treating patients predisposed to bleeding.
Hyponatremia and/or syndrome of insufficient antidiuretic hormone secretion (SIADH) may occur while taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics).
Cases of mydriasis have been reported while taking venlafaxine, so patients with a predisposition to increased intraocular pressure or those at risk of angle-closure glaucoma require careful medical monitoring.
In case of renal and liver failure, special caution is required. In some cases, a dose reduction is required (see section "Method of administration and dosage").
The safety and effectiveness of using venlafaxine with weight-loss drugs, including phentermine, have not been established, so their simultaneous use (as well as the use of venlafaxine as monotherapy for weight loss) is not recommended. Clinically significant increases in serum cholesterol levels have been observed in some patients receiving venlafaxine for at least 4 months. Therefore, when taking the drug for a long time, it is advisable to monitor serum cholesterol levels.
After stopping the drug, especially abruptly, withdrawal symptoms often occur (see section “Side effects”). The risk of withdrawal symptoms may depend on several factors, including course length and dose, and the rate of dose reduction.
Withdrawal symptoms such as: dizziness, sensory disturbances (including paresthesia and electrical sensations), sleep disturbances (including insomnia and unusual dreams), agitation or anxiety, nausea and/or vomiting, tremor, sweating, headache, diarrhea, rapid and increased heart rate, and emotional instability are usually mild to moderate in severity, but may be severe in some patients. They are usually observed in the first days after discontinuation of the drug, although there have been isolated reports of such symptoms in patients who accidentally missed a dose. Usually these phenomena resolve on their own within 2 weeks; however, in some patients they may be longer lasting (2-3 months or more). Therefore, before discontinuing venlafaxine, it is recommended to gradually reduce its dose over several weeks or months, depending on the patient's condition (see sections "Dosage and Administration").
Contraindications to the use of the drug Velaxin
Hypersensitivity to any component of the drug. Simultaneous use of any antidepressant from the MAO inhibitor group, as well as for 14 days after discontinuation of irreversible MAO inhibitors. After complete discontinuation of venlafaxine, therapy with MAO inhibitors can be started no earlier than 7 days later. Diseases of the cardiovascular system (heart failure, coronary artery disease, ECG changes - pre-existing increase in the QT on the ECG), hypertension (arterial hypertension), electrolyte imbalance. Age up to 18 years. During pregnancy and breastfeeding.
Side effects of the drug Velaxin
Side effects are divided by body system and frequency of occurrence: very often (1/10); often (≤1/10, but 1/100); sometimes (≤1/100, but 1/1000); rare (≤1/1000); very rare (≤1/10,000). General symptoms: very often - asthenia, headache; often - abdominal pain, chills, increased body temperature; rarely - anaphylaxis. Gastrointestinal tract: very often - constipation, nausea; often - loss of appetite, diarrhea, vomiting; sometimes - bruxism, reversible increase in the activity of liver enzymes; rarely - gastrointestinal bleeding; very rarely - pancreatitis. Cardiovascular system: often - tachycardia, hypertension (arterial hypertension), dilatation of blood vessels; sometimes - hypotension/orthostatic hypotension, loss of consciousness, arrhythmias, tachycardia; very rarely - pirouette-type tachycardia, increased QT on ECG, ventricular tachycardia, ventricular fibrillation. Respiratory system: often - difficulty breathing, yawning; very rarely - eosinophilic infiltrates in the lungs. Nervous system: very often - dizziness, dry mouth, insomnia, anxiety, drowsiness; often - unusual dreams, agitation, anxiety, confusion, increased muscle tone, paresthesia, tremor; sometimes - apathy, hallucinations, myoclonus; rarely - ataxia with impaired balance and coordination of movements, speech impairment, including dysarthria, mania or hypomania, as well as manifestations that resemble neuroleptic malignant syndrome (NMS), seizures, serotonergic syndrome; very rarely - delirium, extrapyramidal disorders, including dyskinesia and dystonia, psychomotor agitation/akathisia. Genitourinary system: very often - anorgasmia, erectile dysfunction, impaired ejaculation and orgasm; often - frequent urination, decreased libido, menstrual irregularities; sometimes - urinary retention, menorrhagia; rarely - galactorrhea. Sense organs: often - blurred vision and accommodation, mydriasis, noise and ringing in the ears; sometimes - a change in taste sensations. Skin: very often - sweating; often - skin rashes and itching; sometimes - angioedema, maculopapular rash, urticaria, photosensitivity, alopecia; rarely - erythema multiforme, Stevens-Johnson syndrome. Blood system: sometimes - ecchymosis, bleeding from the mucous membrane; rarely - increased bleeding time, hemorrhage, thrombocytopenia; very rarely - agranulocytosis, aplastic anemia, neutropenia, pancytopenia. Metabolism: often - increased cholesterol levels in the blood serum, increase or decrease in body weight; sometimes - hyponatremia, increased activity of liver transaminases; rarely - hepatitis; very rarely - increased prolactin levels. Musculoskeletal system: often - arthralgia, myalgia; sometimes - muscle spasms; very rarely - rhabdomyolysis.
Venlafaxine
Use during pregnancy and breastfeeding
Venlafaxine should not be prescribed to pregnant and breastfeeding women, because
The safety of the drug during pregnancy and lactation in women has not been sufficiently established, due to the fact that there are no adequately controlled clinical studies on a sufficiently large sample of such patients. This concerns the health of both the mother and, to a greater extent, the fetus/child. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug. Venlafaxine and its metabolite (EFV) are excreted into breast milk. If it is necessary to take the drug during lactation, breastfeeding must be stopped.
In practice, there are cases of prescribing venlafaxine to mothers during pregnancy and shortly before childbirth, when in a particular situation the expected benefit to the mother outweighs the potential risk to the fetus. In these cases, newborns often experienced complications that required: increased hospitalization, maintenance of breathing and tube feeding. These complications can develop immediately after childbirth and are also typical when taking other antidepressants from the SNRI group or SSRIs (not containing venlafaxine). In such cases, the following clinical symptoms in newborns have been reported: respiratory disorders, cyanosis, apnea, convulsions, temperature instability, feeding difficulties, vomiting, hypoglycemia, muscle hypertension or hypotonia, hyperreflexia, tremor, trembling, irritability, lethargy, constant crying, drowsiness or insomnia. Such disturbances may indicate the serotonergic effects of the drug Venlafaxine.
If venlafaxine was used during pregnancy and maternal treatment was completed shortly before delivery, the newborn may experience withdrawal symptoms. In such a newborn, the presence of serotonin syndrome or neuroleptic malignant syndrome should be excluded. Epidemiological evidence suggests that use of SSRIs during pregnancy, especially late in pregnancy, may increase the risk of persistent neonatal pulmonary hypertension.
special instructions
Suicide and suicidal behavior
Depression is associated with an increased risk of suicidal ideation, self-harm, and suicide (suicidal behavior). This risk persists until significant remission occurs. Since improvement may not be observed during the first few weeks of therapy or even longer, patients should be closely monitored until such improvement occurs. Based on accumulated clinical experience, the risk of suicide may increase in the early stages of recovery.
Patients with a history of suicide attempts or high levels of suicidal ideation prior to treatment are at greater risk for suicidal ideation or suicide attempts and should be closely monitored. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with mental disorders found that antidepressants were at increased risk of suicidal behavior compared with placebo in patients under 25 years of age. Drug treatment of these patients, and in particular those at high risk of suicide, should be accompanied by careful monitoring, especially early in therapy and during dose adjustment. Patients (and caregivers of such patients) should be warned to monitor for any signs of clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek immediate medical attention if these symptoms occur.
In a small number of patients taking antidepressants, incl. venlafaxine, aggression may occur during initiation of treatment, dose changes, or discontinuation of treatment.
Clinical studies conducted to date have not revealed tolerance or dependence to venlafaxine. Despite this, as with other drugs that act on the central nervous system, the physician should closely monitor patients for signs of drug abuse, as well as patients with a history of such symptoms.
Special patient groups
Venlafaxine is not approved for use in children.
In patients with a history of aggression, venlafaxine should be used with caution.
In patients with affective disorders, bipolar disorder when treated with antidepressants, incl. venlafaxine, hypomanic and manic states may occur. Like other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
Convulsive disorders may occur during therapy with venlafaxine. As with all antidepressants, venlafaxine should be used with caution in patients with a history of seizure disorders and such patients should be closely monitored. Treatment should be discontinued if seizures develop.
Akathisia
The use of venlafaxine has been associated with the development of akathisia, which is characterized by an unpleasant feeling of internal motor restlessness for the patient and manifested in the patient’s inability to sit quietly in one position for a long time or remain motionless for a long time. This condition may occur at the beginning of treatment and during the first weeks of treatment. In patients who develop such symptoms, increasing the dose is not recommended.
Bipolar disorder
Before starting treatment, it is necessary to identify those patients who are at risk for bipolar disorder. Such a check should include a detailed examination of the medical history, incl. family, to identify cases of suicide, bipolar disorder. It should be noted that venlafaxine is not recommended for use in the treatment of bipolar depression.
Use in patients with concomitant diseases
Clinical experience with the use of venlafaxine in patients with concomitant diseases is limited.
It should be used with caution in patients with diseases in which the effect of venlafaxine on hemodynamic parameters and/or metabolism may be significant.
Patients should be warned to immediately consult a doctor if a rash, urticaria or other allergic reactions occur.
Some patients while taking venlafaxine experienced a dose-dependent increase in blood pressure and/or an increase in heart rate, so regular monitoring of blood pressure and ECG is recommended, especially during the period of adjusting or increasing the dosage of venlafaxine. In post-marketing experience with venlafaxine (overdose), fatal cardiac arrhythmias have been reported. Before prescribing venlafaxine to patients at high risk of developing serious cardiac arrhythmias, the ratio of the likely benefit to the possible risk of use should be assessed.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance in order to prevent injury.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
Venlafaxine has not been studied in patients with recent myocardial infarction and decompensated heart failure. The drug should be prescribed to such patients with caution.
Taking SSRIs or venlafaxine in patients with diabetes may cause changes in plasma glucose levels. Dosage adjustments of insulin and/or antidiabetic medications may be required.
During treatment, it is recommended to refrain from drinking any alcohol-containing drinks.
The safety and effectiveness of venlafaxine in combination with weight loss medications (including phentermine) have not been established. The simultaneous use of venlafaxine and drugs that reduce body weight is not recommended.
Women of childbearing potential should use appropriate contraception while taking venlafaxine.
Explanations of special symptoms and conditions that may occur during treatment with the drug
Dry mouth occurs in 10% of patients receiving venlafaxine. This may increase your risk of developing tooth decay. Patients should practice good oral hygiene.
The use of venlafaxine may cause the development of akathisia, characterized by subjective discomfort or restlessness and the need to move frequently, often accompanied by an inability to sit or stand still. This mostly occurs during the first few weeks of treatment. Increasing the dose in patients who develop these symptoms may cause undesirable effects.
In placebo-controlled clinical trials, a clinically significant increase in serum cholesterol was reported in 5.3% of patients. Cholesterol level control is necessary during long-term treatment.
Withdrawal syndrome
When stopping treatment, withdrawal symptoms are common, especially if it is stopped abruptly. The risk of withdrawal syndrome may depend on several factors, including the duration of treatment, the size of therapeutic doses and the rate of dose reduction. These symptoms are very rarely reported in patients who accidentally missed taking the drug.
Withdrawal symptoms usually occur within the first few days after stopping treatment. These symptoms usually go away within 2 weeks, although in some people they may last 2-3 months or more. It is recommended to gradually reduce the dose of venlafaxine when stopping the drug - over several weeks or months, depending on the severity of the clinical symptoms of the disease.
Serotonin syndrome
Taking venlafaxine, like other serotonergic drugs, can cause serotonin syndrome, a potentially life-threatening condition, especially when used concomitantly with other drugs that can affect the serotonergic neurotransmitter systems such as MAO inhibitors.
Symptoms of serotonin syndrome may include mental status changes (agitation, hallucinations, coma), autonomic instability (tachycardia, blood pressure lability, hyperthermia), neuromuscular disorders (hyperreflexia, incoordination), and/or gastrointestinal symptoms (nausea, vomiting). , diarrhea).
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care should be taken when performing potentially hazardous types of work that require increased concentration and speed of psychomotor reaction (including driving a car and operating machinery).
Special instructions for the use of the drug Velaxin
In patients with depression, the likelihood of suicide attempts should be considered before starting any therapy. Therefore, to reduce the risk of overdose, the initial dose of the drug should be as low as possible, and the patient should be under medical supervision. Aggressive behavior of the patient has been reported during the use of venlafaxine (especially at the beginning of the course of treatment and after discontinuation of the drug). The use of venlafaxine is associated with the development of psychomotor agitation, which is characterized by subjectively unpleasant restlessness with a need to move. Most often this occurs during the first weeks of treatment. If such symptoms occur, increasing the dose may not be appropriate, so the question of whether it is advisable to continue taking venlafaxine should be decided. In patients with mood disorders, hypomanic or manic states may occur when treated with antidepressants, including venlafaxine. Velaxin should be prescribed with caution to patients with a history of mania. These patients require medical supervision. Velaxin should be prescribed with caution to patients with a history of epileptic seizures. If epileptic seizures occur, treatment must be stopped. The patient should be warned about the need to immediately consult a doctor if a skin rash, elements of urticaria or other allergic reactions occur. In some patients, during the period of use of venlafaxine, a dose-dependent increase in blood pressure is possible, and therefore it is recommended to regularly monitor blood pressure, especially during the period of dose adjustment or increase. An increase in heart rate is possible, especially when taken in high doses. In this case, medical supervision of the patient's condition is necessary. Occasionally, orthostatic hypotension was observed during use of the drug. Patients, especially the elderly, should be warned about the possibility of dizziness. Velaxin may increase the risk of hemorrhages in the skin and mucous membranes in patients predisposed to these conditions. Patients should be warned about this and advised to exercise caution while using the drug. During the use of Velaxin, especially in conditions of dehydration or decrease in blood volume (including in elderly patients and in patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone is possible. During the period of use of the drug, mydriasis may occur, and therefore it is recommended to monitor intraocular pressure in patients with a tendency to increase it, in patients with angle-closure glaucoma. When treating patients with impaired renal or hepatic function, caution and careful medical monitoring of the patient's condition is necessary (dose reduction is possible). In patients who have recently suffered a myocardial infarction and with signs of decompensated heart failure, the drug should be prescribed with caution under constant medical supervision. The safety and effectiveness of the combined use of venlafaxine and drugs used for weight loss, including phentermine, have not been established, so their simultaneous use is not recommended. With prolonged use of the drug, it is advisable to monitor the level of cholesterol in the blood serum. After stopping the use of Velaxin, especially suddenly, withdrawal syndrome often occurs. The risk of developing withdrawal syndrome depends on the duration of treatment, the dose used, and the rate of dose reduction. With withdrawal syndrome, dizziness, paresthesia, sleep disturbance, agitation, anxiety, nausea, vomiting, tremor, sweating, headache, diarrhea, tachycardia, and emotional disorders appear. These symptoms are usually observed in the first days after discontinuation of the drug and disappear on their own within 2 weeks. Therefore, the drug should be discontinued gradually, reducing the dose of venlafaxine gradually over several weeks or months, depending on the patient's condition. Velaxin does not cause the development of symptoms of tolerance or dependence. Despite this, as with other drugs that act on the central nervous system, patients need to be monitored for signs of drug abuse (especially patients with a history of similar problems). While using Velaxin, women of reproductive age should use adequate methods of contraception. The drug may negatively affect the ability to drive vehicles and operate potentially dangerous machinery. Therefore, doses at which driving vehicles and working with machinery are possible are determined for each patient individually.
Velaxin
Use during pregnancy and breastfeeding
Contraindicated for use during pregnancy and lactation (breastfeeding).
Women of childbearing potential should use reliable methods of contraception during treatment and consult a doctor immediately if they become pregnant or plan to become pregnant.
Venlafaxine and the EDV metabolite are excreted in breast milk. The safety of these substances for newborns has not been proven, therefore, if it is necessary to take venlafaxine during lactation, the issue of stopping breastfeeding should be decided. If the mother's treatment was completed shortly before delivery, the newborn may experience withdrawal symptoms.
Use for liver dysfunction
Contraindicated in severe liver dysfunction.
In case of moderate liver failure (prothrombin time from 14 to 18 seconds), the dose should be reduced by 50%.
Use for renal impairment
Contraindicated in severe renal failure (creatinine clearance < 10 ml/min).
In patients with renal failure with CC 10-30 ml/min, the dose should be reduced by 25-50%. Due to the prolongation of T1/2 of venlafaxine and its active metabolite (EDM), such patients should take the entire dose 1 time/day.
Patients on hemodialysis may receive 50% of the usual daily dose of venlafaxine after completion of the hemodialysis session.
Use in children
Contraindicated in children and adolescents under 18 years of age.
Use in elderly patients
In elderly patients, venlafaxine should be used at the lowest effective dose. When increasing the dose, the patient should be under close medical supervision
Elderly patients should be warned about the possibility of dizziness and impaired balance. While taking venlafaxine, especially in conditions of dehydration or decreased blood volume, hyponatremia and/or syndrome of insufficient ADH secretion may occur in elderly patients
special instructions
Venlafaxine should be used with caution after a recent myocardial infarction, with heart failure in the stage of decompensation, with unstable angina, arterial hypertension, tachycardia, tachyarrhythmia, history of seizures, intraocular hypertension, angle-closure glaucoma, history of manic states, predisposition to bleeding from the skin integuments and mucous membranes, initially reduced body weight.
In patients with depressive disorders, the possibility of suicide attempts should be considered before starting any drug therapy. Therefore, to reduce the risk of overdose, venlafaxine should be used at the minimum effective dose when starting treatment, whenever possible, and the patient should be under close medical supervision.
In patients with affective disorders, when treated with antidepressants (including venlafaxine), hypomanic or manic states may occur. As with other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
If epileptic seizures occur, treatment should be interrupted.
The risk of tachycardia increases when venlafaxine is used in high doses.
During treatment, regular monitoring of blood pressure is recommended, especially during the period of dose adjustment or increase.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient ADH secretion may occur.
Mydriasis may occur while taking the drug, and therefore it is recommended to monitor intraocular pressure in patients prone to increased pressure or suffering from angle-closure glaucoma.
As with other drugs that act on the central nervous system, the physician should closely monitor patients for signs of venlafaxine abuse. Careful monitoring and observation is necessary for patients with a history of such symptoms.
While taking venlafaxine, special care should be taken when conducting electroconvulsive therapy, because There is no experience with the use of venlafaxine in these conditions.
During treatment you should avoid drinking alcohol.
Impact on the ability to drive vehicles and operate machinery
Despite the fact that venlafaxine does not affect psychomotor and cognitive functions, it should be borne in mind that any drug therapy with psychoactive drugs can impair thought processes and reduce the ability to perform motor functions. The patient should be warned about this before starting treatment. If such violations occur, the degree and duration of restrictions must be established by a doctor.
Interactions of the drug Velaxin
The use of Velaxin in combination with MAO inhibitors is contraindicated: tremor, myoclonus, sweating, nausea, vomiting, flushing, dizziness, fever, convulsive seizures, and death are possible. The use of Velaxin can be started no earlier than 14 days after the end of MAO inhibitor therapy. If a reversible MAO inhibitor is used, this interval may be shorter (24 hours). After discontinuation of Velaxin, you should take a break of at least 7 days before starting therapy with MAO inhibitors. Particular caution is required when using Velaxin with drugs that affect the central nervous system. The mutual influence of Velaxin and the following drugs should be taken into account: Lithium: there are reports of interaction between lithium and venlafaxine, as a result of which the level of lithium in the blood increases. Imipramine: the pharmacokinetics of venlafaxine and its metabolite EDV do not change, so a dose reduction of venlafaxine is not required when these drugs are used in combination. Haloperidol: its effect may be enhanced. Diazepam: the pharmacokinetics of the drugs and their main metabolites do not change significantly. Clozapine: an increase in the level of clozapine in the blood and the development of its side effects (for example, epileptic seizures) were noted. Risperidone: with the simultaneous use of these drugs (despite the increase in the AUC of risperidone), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) does not change significantly. Alcohol: depression of psychomotor activity under the influence of alcohol after taking venlafaxine does not increase, however, during the period of use of the drug Velaxin, the consumption of alcoholic beverages is not recommended. Electroconvulsive therapy: when conducting electroconvulsive therapy while taking selective inhibitors of neuronal reuptake of serotonin, an increase in the duration of epileptic activity was noted. It is necessary to exercise caution and ensure careful medical monitoring of the patient's condition when combined with this type of therapy and the use of Velaxin. Drugs metabolized by cytochrome P450 isoenzymes : the CYP 2D6 enzyme of the cytochrome P450 system converts venlafaxine into the active metabolite EDV. Unlike many other antidepressants, the dose of Velaxin does not need to be reduced when used once with drugs that inhibit CYP 2D6 activity, or in patients with a genetically determined decrease in CYP 2D6 activity, since the total concentration of the active substance and metabolite (venlafaxine and ODV) does not change. The main route of elimination of venlafaxine involves metabolism with the participation of CYP 2D6 and CYP 3A4, so special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Venlafaxine is a relatively weak inhibitor of CYP 2D6 and does not inhibit the activity of CYP 1A2, CYP 2C9 and CYP 3A4 isoenzymes; therefore, it should not be expected to interact with other drugs in which these liver enzymes are involved in the metabolism. Cimetidine: inhibits the metabolism of venlafaxine during its initial passage through the liver, but does not have a significant effect on its conversion to EDV or the rate of elimination of EDV, the concentration of which in the circulating blood is much higher. Therefore, there is no need to change the dose of Velaxin and cimetidine when used in combination. This interaction may be more pronounced in elderly patients or with impaired liver function, therefore, in such cases, the combined use of cimetidine and Velaxin requires medical supervision. Antihypertensive and antidiabetic agents: no clinically significant interactions of venlafaxine with antihypertensive (including beta-adrenergic receptor blockers, ACE inhibitors and diuretics) and hypoglycemic agents have been identified. Drugs that bind to plasma proteins: Plasma protein binding is 27% for venlafaxine and 30% for EDV. Therefore, interactions due to their binding to proteins should not be expected. Warfarin: the anticoagulant effect of the latter may be enhanced; at the same time, prothrombin time increases. Indinavir: When used concomitantly with this drug, the pharmacokinetics of indinavir changes (with a 28% decrease in AUC and a 36% decrease in maximum concentration).
Instructions for use VELAXIN® tablets
Suicide/suicidal ideation or clinical worsening
Depression is associated with an increased risk of suicidal ideation, self-harm and suicide (suicide-related events). This risk persists until significant remission occurs. Since improvement may not occur during the first few weeks of treatment or longer, patients should be closely monitored until such improvements occur. Clinical experience suggests a possible increased risk of suicide in the early stages of remission.
Other psychiatric conditions for which venlafaxine is prescribed may also be associated with an increased risk of suicidal events. In addition, these conditions may be comorbid with major depressive disorder. The precautions observed when treating patients with major depressive disorder should also be observed when treating patients with other psychiatric disorders.
It is known that patients with a history of suicidal symptoms who exhibit a significant degree of suicidal ideation before treatment are at greater risk of suicidal ideation and suicide attempts; During treatment, such patients should be closely monitored. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with psychiatric disorders showed an increased risk of suicidal behavior in patients under 25 years of age taking antidepressants compared with age-matched patients taking placebo.
Patients, incl. those at high risk of suicidal ideation and suicide attempts require careful monitoring during drug treatment, especially at the beginning of treatment and when changing doses. Patients (and caregivers) should be warned to monitor for clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek prompt medical attention if these symptoms occur.
Use in children and adolescents under 18 years of age.
Velaxin® immediate release tablets should not be used to treat children and adolescents under 18 years of age. Suicidal behavior (suicide attempt and suicidal ideation) and hostility (primarily aggression, hostile behavior and anger) were observed more frequently in children and adolescents treated with antidepressants compared with those taking placebo in clinical studies. If, despite this, a decision is made to carry out treatment, careful monitoring of the patient is necessary in order to identify suicidal symptoms. In addition, there are no long-term safety data on growth, maturation, and cognitive and behavioral development in children and adolescents.
Serotonin syndrome
As with other serotonergic drugs, venlafaxine may cause serotonin syndrome or neuroleptic malignant syndrome (NMS)-like reactions, a potentially life-threatening condition, particularly when co-administered with other serotonergic drugs (including triptans, serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), amphetamines, lithium preparations, sibutramine, preparations containing St. John's wort ( Hypericum perforatum
), fentanyl and its analogues, tramadol, dextromethorphan, tapentadol, pethidine, methadone and pentazocine), with drugs that inhibit serotonin metabolism (MAO inhibitors, such as methylene blue), with serotonin precursors (for example, with supplements containing tryptophan), and also with other antipsychotic drugs and dopamine antagonists (see sections Contraindications and Drug Interactions).
Serotonin syndrome may include the following symptoms: mental status changes (e.g., psychomotor agitation, hallucinations, coma), autonomic nervous system disturbance (e.g., tachycardia, unstable blood pressure, pyrexia), neuromuscular abnormalities (e.g., hyperreflexia, incoordination), and/or gastrointestinal symptoms (eg, nausea, vomiting, diarrhea).
In its most severe form, serotonin syndrome is similar to NMS, with symptoms such as hyperthermia, muscle rigidity, instability of the autonomic nervous system with possible rapid changes in the patient's vital signs and mental status.
If there is a clinical need for the combined use of venlafaxine with other drugs that affect the serotonergic or dopaminergic neurotransmitter system, it is recommended to carefully monitor the patient's condition, especially at the beginning of treatment and when increasing doses.
Concomitant use of venlafaxine with serotonin precursors (eg, tryptophan-containing supplements) is not recommended.
Narrow-angle glaucoma
Mydriasis may occur in connection with taking venlafaxine. Close monitoring of patients with elevated intraocular pressure or patients at risk of developing angle-closure glaucoma is recommended.
Arterial pressure
A dose-dependent increase in blood pressure is often reported when taking venlafaxine. In the post-marketing period, several cases of severe increases in blood pressure requiring immediate treatment have been observed. Before starting treatment, all patients should undergo a thorough evaluation for high blood pressure, and control of pre-existing hypertension is also necessary. Periodic monitoring of blood pressure is necessary after starting treatment, as well as after increasing the dose. Caution should be exercised when prescribing the drug to patients whose underlying disease may be accompanied by an increase in blood pressure, for example, with impaired cardiac function.
Heartbeat
An increase in heart rate is possible, especially when taking the drug in high doses. Caution should be exercised when prescribing the drug to patients in whom an increase in heart rate may have an adverse effect on the underlying disease.
Heart disease and risk of arrhythmia
There is insufficient experience with the use of venlafaxine in patients who have recently had a myocardial infarction or have unstable cardiac disease. Therefore, it should be used with caution in such patients. In the post-marketing period, cases of QTc prolongation, torsade de pointes (TdP), torsade de pointes (TdP), and fatal cardiac arrhythmias have been observed with venlafaxine, especially in overdose or in patients with risk factors for QTc prolongation or torsade de pointes (see Pharmacology). action). The risk-benefit ratio must be assessed before prescribing venlafaxine to patients at high risk of serious cardiac arrhythmias (see Pharmacological Actions).
Convulsions
During treatment with venlafaxine, seizures may occur. As with all antidepressants, venlafaxine should be used with caution in patients with a history of seizures; such patients should be closely monitored. Treatment with the drug should be discontinued in patients who develop seizures.
Hyponatremia
When taking venlafaxine, cases of hyponatremia and/or syndrome of impaired antidiuretic hormone secretion are possible. This phenomenon was most often observed in patients with hypovolemia or dehydration. Elderly patients, patients taking diuretics, and patients at increased risk of hypovolemia are at greater risk for this phenomenon.
Abnormal bleeding
Medicines that inhibit serotonin reuptake may lead to decreased platelet function. Patients taking SSRIs and SNRIs, including venlafaxine, may have an increased risk of bleeding, ranging from ecchymoses, hematomas, epistaxis and petechiae to gastrointestinal and life-threatening bleeding. Patients receiving venlafaxine may have an increased risk of bleeding. As with other serotonin reuptake inhibitors, venlafaxine should be administered with caution to patients predisposed to bleeding, including patients taking anticoagulants and platelet inhibitors.
Serum cholesterol
In placebo-controlled clinical studies, a clinically significant increase in serum cholesterol was observed in 5.3% of patients receiving venlafaxine and 0.0% of patients receiving placebo for at least 3 months. With long-term use of the drug, it is advisable to monitor the cholesterol level in the blood serum.
Combined use with weight loss agents
Safety and effectiveness of combining venlafaxine with weight loss agents, incl. phentermine, not established. It is not recommended to use venlafaxine and weight loss agents together. Venlafaxine should not be used as a means of weight loss and is not recommended in combination with other drugs.
Mania/hypomania
In a small number of patients with mood disorders receiving antidepressants, incl. and venlafaxine, mania/hypomania may occur. As with other antidepressants, venlafaxine should be prescribed with caution to patients with a personal or family history of bipolar affective disorder.
Aggression
In a small number of patients during treatment with antidepressants, incl. venlafaxine, aggression may occur. These symptoms were observed at the beginning of treatment, with increasing doses and discontinuation of treatment.
As with other antidepressants, venlafaxine should be prescribed with caution to patients with a history of aggression.
Stopping treatment
After stopping treatment (especially abruptly), withdrawal symptoms often appear (see section Side effects). In clinical studies, adverse events observed after treatment discontinuation (dose taper and post-dose reduction) occurred in approximately 31% of patients receiving venlafaxine and 17% of patients receiving placebo.
The risk of withdrawal symptoms may depend on several factors, including: on the duration of treatment and doses used, as well as the rate of dose reduction. Dizziness, sensory disturbances (including paresthesia), sleep disturbances (including insomnia and vivid dreams), psychomotor agitation or anxiety, nausea and/or vomiting, tremor and headache are the most common reactions. In general, these symptoms are mild or moderate, however, in some patients they can be severe.
Typically, symptoms appear within the first few days after stopping treatment, but in very rare cases, similar symptoms have been reported in patients who accidentally missed a dose. These symptoms usually go away on their own, usually within 2 weeks, but in some patients they may persist for a longer period of time (2-3 months or more). Therefore, if it is necessary to discontinue treatment, it is recommended to gradually reduce the dose (over several weeks or months, depending on the patient's response (see Dosage Regimen).
Akathisia/psychomotor restlessness
The use of venlafaxine is associated with the development of akathisia, characterized by a subjectively unpleasant and disturbing restlessness for the patient, with a need to move, often combined with the inability to sit or stand still. This is most likely to occur during the first few weeks of treatment. In patients with such symptoms, increasing the dose may have an adverse effect.
Dry mouth
Dry mouth occurs in 10% of patients receiving venlafaxine. This may increase the risk of dental caries and patients should be advised of the importance of dental hygiene.
Diabetes
In patients with diabetes mellitus, the use of selective serotonin reuptake inhibitors or venlafaxine may lead to changes in glycemic control. It may be necessary to change the dose of insulin and/or oral antidiabetic medications.
Sexual dysfunction
SSRIs and SNRIs can cause sexual dysfunction. There have been reports of long-term impairment of sexual function despite discontinuation of SSRIs or SNRIs.
Impact on the results of laboratory tests for the presence of narcotic drugs
False-positive urine immunoassay results for phencyclidine (PCP) and amphetamine have been observed in patients receiving venlafaxine. This is due to the lack of specificity of immunotests. False-positive test results are possible several days after venlafaxine is discontinued. Confirmatory tests such as gas chromatography or mass spectrometry can differentiate venlafaxine from phenylcyclidine and amphetamine.
Velaxin® tablets contain lactose
Patients with rare hereditary diseases such as galactose intolerance, complete lactase deficiency and glucose/galactose malabsorption should not take this drug.
Sodium content
All Velaxin® tablets with varying levels of active substance contain less than one millimole (23 mg) of sodium, so the tablets are practically sodium-free.
Preclinical safety studies
Studies of venlafaxine in rats and mice showed no evidence of tumorigenesis. In numerous in vitro
and
in vivo
, venlafaxine demonstrated no mutagenicity.
Reproductive toxicity studies in animals have shown decreased body weight of pups, increased rates of stillborn pups, and increased pup mortality during the first 5 days of lactation. The cause of these deaths is unknown. These effects were observed at a dose of 30 mg/kg/day, which is 4 times higher than the daily dose of venlafaxine for humans - 375 mg (based on mg/kg). The dose at which these effects were absent is 1.3 times the human dose. The potential risk to humans is unknown.
Decreased fertility was observed in a study in which both male and female rats were given EFA. The dose administered in this case was approximately 1-2 times higher than the human dose of 375 mg/day. The clinical significance of this interaction is unknown.
Impact on the ability to drive vehicles and operate machinery
Any psychotropic drug can affect thinking, judgment and motor skills. Therefore, patients receiving venlafaxine should be warned about the possible effect of the drug on their ability to drive vehicles or operate dangerous machinery.
Velaxin overdose, symptoms and treatment
Symptoms: ECG changes (increased QT , bundle branch block, expansion of the QRS ), sinus and ventricular tachycardia, bradycardia, hypotension, convulsions, impaired consciousness. In some cases, fatalities due to overdose have been reported when high doses of venlafaxine were taken concomitantly with alcohol and/or other psychotropic drugs. Treatment: there is no specific antidote. Gastric lavage and the use of activated carbon are indicated. Inducing vomiting is not recommended. It is necessary to ensure airway patency, adequate ventilation and oxygenation. Monitoring of ECG and vital body functions is recommended, as well as supportive and symptomatic therapy. In case of overdose, the possibility of the patient taking several psychotropic drugs simultaneously should be taken into account. Venlafaxine and EDV are not eliminated by dialysis.