"Amitriptyline": main characteristics
The main component of the drug is the substance of the same name, amitriptyline (for better absorption, it is presented in the form of hydrochloride). Available in 3 forms:
- Tablets (each containing 10 mg or 25 mg of amitriptyline).
- Dragee (same dosage).
- Solution for injections (10 mg of amitriptyline per 1 ml volume).
According to its effects on the body, it is classified as a tricyclic antidepressant. Gives a sedative and thymoleptic effect, also acts as an analgesic (as an additional remedy).
Tablets, dragees and containers with solutions are dispensed only with a prescription. They are stored under normal room conditions (temperature no higher than 25 degrees, moderate humidity) within the general shelf life (3 years from the date of production).
Obesity in patients with severe mental disorders
Share with friends
Treatment of severe mental disorders in individuals with obesity (previous or induced by therapy) is a complex clinical problem in modern psychiatry. Unfortunately, many effective psychotropic drugs promote weight gain, which often forces patients to resort to surgical correction. According to leading experts, first-line drugs for drug treatment of mental disorders in obese individuals must meet criteria such as high efficiency for a specific nosological form, a good safety profile, optimal tolerability, weight neutrality or induction of weight loss.
If it is necessary to prescribe medications that stimulate weight gain, it is recommended to change the eating behavior strategy, use methods aimed at weight loss, and, if ineffective, alternative drug correction.
The article by S. L. McElroy, “Obesity in patients with severe mental illness: overview and management,” published in the Journal of Clinical Psychiatry (2009; 70 (3): 1221), describes currently known factors predisposing to obesity, as well as methods of control. and weight correction when taking various psychotropic drugs.
An increase in the proportion of obesity and overweight in the general population, according to US health services (NHANES), has been observed since the 90s. and tends to further increase. In addition, overweight/obesity is particularly common in individuals with severe mental illnesses such as schizophrenia and bipolar disorder.
It is known that obesity, accompanied by an imbalance of energy intake and expenditure and an increase in the volume of adipose tissue, is a risk factor for the development of a number of diseases and pathological conditions, such as type 2 diabetes mellitus, cardiac and cerebral dyshemia (cerebrovascular disorders, coronary heart disease, peripheral vascular diseases) , dyslipidemia, arterial hypertension, impaired glucose tolerance, cancer. The volume of intra-abdominal and visceral adipose tissue (to a greater extent than subcutaneous adipose tissue) correlates with cardiovascular and metabolic disorders that accompany obesity. An increase in the volume of intra-abdominal adipose tissue is regarded as abdominal obesity with an increase in waist circumference of more than 88 cm for women and more than 102 cm for men.
The results of clinical studies indicate that more than 60% of patients with schizophrenia or bipolar disorder are overweight. Thus, the results of a comparative study involving 169 individuals (48% of individuals with schizophrenia and 52% with major depressive disorder) and data from a survey of 2404 subjects of the general population, identical in gender, age and race (according to NHANES), demonstrated that excess body weight was significantly more common in patients with mental illness (50% of women and 41% of men). Data from a similar trial of 86,028 individuals (USO) showed a higher incidence of obesity (41%) in patients with bipolar disorder than in those without mental disorders (27%, p = 0.002).
Despite the fact that most studies included individuals taking psychotropic drugs, there are a number of reports of weight disturbances in patients with newly diagnosed mental disorders, as well as in the absence of drug correction (in particular, abdominal obesity was observed in patients with schizophrenia and overweight in those with bipolar disorder). Thus, an examination of 17 patients with a primary episode of schizophrenia who had not previously received pharmacological correction indicated a significant increase in the volume of intra-abdominal adipose tissue in comparison with patients in the control group, matched by gender, age and body mass index. In addition, according to Italian researchers, 41% of untreated individuals with bipolar disorder were overweight or obese to varying degrees, which significantly exceeded the percentage of such weight disorders in patients with obsessive-compulsive disorder (11%).
Thus, a large-scale study conducted in Finland confirmed previously obtained results - the association of schizophrenia or schizoaffective disorders with obesity and decreased muscle mass, according to a survey of 8082 individuals, had a high frequency in comparison with healthy individuals. At the same time, the influence of the volume and quality of antipsychotic therapy, diet, level of education and the presence of bad habits, in particular smoking, was also noted. Canadian researchers came to similar conclusions, revealing a connection between obesity, as well as bipolar and major depressive disorders in 19% of patients compared with persons without mental status disorders. In reports from American scientists who conducted a large-scale (41,654 respondents) data analysis
The US National Epidemiological Service, the combination of obesity with a number of mental disorders accompanied by manic episodes, indicated the presence of a large percentage of high-grade obesity. According to the results of analytical studies, the frequency of conditions associated with obesity, such as cardiovascular disorders and type 2 diabetes mellitus, is correspondingly increasing in this group of patients.
According to available reports, metabolic syndrome in patients receiving therapy aimed at correcting the manifestations of bipolar disorder was observed in at least 25% of the subjects, which is significantly more than in the general population (14%, p = 0.013). Increases in body mass index, triglyceride levels, and decreases in high-density lipoprotein cholesterol concentrations occurred in the group of individuals with mental illness.
At the same time, a reduction in life expectancy was noted, and cardiovascular disorders became the most common cause of death in patients.
The conditions and diseases most often associated with obesity include:
- oncological diseases of various localizations (chest, bladder, cervix, intestines, esophagus, pancreas, kidneys, prostate);
- cardiovascular diseases (coronary heart disease, stroke, peripheral vascular disease);
- dermatological diseases (infectious diseases, dermatitis);
- endocrine disorders (type 2 diabetes mellitus, dyslipoproteinemia, metabolic syndrome);
- gynecological diseases and disorders (menstrual cycle disorders, infertility, polycystic ovary syndrome, unfavorable course of pregnancy);
- lung diseases (hypoventilation syndrome, sleep apnea);
- other diseases (osteoarthritis, gout, cholelithiasis, liver adiposis, arterial hypertension, phlebitis, pancreatitis).
Predisposing factors for obesity
Recently, the attention of scientists has been drawn to the identification of a connection between the composition of antipsychotic therapy and the development of obesity.
It has been observed that long-term use of drugs such as clozapine, olanzapine, risperidone or amisulpride often leads to weight gain. This is supported by data from two large studies indicating that treatment with atypical antipsychotic drugs increases the risk of developing abdominal obesity.
An increase in the degree of obesity from 25 to 36% during the first 4 weeks of intensive treatment for bipolar disorder was noted by South Korean researchers who presented data from a survey of 179 patients.
However, atypical antipsychotics contributed more to weight gain than typical antipsychotics and mood stabilizers. Patients receiving combination therapy with atypical antipsychotics or mood stabilizers (eg, olanzapine and valproate) had the highest incidence of reported obesity.
In addition, an analysis of a significant number of cases of obesity in people with schizophrenia and bipolar disorder showed that overweight is more often recorded in women (72%) than in men (37%), and in people who do not adhere to the principles of a healthy lifestyle, and also with an unbalanced diet.
Among the various groups of psychotropic drugs, antipsychotics have the greatest effect on weight. Clozapine, olanzapine, quetiapine, risperidone, thioridazine and chlorpromazine are associated with weight gain, whereas ziprasidone, aripiprazole, haloperidol, fluphenazine, molindone and perphenazine do not.
Antidepressants such as fluoxetine and bupropion may have an effect on weight, sertraline, nefazodone, duloxetine, citalopram, escitalopram and venlafaxine do not affect weight, and amitriptyline, nortriptyline, imipramine, mirtazapine and paroxetine may contribute to obesity.
Among anticonvulsants and mood stabilizers, the weight-neutral drugs lamotrigine and oxcarbazepine, topiramate, and zonisamide are associated with weight loss, and valproate, carbamazepine, gabapentin, and lithium are associated with weight gain.
Ways to control and monitor weight
Most currently available guidelines for the management of persons with mental disorders include weight control and identification of obesity-associated conditions and diseases.
Monitoring includes recording body mass index, waist circumference, lipid profile, and blood glucose levels, especially in patients receiving antipsychotic drug therapy. Some experts recommend determining body mass index before initiating therapy or correcting a previous regimen, and subsequently at each patient visit during the first 6 months of treatment.
A sharp increase in body weight during the first month of therapy is a predictor of the accumulation of excess weight in the future. When the body mass index stabilizes within 6 months, it is monitored quarterly.
Behavioral correction of weight loss
Prevention and treatment of obesity involves behavioral interventions aimed at achieving three main goals, such as reducing caloric intake, increasing physical activity, and learning cognitive behavioral strategies to reinforce positive changes related to diet and training. The effectiveness of this technique is confirmed by recent studies that found significant reductions in body weight in people with schizophrenia who used corrective behavioral weight loss methods. According to DSM criteria, in the trials, at least 75% of patients had schizophrenia-like disorders and were treated with cognitive behavioral therapy, dietary changes, and exercise to improve their weight. Training in these techniques was both group and individual.
The results showed a statistically significant reduction in weight in the groups that used these methods, which was reflected by changes in body mass index. The difference in weight between individuals in the group that combined psychotropic therapy with non-pharmacological correction and patients who received only drug treatment averaged 2.6 kg (95% confidence interval, p < 0.001), according to body mass index - 0.9 kg/m2 (p < 0.001). This led to the conclusion that behavioral modification is an effective method of weight loss in individuals receiving antipsychotic drugs.
Diet and exercise
Recent placebo-controlled studies have demonstrated that omega-3 fatty acid supplementation has a beneficial effect on treatment-resistant mental illnesses such as bipolar disorder, major depressive episode, and possibly schizophrenia. Earlier observations supported the use of a diet high in vegetables, fruits, whole grains and low amounts of animal fats.
One of the effective weight loss systems developed for patients suffering from schizophrenia and schizoaffective disorders is a nutritional replacement program, which involves a weekly cash payment for a conscious choice of dietary components: vegetables, fruits, low-fat foods, whole grain bread, cereals, lean meat and poultry. . Appetizer and dessert selections were not refundable. The results of the implementation of this program were a decrease in the patients’ body weight and stabilization of blood glucose levels, which persisted for 6 months after the end of the program.
Small controlled trials have examined the effectiveness of exercise for the treatment of obesity in people with severe mental disorders. Thus, in one of them, in 53 patients with schizophrenia who were prescribed clozapine, it was possible to achieve a decrease in body weight when included in a therapeutic program of diet and physical training lasting one hour three times a week.
Similar results were obtained by Australian specialists who studied the effect of physical activity and diet on weight stabilization in people with bipolar disorders, schizophrenia and schizoaffective disorders. They found that patients who completed individually designed training programs had significantly lower weight, body mass index and waist circumference compared to the control group, where not only the values of these indicators increased, but also the levels of low-density lipoprotein cholesterol and triglycerides.
Effect of drugs on body weight
Antipsychotics It is now known that a number of antipsychotics are weight-neutral and can be used in this group of patients as an alternative correction (by replacing olanzapine and risperidone, which affect weight gain, with ziprasidone and ariprazole). In addition, according to a number of authors, such changes in the therapeutic regimen have a positive effect on the state of lipid metabolism.
Antidepressants In studies devoted to a detailed assessment of the effects of modern antidepressants, it was found that taking fluoxetine and bupropion leads to a decrease in the body weight of patients (especially when combining bupropion with naltrexone). One trial showed a positive effect of reboxetine compared with placebo in reducing weight in patients with schizophrenia (after 8 weeks of therapy).
Anticonvulsants Anticonvulsants such as topiramate, zonisamide and lamotrigine can induce weight loss in persons with severe mental disorders. Thus, according to research results, taking topiramate as monotherapy significantly reduced weight in patients with bipolar disorders, and as part of combination therapy in patients with schizoaffective disorder. The daily dose of topiramate was 100200 mg/day. Topiramate combined with risperidone or olanzapine prevented weight gain in bipolar disorder patients, according to two reports. However, according to the results of two observations, taking zonisamide as an additional therapy, although it led to the desired weight loss, but significantly reduced the effectiveness of basic treatment with antipsychotics and mood stabilizers, which in both cases required its discontinuation.
Adjunctive pharmacotherapy A number of drugs with stimulant effects, such as methylphenidate, can lead to decreased appetite and weight loss, some of which, particularly phentermine, diethylpropion, benzphetamine, and phendimetrazine, are approved by the FDA as acceptable short-term therapy for weight management, but not recommended for patients with mental disorders and obesity. Dopamine agonists that reduce weight (bupropion) and relieve symptoms of depression in people with bipolar disorder (pramipexole) are also not currently approved by the FDA.
The selective serotonin and norepinephrine reuptake inhibitor sibutramine was effective as an adjunctive therapy against weight gain in individuals with schizophrenia and schizoaffective disorder, according to a double-blind, placebo-controlled study.
The results of the 12-week therapy were a decrease in weight, waist circumference and glycosylated hemoglobin levels. The lipase inhibitor orlistat, which was studied in a 12-week study, did not influence weight loss or eliminate metabolic changes in women receiving clozapine or olanzapine, although the study authors noted a significant decrease in body weight in men.
Controlled trials of the effects of metformin demonstrated its positive effect on carbohydrate metabolism and some weight loss in patients (including children) with severe mental disorders who were treated with antipsychotics (olanzapine, risperidone, quetiapine).
In addition, they were well tolerated.
A randomized, placebo-controlled trial found that the H2 receptor antagonist nizatidine promoted weight loss in patients receiving olanzapine. However, these data have not been confirmed in subsequent trials.
Prepared by Evgeniya Solovyova
Source:
Share with friends
Indications for use
"Amitriptyline" is prescribed by a doctor in the presence of depressive conditions associated with the following manifestations:
- sleep disorders;
- agitation (restlessness);
- high level of anxiety;
- withdrawal syndrome in alcoholism;
- nocturnal enuresis;
- emotional instability;
- organic lesions of brain tissue.
The product is also used to treat such pathologies;
- nocturnal enuresis;
- postherpetic neuralgia;
- severe pain;
- migraine;
- bulimia nervosa;
- ulcers of the digestive system.
Contraindications
The drug is not approved for use in the presence of the following diseases and characteristics:
- myocardial infarction;
- individual characteristics (intolerance to the active substance);
- angle-closure glaucoma;
- poisoning with certain drugs (sleeping pills, analgesics);
- taking psychoactive substances;
- severe alcohol poisoning;
- breastfeeding (any period);
- disorder of bone marrow hematopoiesis.
In some cases, Amitriptyline can be taken, but only with caution:
- bronchial asthma;
- digestive system disorders;
- stroke;
- dysfunction of the liver, kidneys;
- increased pressure inside the eye;
- pregnancy (any stages);
- epilepsy;
- urinary retention.
Description of the drug AMITRIPTILINE
Use with caution in cases of coronary artery disease, arrhythmia, heart block, heart failure, myocardial infarction, arterial hypertension, stroke, chronic alcoholism, thyrotoxicosis, during therapy with thyroid drugs, and with impaired liver and/or kidney function.
During amitriptyline therapy, caution is required when suddenly moving to a vertical position from a lying or sitting position.
If you stop taking it abruptly, withdrawal syndrome may develop.
Amitriptyline in doses of more than 150 mg/day reduces the seizure threshold; the risk of developing epileptic seizures in predisposed patients should be taken into account, as well as in the presence of other factors that increase the risk of developing convulsive syndrome (including brain damage of any etiology, simultaneous use of antipsychotic drugs, during the period of ethanol withdrawal or drug withdrawal, having anticonvulsant activity).
It should be taken into account that patients with depression may experience suicide attempts.
Should only be used in combination with electroconvulsive therapy under close medical supervision.
In predisposed patients and elderly patients, it can provoke the development of drug-induced psychoses, mainly at night (after discontinuation of the drug, they disappear within a few days).
May cause paralytic ileus, primarily in patients with chronic constipation, the elderly, or those forced to bed rest.
Before performing general or local anesthesia, the anesthesiologist should be warned that the patient is taking amitriptyline.
With long-term use, an increase in the incidence of caries is observed. The need for riboflavin may increase.
Amitriptyline can be used no earlier than 14 days after discontinuation of MAO inhibitors.
Should not be used simultaneously with adrenergic and sympathomimetics, incl. with epinephrine, ephedrine, isoprenaline, norepinephrine, phenylephrine, phenylpropanolamine.
Use with caution simultaneously with other drugs that have anticholinergic effects.
Avoid drinking alcohol while taking amitriptyline.
Impact on the ability to drive vehicles and machinery
During the treatment period, you should refrain from potentially hazardous activities that require increased attention and rapid psychomotor reactions.
Side effects of Amitriptyline
While taking the drug, side effects associated with disorders of various organ systems may occur:
- pulse disturbance;
- problems with urination;
- dry mouth;
- headaches;
- increased drowsiness;
- anxiety;
- hypomanic states;
- increased depression;
- increased epilepsy attacks;
- blood pressure surges;
- diarrhea;
- taste disturbances;
- heartburn;
- problems with potency;
- swelling of the testicles;
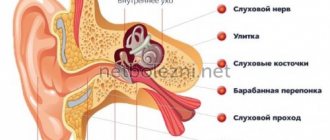
- ringing in the ears and others.
If the drug is discontinued, there may also be negative consequences associated with sleep disturbances, overexcitation, anxiety, and increased levels of irritability.
"Amitriptyline" tablets: instructions for use
When determining the normal dosage, the stage of treatment, the characteristics of the patient’s condition and the form of the drug are taken into account:
- At the first stage, adult patients are given from 25 to 50 mg of the active substance (taken at night).
- Then, over the course of 5 days, the norm is increased to a maximum of 200 mg, and taken 3 times a day.
- If the effect does not occur within 14 days, then the norm is increased to 300 mg.
In the case of a solution, the dosage ranges from 20 to 40 mg at a time (the total number of injections is 4 per day). Then the patient switches from injections to tablets. The general course of treatment lasts a maximum of 8 months in a row.
Attention!
For the treatment of headaches, migraines, and chronic pain syndromes, the dosage can be set in the range from 12.5 mg to 100 mg every day.
How to take Amitriptyline
Amitriptyline should be taken exactly as prescribed by your doctor. If you have any doubts, you should consult your doctor or pharmacist.
Not all dosage regimens are possible with different dosage forms and doses of the drug.
The appropriate dosage form and dose of the drug should be selected for the starting and subsequent increasing doses.
Depression
Adults:
The recommended starting dose is 25 mg twice daily. Depending on the clinical effect, the dose may be increased to 150 mg/day, divided into two doses.
Elderly patients (over 65 years of age) and patients with cardiovascular diseases
The recommended starting dose is 10-25 mg per day. Depending on the clinical effect, the dose may be increased to 100 mg/day, divided into two doses. If you take 100 mg to 150 mg of the drug, you may need to consult your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for use in children and adolescents for the treatment of depression. For more information see section 2.
tension headaches and migraine prevention
Your doctor will choose the right dose based on your symptoms and your body's response to treatment.
Adults:
The recommended starting dose is 10-25 mg in the evening.
The recommended daily dose is 25-75 mg.
Depending on the clinical effect, the dose may be gradually increased. If you take more than 100 mg/day, you may need to consult your doctor more often. Your doctor will advise you to take the drug once a day or divide the dose into two doses.
Elderly patients (over 65 years of age) and patients with cardiovascular diseases
The recommended starting dose is 10-25 mg in the evening.
Depending on the clinical effect of the drug, the dose may be gradually increased.
If you take more than 75 mg/day, you may need to consult your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for use by children and adolescents for the treatment of neuropathic pain, chronic tension-type headaches, and for the prevention of migraine. For more information, see the section What you need to know before using Amitriptyline.
Bed-wetting
Use in children and adolescents
Recommended dose for children:
- Children under 6 years of age: See section “Do not take Amitriptyline tablets”
- Children from 6 to 10 years: 10-20 mg per day. In this age group, appropriate release forms are used.
- Children 11 years and older: 25-50 mg.
The dose should be increased gradually.
You should take the drug 1 or one and a half hours before bedtime.
Before starting treatment, your doctor may perform an ECG to determine if there are signs of a heartbeat abnormality.
Your doctor will re-evaluate your condition after 3 months of treatment and perform a repeat ECG if necessary.
Do not stop taking the drug without consulting your doctor.
Special patient groups
Patients with liver disease or known to be "poor metabolizers" are usually prescribed lower doses.
Your doctor may take blood samples to determine your amitriptyline level (see What you need to know before you use Amitriptyline).
How and when to take Amitriptyline
The drug should be taken during or after meals.
The tablets should be swallowed whole with water. The tablets should not be chewed.
Treatment period
You should not change the dose of the drug or stop taking the drug without consulting your doctor.
Depression
As with other medications used to treat depression, it may take several weeks before you feel any improvement in your condition.
When treating depression, the duration of treatment is individual and is usually at least 6 months. The duration of treatment is determined by your attending physician.
Continue taking Amitriptyline for as long as prescribed by your doctor. The disease can persist for a long time. If you stop treatment too early, your symptoms may return.
tension headaches and migraine prevention
It may take several weeks for your condition to improve.
Consult your doctor about the duration of treatment and continue taking the drug until your doctor stops it.
Bed-wetting
Your doctor will determine the need to continue treatment after 3 months of taking the drug.
If you take more Amitriptyline than recommended
If you take more Amitriptyline than prescribed by your doctor, you should immediately contact your doctor or the nearest hospital emergency room, even if you do not experience any discomfort or symptoms of poisoning. Take the medicine package with you if you are going to the doctor or hospital.
Overdose symptoms include:
- dilated pupils
- fast or irregular heartbeat
- difficulty urinating
- dry mouth or tongue
- intestinal obstruction
- seizures
- fever
- anxiety
- confusion
- hallucinations
- involuntary movements
- low blood pressure, weak pulse, pallor
- difficulty breathing
- bluish skin
- decreased heart rate
- drowsiness
- loss of consciousness
- coma
- various heart diseases, such as cardiac conduction block, heart failure, hypotension, cardiogenic shock, metabolic acidosis, hypokalemia.
If you forget to take Amitriptyline
Take your next dose at your usual time. Do not take a double dose of the drug to compensate for the missed dose.
If you stop taking Amitriptyline
Your doctor will decide when and how to stop treatment to avoid unwanted symptoms that may occur if the drug is suddenly stopped (for example, headache, feeling unwell, insomnia and irritability).
If you have additional questions about the use of the drug, contact your doctor or pharmacist.
Cases of overdose
It has been established that due to an overdose, disorders of the nervous system are observed, which leads to the following consequences:
- anxiety;
- falling into a coma, stupor;
- epileptic seizures;
- ataxia;
- appearance of hallucination;
- surges in blood pressure and pulse;
- vomiting, symptoms of poisoning.
- in extremely rare cases, cardiac arrest.
For treatment, urgent gastric lavage and taking appropriate medications are indicated (symptomatic treatment).
special instructions
During the course of treatment, the patient is advised to regularly monitor blood pressure levels (even if there were no problems with the cardiovascular system before). The medicine is intended only for inpatient treatment under medical supervision. In the first days, bed rest is observed. During therapy, you must completely abstain from alcoholic beverages.
The dosage of the medication is increased and decreased gradually. An abrupt stop leads to withdrawal syndrome. This is expressed in manic states during the development of depression and other behavioral disorders. If the course lasts several months, caries may develop - a dental examination is required.
Amitriptyline
Concomitant use of amitriptyline and MAO inhibitors can cause serotonin syndrome (agitation, confusion, tremor, myoclonus, hyperthermia are possible).
Amitriptyline can be prescribed 14 days after stopping treatment with irreversible MAO inhibitors and at least 1 day after stopping therapy with the reversible MAO type A inhibitor, moclobemide. MAO inhibitors can be prescribed 14 days after stopping amitriptyline.
Amitriptyline may enhance the effects of alcohol, barbiturates and other CNS depressants.
Since tricyclic antidepressants, including amitriptyline, can enhance the effect of anticholinergic drugs on the organs of vision, central nervous system, intestines and bladder, their simultaneous use should be avoided due to the risk of developing paralytic ileus and hyperpyrexia.
When taking tricyclic antidepressants in combination with anticholinergic drugs or antipsychotics, especially in hot weather, hyperpyrexia may develop.
Amitriptyline may enhance the cardiovascular effects of epinephrine, ephedrine, isoprenaline, norepinephrine, phenylephrine and phenylpropanolamine; therefore, anesthetics, decongestants and other drugs containing these substances should not be used simultaneously with amitriptyline.
May reduce the antihypertensive effect of guanethidine, betanidine, reserpine, clonidine and methyldopa.
When taking tricyclic antidepressants simultaneously, it is necessary to adjust antihypertensive therapy.
When used together with antihistamines (clonidine), the inhibitory effect on the central nervous system may be enhanced; with drugs that cause extrapyramidal reactions - an increase in the severity and frequency of extrapyramidal effects.
Concomitant use of amitriptyline and drugs that prolong the QT interval (antiarrhythmics (quinidine), antihistamines (astemizole and terfenadine), some antipsychotics (cisapride, halofantrine and sotalol, especially pimozide and sertindole)) increases the risk of developing ventricular arrhythmia.
Antifungal drugs, for example, fluconazole, terbinafine, increase the concentration of tricyclic antidepressants in the blood serum and, accordingly, their toxicity.
Possible fainting and the development of paroxysms of ventricular tachycardia ( Torsade de Pointes
).
Barbiturates and other enzyme inducers, such as rifampicin and carbamazepine, can increase the metabolism of tricyclic antidepressants, and as a result, reduce the concentration of tricyclic antidepressants in the blood plasma and reduce their effectiveness.
When amitriptyline is used together with phenytoin, the metabolism of the latter is inhibited, and the risk of its toxic effects (ataxia, hyperreflexia, nystagmus, tremor) increases.
When starting the use of amitriptyline in patients receiving phenytoin, the concentration of the latter in the blood plasma should be monitored due to an increased risk of inhibition of its metabolism. At the same time, the therapeutic effect of amitriptyline should be monitored, because your dose may need to be increased.
Preparations of St. John's wort reduce the AUC0-12 hours and the maximum concentration of amitriptyline in the blood plasma by approximately 20% due to the activation of the hepatic metabolism of amitriptyline by the CYP3A4 isoenzyme.
This combination can be used with amitriptyline dose adjustment depending on the results of measuring its concentration in the blood plasma.
With simultaneous use of valproic acid, the clearance of amitriptyline from blood plasma decreases, which can lead to an increase in the concentration of amitriptyline and its metabolite, nortriptyline. When co-administering amitriptyline and valproic acid, serum concentrations of amitriptyline and nortriptyline should be monitored. Amitriptyline dose reduction may be required.
When used simultaneously with cimetidine, methylphenidate and calcium channel blockers, it is possible to slow down the metabolism of amitriptyline, increase its concentration in the blood plasma and develop toxic effects.
When co-prescribed with antipsychotics, it should be taken into account that tricyclic antidepressants and antipsychotics mutually inhibit each other's metabolism, reducing the threshold for convulsive readiness.
With the simultaneous use of amitriptyline and indirect anticoagulants (coumarin or indadione derivatives), the anticoagulant activity of the latter may increase.
Amitriptyline may enhance depression caused by glucocorticoids (GCS).
When used together with anticonvulsants, it is possible to enhance the inhibitory effect on the central nervous system, reduce the threshold of convulsive activity (when used in high doses) and reduce the effectiveness of the latter.
Concomitant use with drugs for the treatment of thyrotoxicosis increases the risk of developing agranulocytosis.
Due to the risk of arrhythmias, special caution must be exercised when prescribing amitriptyline to patients with hyperthyroidism or patients receiving thyroid medications.
Fluoxetine and fluvoxamine may increase plasma concentrations of amitriptyline (a dose reduction of amitriptyline may be required).
When used together with anticholinergic blockers, phenothiazines and benzodiazepines, a mutual enhancement of the sedative and central anticholinergic effects and an increased risk of epileptic seizures (lowering the threshold of convulsive activity) is possible.
Estrogen-containing oral contraceptives and estrogens may increase the bioavailability of amitriptyline. A dose reduction of either estrogen or amitriptyline may be necessary to restore efficacy or reduce toxicity. However, discontinuation of estrogen-containing oral contraceptives may be necessary. In this case, it is necessary to discuss the possibilities of contraception with your gynecologist.
Concomitant use with disulfiram and other acetaldehydrogenase inhibitors may increase the risk of developing psychotic conditions and confusion.
With the simultaneous use of amitriptyline in a high dose and lithium preparations for more than six months, the development of seizures and cardiovascular complications is possible. It is also possible that signs of a neurotoxic effect may occur in the form of tremor, memory impairment, distractibility, disorganization of thinking, even with normal lithium concentrations in the blood and average doses of amitriptyline.