20.07.2018
The author of the article is Dakhno L.A. Candidate of Medical Sciences, dental surgeon, radiologist.
Post-traumatic neuropathy of the trigeminal system is a sensory disturbance with or without neuropathic pain, often leading to functional and psychological consequences.
The trigeminal nerve is the largest sensory nerve in the body and is responsible for the orofacial region. Iatrogenic injuries of the trigeminal nerve (trigeminal nerve injuries -TNI) lead to pain in 70% of patients, which in turn leads to functional impairments in speech, eating, kissing, shaving, applying makeup, brushing teeth, etc., which means there is a negative impact on self-esteem, quality of life and patient psychology.
It must be understood that after injury to the trigeminal nerve, complete recovery is rare, except in cases of minor injury, so it is very important to maintain a trusting relationship between the dentist and the patient and not give false assurances of a complete recovery.
Nerve damage can occur during any dental procedure: injections of local anesthesia, wisdom tooth extraction, endodontic treatment, as well as at all stages of implantation - from the administration of anesthetic and preparation of the implant bed to implantation, bone augmentation and/or soft tissue swelling after surgery .
Rice. 1 Clinical case. CBCT computed tomography images show fragments of sealer that are directly adjacent to the lumen of the mandibular canal in the area of the mental foramen. The patient complained of paresthesia and pain from touch and wind in the area of the chin and lower lip on the left, which appeared after endodontic treatment of the 34th tooth. After 6 months - paresis (motor disorder) of the left half of the lower lip, which led to the inability to fully drink and eat (the patient holds the lip with her fingers while eating to prevent food and liquid from falling out of the mouth) and, as a result, a stress disorder accompanied by anxiety, fear and fits of anger.
Fig. 2. Removal of the sealer into the mandibular canal due to the absence of an apical stop
Regarding implantation, pain during bone preparation with a pilot drill can be an indicator of the proximity of the nerve and, if this is not addressed immediately (deciding to place a shorter implant), permanent nerve damage can occur.
Nerve injury during implantation is associated primarily with preoperative factors, including poor preoperative planning, which leads to inaccurate measurements and incorrect selection of implantation site and implant type (diameter and length).
Figure 3a. Planning error.
Figure 3b. Incorrect choice of implant length.
Figure 3-a, b. CBCT images from two clinical cases demonstrate implantation-related nerve damage. The implants are inserted directly into the canal of the inferior alveolar nerve, which is associated with errors in preoperative planning.
The habit of carefully planning implantation based on computed tomography data, performing implantation under infiltration anesthesia using surgical guides, performing intraoperative X-ray control and using drill stops (drill stops) can minimize possible nerve injury during implantation.
Any injury (penetration or compression) as well as hemorrhage into the mandibular canal results in acute and often severe intraoperative pain of the neuralgic type and it is imperative that the physician use an appropriate protocol of infiltration local anesthesia so that the patient can indicate the proximity of surgical instruments to the mandibular canal .
Since implantation is the surgery of choice, nerve injury, which leads to potentially irreversible consequences even after repeated surgery (implant removal), can always be avoided.
The physiological consequences of sensory nerve damage are immediate and often irreversible. The inferior alveolar nerve passes through the bony canal, which may be subject to compression and ischemic damage. Compression of peripheral sensory nerves for 6 hours can cause nerve fiber atrophy.
Ischemia itself, even without direct nerve damage, will cause sufficient inflammation and nerve damage that may result in permanent nerve damage.
Figure 4. Sagittal CBCT sections demonstrate an acceptable relationship between the implant and the lumen of the inferior alveolar nerve canal, but the clinical picture is consistent with ischemia, which caused pain and paresthesia. During the first 24 hours, a clinical decision was made to remove the implant and prescribe medication.
Three months after injury to the inferior alveolar nerve, permanent changes in the nervous system, both central and peripheral, will occur, which are unlikely to respond to surgical treatment or respond to drug treatment and peripheral interventions.
When nerve injury occurs, the clinician must be able to recognize the type and extent of injury, provide the most appropriate postoperative care, and be able to make recommendations.
Types of nerve damage:
- complete or partial resection of the nerve (cutting),
- compression, crushing, stretching, pinching, thermal and ischemic damage.
Total sensory deficits can range from minor sensory loss to persistent, severe, and debilitating pain dysfunction, but the most common combinations include anesthesia, paresthesia (painless altered sensation), dysesthesia (uncomfortable altered sensation), and neuropathic pain.
Currently, there is no standardized protocol for the dentist to diagnose and treat post-implant nerve injuries.
We will try to fill this gap.
Post-traumatic sensory nerve damage. Terminology.
The Association for the Study of Pain has standardized a nomenclature system that defines the most commonly used neurosensory descriptive terms Classification of Chronic Pain, Second Edition: International Association for the Study of Pain Task Force on Taxonomy, ed.: H Merskey and N. Bogduk. IASP Press IASP Council in Kyoto, November 29-30-2007.
- Paresthesia is a non-painful altered sensation. May be described by patients as a pins and needles, slight burning or tingling sensation. NEW sensations - stretching, pulling sensations.
- Dysesthesia is perverted sensations. Abnormal, sometimes unpleasant sensations experienced by a person with partial damage to sensory nerve fibers when touching the skin. - Unpleasant abnormal sensation, spontaneous or provoked. Note : Dysesthesia is not pain when it hurts or paresthesia. Special cases of dysesthesia are hyperalgesia and allodynia. Dysesthesia should always be unpleasant , and paresthesia should not be unpleasant, although it is recognized that the boundary can create some difficulties when it comes to whether these sensations are pleasant or unpleasant. It should always be stated whether the sensations are spontaneous or provoked.
- Neuropathic pain (IASP) is pain caused by damage or disease of the somatosensory nervous system.
- Neuropathy (IASP) is a dysfunction or pathological change in a nerve: in one nerve - mononeuropathy; in several nerves - mononeuropathic multiplex; if diffuse and bilateral - polyneuropathy. Note : Neuritis is a special case of neuropathy and is currently a term reserved for inflammatory processes affecting the nerves. - sensitive (touch, heat, pain) - motor (movement).
- Allodynia is pain from non-noxious stimuli (pain with light touch/cold/heat). The appearance of pain in response to a stimulus that does not cause pain in healthy people. Thermal allodynia, especially cold allodynia, is a feature of the extraoral dermatome in patients with IANIs. Some patients report decreased taste and heat sensitivity. Perversion of sensitivity is characterized by an increased threshold of sensitivity and increased duration of perception, lack of precise localization of sensations of an unpleasant nature, and a tendency to irradiate. The pain continues when the stimulus is removed.
- Hyperalgesia - increased sensitivity to painful stimuli
- Anesthesia - numbness
- Hyperesthesia and Hypostesthesia are terms that are often used to describe changes in sensitivity that increase or decrease, respectively.
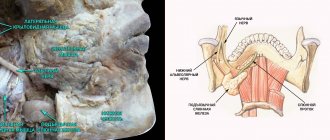
Rice. 5 Anatomy of the II (maxillary) and III (mandibular) branches of the trigeminal nerve. It is important to note that the branches of the superior alveolar nerve retrogradely “merge” into the infraorbital nerve, which explains the symptoms of swelling and pain in the infraorbital region when the superior dental plexus is damaged.
Post-traumatic sensory neuropathy is pain that develops after medical intervention (surgery, treatment, anesthesia), with a minimum duration of 2 months, while other causes of pain are excluded (infection, persistent malignancy, misdiagnosis, etc.), preoperative pain from others must also be excluded reasons.
It is important to add that the neuropathic area does not have to be clearly indicated by the patient, however, about 80% of patients can localize and indicate the neuropathic area.
HERE you can read more about the incidence of “phantom toothache” (atypical odontalgia) after endodontic treatment, which is classified as persistent dentoalveolar pain (PDAP type 2) and occurs in up to 3% of cases.
General overview
The trigeminal nerve is one of the cranial nerves that perform a wide range of functional tasks. Located on both sides of the face, it provides sensitivity to the skin, elements of the dentition, mucous tissues, as well as other areas of the head, and at the same time regulating salivation. Quite often the trigeminal nerve is confused with the facial nerve, which is due to the similarity of their anatomical position. However, in fact, these are different paired elements of the nervous system, each of which implements its own functionality.
Factors influencing neurological response to nerve injury
— Preoperative screening for neuropathic pain is necessary. Preexisting neuropathic dental pain (PDAP type 1), which exists before surgery, can be caused by many different systemic conditions, medications, and other lesions. It is critical that surgeons recognize presurgical neuropathic conditions because neuropathic pain does not respond to surgery and can often lead to worsening pain. In addition, poorly controlled preoperative pain and nerve damage can cause chronic postoperative pain.
— The main indicators for predicting chronic post-surgical pain are psychological factors, including the level of anxiety, neuroticism (a fundamental personality trait in psychology, characterized by anxiety, fear, rapid mood swings, frustration and a feeling of loneliness. It is believed that neurotic people cope worse with stress and are prone to exaggerate the negative side of a particular situation.), catastrophization and introversion. Thus, the doctor has the opportunity not to perform the surgery of choice (implantation) in such patients, but to decide in favor of an alternative treatment plan.
- The concentration of the anesthetic used is up to 2% lidocaine - the accepted standard, because higher concentrations have a greater neurotoxic effect, which may cause permanent neuropathy. Avoid using multiple (repeated) anesthetic blocks in the same area for the same reason.
— Preoperative medical examination should exclude the following diseases : Raynaud's disease, Erythromelalgia (Mitchell's disease), Irritable bowel syndrome (IBS), Migraines, Fibromyalgia.
—Location of surgery is another factor associated with neurological response. Trauma in the distal jaw is more significant (eg, angle and ramus) than in the mental foramen, because the closer the proximal nerve injury is, the greater the risk of damaging trigeminal ganglion cells and initiating retrograde effects of differentiation into the central nervous system. .
Thus, a thorough interview and examination of the patient, detailed pre-implantation planning based on CBCT data, appropriate visualization of the implantation plan and the use of surgical guides, selection of optimal implant sizes with extended safety zones, use of drill limiters and, of course, an experienced team of doctors who will carry out the implantation followed by early postoperative care, all of which will contribute to safer practice and optimized patient outcomes.
Symptoms
It is no secret that timely treatment is highly effective. Therefore, at the first
manifestations, you should consult a doctor. Why do you need to know what symptoms are characteristic of pathology?
The trigeminal nerve is one of the largest nerves located in the skull. It has three branches, the first of which is affected much more often. In this case, the patient feels a sharp and severe pain of a shooting nature. It either intensifies or subsides. Sometimes accompanied by tics and spasms.
Seizures occur in the trigger zone - the nasolabial triangle, temporal and frontal parts of the face. Common activities that can trigger pain include:
- Talking, smiling or other facial movements.
- Sometimes occurs when shaving, brushing teeth and washing.
- A blow to the nose.
- As a result of hypothermia.
The reason may be:
- ARVI, influenza and other diseases.
- Tooth extraction and other dental problems, for example, incorrect installation of fillings, pulpitis, periodontitis.
- Bacterial diseases of the oral cavity.
- Eating spicy, smoked and fatty foods.
- Impact, bruise in the jaw and face, as well as other injuries.
A migraine attack can cause the development of neuralgia, as can endocrine disorders and herpes infection.
The main symptom is severe pain that can last from a few seconds to an hour. At this time, the patient experiences torment that knocks him out of his usual way of life, he completely loses his ability to work.
Characteristic features are:
- Severe pain, the intensity of which increases with any movement, for example, chewing food, talking, opening the mouth.
- The face is skewed to one side.
- The pain is localized in the ear, teeth, lips.
- Involuntary muscle contraction - tic.
- Increased salivation and lacrimation are often observed.
In most cases, the lesion covers the right or left side of the face, but can also be bilateral.
Features of manifestations of iatrogenic damage to the trigeminal nerve
- Painful discomfort, changes in sensations, numbness (anesthesia).
- Functional consequences - Patients who experience pain from touch or cold often have difficulty with daily functions: kissing, communicating, speaking, eating and drinking, etc. https://www.ncbi.nlm.nih.gov/pubmed/22677874
- Psychological consequences - patients develop various anxiety, fear, anger, post-traumatic stress disorder. Psychological disorders can be aggravated in cases where informed consent for implantation, endodontic treatment, orthognathic surgery, etc., which specifically indicates possible nerve damage, has not been signed before medical intervention.
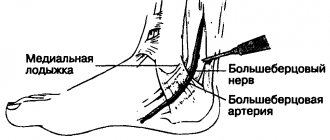
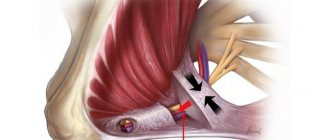
Rice. 6. Schematic representation of the relationship of the branches of the inferior alveolar nerve with the formed implant bed. Pain during drilling is an important diagnostic criterion for the proximity of the nerve.
Clinical algorithm for determining post-traumatic neuropathy
Trigeminal Neuropathy Assessment Questionnaire
Important! Severe pain experienced during treatment may indicate a possible nerve injury.
- History of the initial onset of pain.
- Development of pain.
- Duration of pain.
- History of regular pain SOCRATES (Site, Onset, Character, Radiation, Associated signs, Timing, Exacerbating and relieving factors, Severity) - Localization, Occurrence (frequency of attacks), Character, Irradiation, Associated symptoms, Duration, Exacerbation and relief factors (what intensifies and relieves pain), severity of pain.
- Psychological screening.
- Functional screening (impact on daily life).
Mechanosensory tests (mapping the affected area)
A protocol for examining the dermatome to assess the extra-oral mechanosensory function of the alveolar branch of the trigeminal nerve.
Dermatomes are segments of skin into which the entire surface of the human body is divided in connection with its innervation by various roots of the spinal cord, in this case the trigeminal nerve.
Figure 7. Dermatomes of the branches of the trigeminal nerve
1. Logging the affected area.
Using surgical forceps, move from the normal to the neuropathic (changed) area, warning the patient that there may be increased sensitivity and/or decreased sensitivity. Mark an area on the patient's face with marker marks and take a photo. Assess the % or area of the extra-oral dermatome that is affected by neuropathy.
2. Recording the assessment of subjective sensation.
Press the surgical forceps or probe firmly (but not painfully) against the patient's arm several times at intervals (5 times per minute), explaining that this is a "normal" subjective rating of function on a scale of 10 out of 10. Press with the same pressure on the unaffected side of the face or tongue and repeat the stimulation, explaining that it should be 10 out of 10. Then remove the forceps or probe and explain that the missing stimulation is 0 out of 10. Only then repeat the same actions in the area of neuropathy that you have already confirmed and marked with markers labels, and ask the patient to report the stimulus level out of a possible 10 (if >10 = hyperesthesia and <10 = hypoesthesia). This test should be repeated in different areas of the neuropathy (lip border, lip skin, chin, tongue, etc.)
3. Recording the light touch assessment
To assess light touch thresholds, it is recommended to use a frayed cotton swab, repeating touches at intervals of 5 times per minute. First on the unaffected side and then repeating on the affected side, ask the patient to report the differences. If the patient is experiencing numbness, then the stimulation will have a reduced threshold for detecting light touch, however, if the patient suffers from hyperesthesia and possible allodynia (pain to touch), then this test can be very uncomfortable and irritating.
Dermatomal Involvement Map Interpretation and Neuropathy Assessment —Does the area of neuropathy correspond to the dermatomal area in which surgery was performed? — Dynamics of the area of the involved extraoral and intraoral area when mapping neuropathic areas (criterion reliability is low)
Important! Localized sensory neuropathy is not always present in patients, but there is almost always an area of abnormal sensation, and the patient's maximum pain is associated with the area of sensory deficit, that is, suffering from a combination of pain, numbness and altered sensation. This is an important diagnostic distinction for sensory neuropathy.
Subjective function
- Is neuropathy hyperesthesia or hypoesthesia?
- Thermal allodynia test is the occurrence of pain when exposed to heat or cold. Thermal allodynia, especially cold allodynia, is a feature in patients with trigeminal nerve damage.
- Thermal hyperalgesia test. Increased pain that occurs after a weak stimulus.
- Test "Direction of movement". The patient closes his eyes, the doctor uses a soft brush to determine the patient's ability to detect both the sensation and the direction of movement of the brush.
- Test for sensitivity to temperature stimuli. A cotton swab with cold test spray and a dental mirror handle heated to 43 - 45 ° C are used to determine the patient's ability to feel cold and heat. Alternatively, test tubes can be filled with hot (43 -45 °C) water and cold water.
There are WHO recommendations regarding which parameters of peripheral sensory consequences should be taken into account to predict the results of microsurgical restoration of a damaged sensory nerve. Zuniga JR and Yates DM adapted the recommendations to trigeminal nerve lesions. More details here: Zuniga JR and Yates DM Factors Determining Outcome After Trigeminal Nerve Surgery for Neuropathic Pain. J Oral Maxillofac Surg 2021 Jul;74(7):1323-9.
Today, a guideline for mandatory X-ray monitoring after endodontic treatment and dental implantation surgery has already been adopted in order to indicate the relationship between the root and the root filling, as well as the proximity of the implant bed and/or the implant itself to the canal of the inferior alveolar nerve. Intraoral dental radiography is considered to be sufficient to detect iatrogenicity, although post-traumatic neuropathy is primarily a clinical diagnosis.
Renton T, Yilmaz Z. Managing iatrogenic trigeminal nerve injury: a case series and review of the literature. Int J Oral Maxillofac Surg 2012 May;41(5):629-637.
Treatment of trigeminal neuropathy
Treatment may include drug therapy, surgery, and complex treatment.
Drug therapy is aimed at relieving pain symptoms. Treatment can be long-term (six months or more).
Drugs for the treatment of trigeminal neuritis:
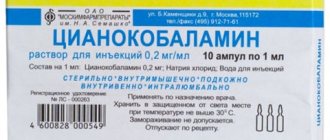
- antiepileptic drugs (carbamazepine, pregabalin, gavapentin), prescribed to reduce pain
- muscle relaxants
- tricyclic antidepressants in small doses (amitriptyline)
- B vitamins (B1, B6, B12)
- antihistamines
- antibacterial (if there are contraindications)
- NSAIDs (non-steroidal anti-inflammatory drugs)
- sedatives
- antiviral drugs (if there are indications for their use).
Physiotherapeutic methods can be used to treat pain:
- antiepileptic drugs (carbamazepine, pregabalin, gavapentin), prescribed to reduce pain
- UFO, UHF
- phonophoresis with anesthetic (lidocaine)
- diathermic currents.
Treatment is carried out on an outpatient basis, sometimes peripheral nerve root blockade is used, but it does not always have a positive effect.
According to indications, radiosurgery and the Gamma Knife technique can be used, but in this technique the treatment result appears after 4 months or more.
One of the last treatment options may be the destruction of the trigeminal nerve - rhizotomy.
What happens after nerve damage?
The interaction between peripheral sensory nerves and the central nervous system is extremely complex. It has been proven that minor trauma such as compression, concussion, contusion or pinching can only lead to numbness, but more serious trauma (chemical burn, partial or complete anatomical break) can lead to dysesthesia and/or neuropathic pain, which causes constant discomfort in patients (especially at night) and affects their quality of life.
- After damage to the fibers of the inferior alveolar nerve, degeneration develops within just a few minutes from the entire site of damage: retrograde towards the central nervous system and Wallerian towards the periphery.
- With acute compression, the axoplasmic flow is immediately disrupted, which will lead to a decrease in membrane excitability. If the compression is not removed = chronic compression, the development of axolysis and Wallerian degeneration begins, which in turn will lead to the development of fibrosis, the formation of neuroma and the progression of neuropathy.
- Even if the nerve fibers are partially interrupted, the possibility of spontaneous regeneration of the nerve remains due to the ingrowth of the axons of the terminal sections of its central segment into the peripheral section, provided that the implant is immediately removed. Between the interrupted nerve fibers, a linear array of Schwann cells is preserved, which significantly increases the nerve growth factor. In addition, the work of the gene encoding receptor mRNA is significantly activated and nerve regeneration is activated. These defense mechanisms and repair reactions can be completed within 2 to 3 weeks. This way, the nerve can reconnect fairly quickly unless there is severe neuropathy or complete rupture.
Although regenerative repair and nerve reconnection will be observed histologically, function is not completely restored. Reconnecting (reconnecting) the nerve does not mean healing, and under certain conditions can cause pain in patients.
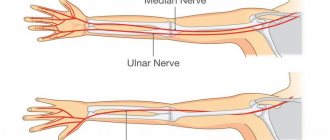
The inferior alveolar nerve is a mixed nerve and is responsible for pain, touch, heat, cold, and pressure, although the mechanism of each sensation is different. An analogy can be drawn with an underground network of pipes in a big city, where gas, electricity, telephone, water and sewage are transported, but each pipe is separate and along its own route. If the nerve networks are damaged, the insulation of the structure is compromised, and when regeneration occurs, adjacent nerve fibers may be accidentally connected to each other. This means that impulses from peripheral nerves can be transmitted to the wrong destination, and from there to the central nervous system. If we take the pipeline analogy, it is as if groundwater and electrical cables severed by an earthquake were cross-connected.
Rice. 8. Inferior alveolar nerve. Mixed sensitivity. Each fiber is responsible for its own type of sensitivity.
This inappropriate connection is called “ ephapsia ” and was proven in laboratory animals back in the 70s of the last century. https://www.ncbi.nlm.nih.gov/pubmed/224343
Thus , after injury, nerve function is never completely restored, even if histological nerve regeneration is completed through active repair.
Consider a case where nerve fibers designed to convey the sensation of cold accidentally become associated with heat fibers, which can compromise the patient's ability to respond to changes in temperature. There are countless numbers of nerve fibers, so injury to any particular nerve can result in connections to any number of other nerves depending on the severity of the injury. A large number of incorrect connections of nerve fibers leads to the formation of neuroma.
Neuromas often generate spontaneous discharge. This electrical impulse causes dysesthesia, and such patients usually complain of numbness, tingling or goosebumps on the skin. https://www.joms.org/article/0278-2391(90)90385-F/pdf
Thus, the healing of a damaged nerve is an incredibly complex process, which is not limited only to the site of injury, but involves the entire system from the periphery to the central nervous system, in contrast to the healing processes of the mucosa or bone. Regressive changes in axons and myelin sheath, as well as nerve regeneration, affect all neurons not only histologically, but also molecularly and electrophysiologically. The emerging ephaps
creates a contact area in which excitation from one cell to another is transmitted through electric current without the participation of mediators.
Rice. 9. Cross-excitation of adjacent fibers of cold and hot sensitivity due to ephaptic transmission of electrical impulses. It is possible for fibers of different diameters to interact (eg, cold and pain sensory fibers), with the signal propagating in both directions, which underlies stimulus-dependent pain symptoms and explains the abnormal perception of non-noxious stimulation in allodynia and hyperpathia.
Prognosis of post-traumatic neuropathy
Important! It is impossible to classify the extent and prognosis of sensory nerve injury based on clinical findings early after injury. Thus, in order to assess the actual outcome of nerve damage, it is necessary to re-interview, examine and test the patient after 2 to 3 weeks of drug treatment.
Prognosis for recovery after injury to the inferior alveolar nerve during implantation:
Full recovery – 50%
Partial recovery – 44%
No signs of recovery – 6%
Diagnostics
The neurologist makes a diagnosis based on the clinical picture, the patient's medical history, the results of a neurological examination and a physical examination. The doctor must rule out diseases that may manifest as facial pain (herpes, headaches). An accurate diagnosis is necessary in order to choose the right tactics for treating neuritis. With neuritis, palpation of the exit points of the trigeminal nerve is accompanied by painful sensations. Diagnosis includes MRI. This is necessary in order to exclude tumors and demyolinating diseases. The diagnosis can be confirmed by the positive effect of low-dose anticonvulsants or tricyclic antidepressants.