Elbow joint
is a unique connection of three bones: humerus, radius and ulna. This is a complex combined joint, which includes three simple joints: humeroulnar, brachioradialis, proximal radioulnar. All of them are united by one common capsule and articular capsule (cavity). Inside the joint capsule, synovial fluid is constantly produced, which serves as a lubricant for the rubbing articular surfaces and nutrition for the anatomical parts. The ends of the bones are covered by a layer of periosteum, which helps protect and renew bone tissue, and also facilitates the supply of nutrients from the synovial fluid. All articular surfaces are covered with articular cartilage. The elbow joint is securely strengthened by ligaments and protected by a good muscular frame. These features allow you to perform four types of movements: extension and flexion, supination (rotation of the forearm in the elbow joint, in which it is possible to turn the hand with the palm up) and pronation (rotation of the forearm in the elbow joint, in which it is possible to turn the hand with the palm down). It is worth noting that the top end of the ulna has an olecranon process, shaped like a hook. The triceps brachii muscle is attached to it. A fracture of this process is a fairly common injury.
Types of damage
The following categories of diseases are characteristic of the elbow joint:
- Traumatic
Bruises. The most common injuries are to the olecranon, periarticular tissues, humeral condyles and ulnar nerve. - Ligament sprains
- Dislocations. There are: isolated dislocation and pronation subluxation of the radial head; dislocations of the forearm posteriorly, anteriorly, inwardly, outwardly; divergent dislocations with rupture of the proximal articulation and divergence of the bones of the forearm to the sides
- Fractures of the bones of the elbow joint according to the nature of the damage can be divided into: intra-articular;
- periarticular;
- closed;
- open;
- no offset;
- with displacement of fragments (displacement of bone fragments most often occurs with fractures of the olecranon)
- Epicondylitis (“tennis elbow”) is an inflammatory and degenerative disease that affects the tendons in the elbow joint due to chronic overload of the forearm muscles.
- Osteoarthritis is a dystrophic-degenerative disease of the cartilage and bone tissue of the joint.
Pinched nerve in the elbow joint. What is Elbow Neuropathy?
Our doctors
Meet our specialists
Work experience 30 years Status Orthopedic traumatologist Qualification Doctor of the highest category
Donskoy E.O. Chief physician of the medical center "MEDICUS". Graduated from the First St. Petersburg State Medical University named after Academician I.P. Pavlov.
Work experience 12 years Status Vascular surgeon Qualification Doctor of the highest category
Nikitina O.A. Graduated from St. Petersburg State Medical University named after academician I.P. Pavlov. She completed an internship at the City Hospital of St. Great Martyr George.
Work experience 5 years Status Therapist Qualification Doctor
Nigai E.Yu. Works as a general practitioner at the Medical Center "Medicus". Conducts initial consultations with patients with various concomitant pathologies.
Work experience over 30 years Status Therapist Qualification Therapist
Danilchenko A.V. Conducts initial consultations with patients with various concomitant pathologies. Works as a therapist at the Medical Center "Medicus"
Work experience 15 years Status Orthopedic traumatologist Qualification Doctor of the highest category
Malofeev V.A. He is fluent in all the necessary methods of diagnosing and treating orthopedic pathologies and successfully restores patients.
Work experience over 30 years Status Nurse Qualification Nurse
Pugacheva O.N. Graduated from Leningrad Medical School. Works as a nurse.
Work experience 10 years Status Physiotherapy nurse Qualification Highest category
Murzakova A.Z. In 1981 she graduated from the Ufa Medical School. In 2012 - “Center for Advanced Training of Specialists No. 1”. Specialty: physiotherapy.
Work experience over 20 years Status Chiropractor Qualification Highest category
Azimov O.A. Specializes in the treatment of diseases of the joints and spine, rehabilitation after injuries and fractures. Works as a chiropractor at the Medical Center MEDICUS.
Work experience 4 years Status Nurse Qualification Junior nurse
Semenyuk E.B. Graduated from St. Petersburg Medical College No. 2. Works as a nurse at the Medical Center MEDICUS.
Work experience 30 years Status Nurse Qualification Highest qualification
Gadzhieva L.A. Graduated from Leningrad Medical School. Works as a senior nurse at the Medical Center MEDICUS.
Symptoms
If the ulnar nerve is incompletely pinched, the following symptoms are observed:
- pain occurs along the nerve
- the hand becomes weaker. It is difficult for a person to write, type and perform other tasks with his fingers.
- tingling occurs in the palm area
- Sensitivity in the little finger and tissues around the ring finger decreases.
- the muscles between the thumb and index finger weaken and decrease in volume.
- sensitivity to cold appears
If the nerve is completely damaged, in this case the sensitivity of the little finger and half of the ring finger disappears completely. Paralysis of the flexor muscles may occur. The hand becomes like a bird's paw.
Treatment methods
Joint reconstruction
1 procedure per course FREE!
Introduction of organic serum with hyaluronic acid into the joint capsule. As a result, cartilage reconstruction occurs Read more…
Neuroprotective therapy
Discount -10%! Only 3 days!
Neuroprotectors are new generation drugs that can restore the conduction of impulses in nerve tissues. Read more…
Plasmacytopheresis
1 procedure for the course is FREE!
Treatment and healing of cartilage with growth factors. Restoration of joint tissue with purified platelet blood. Read more…
Transdermal therapy
Discount -25%! Only 3 days!
The introduction of titanium glycerosolvate into a diseased joint is a unique method of drug delivery without surgery or painful injections. Read more…
Ultraphonophoresis
Discount -25%! Only 3 days!
This is an innovative way to administer medications using ultrasound, which has the unique ability to loosen tissue. Read more…
EHF therapy
Discount -25%! Only 3 days!
This is a promising method of physiotherapy with a great future. In life, waves of this range do not reach the ground, being dispersed in the atmosphere. The device generates these waves itself. Read more…
Infusion therapy
Combinations of drugs for drip administration through a vein. High digestibility and rapid achievement of therapeutic action make infusion therapy Read more…
Blockade
1 procedure for the course is FREE!
A joint or spinal block is a way to quickly help a joint or back. In case of acute pain, the blockade helps to quickly relieve pain and help locally Read more…
Introduction of chondroprotectors
"HONDRO" in Latin means "cartilage" and that says it all. Injection of cartilage cells into damaged segments of the spine Read more...
Autohemotherapy
Treatment using the patient's autologous blood cells. Blood is administered intramuscularly, which provokes the body to intensify the fight against chronic infection, suppuration and trophic ulcers, the immune system is strengthened and effectively resists new infections. Read more…
Laser treatment
Infrared healing with a wavelength of 0.8-0.9 microns affects the internal source of the problem. This relieves inflammation, swelling and pain in the joint. Degenerative processes in the joint fade away as metabolic processes inside the joint accelerate many times. Read more…
Peloid therapy
Nutrition and growth of cartilage cells using peloid dressings. The base comes from Lake Sivash, where mud with a high concentration of Dunaliela Salina microalgae, which is rich in beta-carotene, is extracted.
Diagnosis and treatment
If you consult a doctor in a timely manner, undergo examination and treatment of ulnar neuropathy, you can avoid muscle atrophy and disability. At the beginning, the neurologist interviews and examines the patient. And to determine whether the ulnar nerve is pinched, the following tests are used:
- When pinched, as a rule, the middle and index fingers are bent halfway
- When pressing the hand to the table, a person cannot spread his fingers to the side and raise his little finger.
- If you press on a nerve, the pain intensifies and the hand goes numb.
Results of our patients BEFORE and AFTER treatment
Evgenia Semenovna, 67 years old.
Arthrosis of the knee, stage 3, was sent for joint replacement surgery. With the help of plasma, I coped with arthrosis in 3 sessions. Refused the cane. Avoided surgery. There is no pain, the cartilage and joint capsule have been restored. The duration of treatment is a week.
Pavel Ivanovich, 73 years old
Periarthrosis of the shoulder joint stage 2. I was treated by chiropractors, with leeches and needles - it didn’t help. The plasma caused the regeneration of lost tissue. Full mobility returned, chronic pain of 15 years went away. The treatment period is 10 days.
Natalya Igorevna, 59 years old
Osteochondrosis complicated by hernia formation. Excruciating back pain was relieved in one session. Neurological manifestations - goose bumps in the legs, numbness in the lower leg - disappeared after the second procedure. Course - 2 weeks.
Taisiya Romanovna, 82 years old
Arthrosis of the hip joint stage 3. The operation was refused due to his age and heavy weight. Plasmacytopheresis restored the joint capsule, restoration of articular cartilage and joint lubricating fluid production occurred. Course - 7 days.
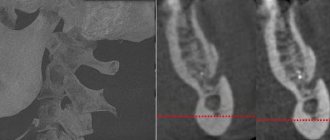
Roman Stepanovich, 73 years old
Headaches, cervical osteochodrosis and vertebral hernias. As a result of treatment, headaches disappeared and pain in the cervical spine decreased. The pictures show restoration of the paravertebral tissues, reduction of the hernia.
Then the doctor sends you for tests: blood and urine tests to determine inflammation in the body, x-ray of the hand, ultrasound, MRI, electromyography, electroneurography, biopsy (if there is a suspicion of a tumor).
Based on the collected data, the doctor prescribes treatment. It should be comprehensive and include: taking medications, vitamin complexes, and antioxidants. Physical therapy, acupuncture, and massage are used to develop muscles.
In severe cases of pinched ulnar nerve, when the integrity of the nerve is compromised and in Guyon's syndrome, surgical intervention is used. It consists of removing the pathology that pinches the nerve. Such operations, as a rule, lead to a complete recovery of the patient.
Experienced doctors at our medical center will give you a professional diagnosis and select the most effective treatment program for ulnar neuropathy. You can make an appointment with a neurologist by calling 986-66-36 or through our website.
Symptoms of pain
The main symptom of elbow disease is pain.
The following signs are typical for the traumatic group of injuries:
- Piercing pain at the time of injury
- Swelling and hematoma in the elbow joint
- Elbow deformity
- Restrictions in arm movements, partial or complete loss of limb function
- Or pathological mobility and the possibility of movements atypical for the elbow
- Numbness or tingling in the forearm, wrist, or hand
- Creaking or clicking noise when moving your elbow
- Any discoloration of the skin in the area of injury
- Palpable protrusion of bone fragments under the surface of the skin
If any of the above symptoms occur, you should immediately seek help from the traumatology department.
Symptoms and causes
Diagnosing elbow pain can be challenging due to the complexity of the joint and its central location in the upper extremity. Diagnosing injuries requires an understanding of the anatomy of the elbow, which includes three joints, two sets of ligaments, four muscle groups, and three major nerves. The medical history should be aimed at identifying the location of symptoms and identifying those activities that cause pain to the patient. It is important to identify specific muscle-ligamentous structures that are at risk of overuse and can be damaged during excessive loads. Mechanical symptoms indicate intra-articular pathology, while neurological symptoms are characteristic of nerve compression.
Types of activities and possible stress injuries to the elbow
| Bowling | tendonitis, radial tunnel syndrome |
| Boxing | Biceps tendinitis |
| Football basketball wrestling | Olecranon bursitis |
| Golf | Radial tunnel syndrome |
| Gymnastics | Biceps and triceps tendinitis |
| Posterior dislocation | Posterior rotational instability |
| Tennis | Pronator syndrome, triceps tendinitis, stress-olecranon fracture, tennis elbow, radial tunnel syndrome, golfer's elbow, ulnar neuritis |
| Rowing | Radial tunnel syndrome |
| Skis | Ulnar nerve neuritis |
| Swimming | Radial tunnel syndrome |
| Throwing (throws) | Pronator syndrome, olecranon impingement syndrome, olecranon stress fracture, collateral ligament sprain, golfer's elbow, ulnar neuritis |
| Weightlifting | Biceps and triceps tendinitis, anterior capsule deformity, radial tunnel syndrome, ulnar neuritis. |
The timing of symptoms can be helpful in identifying possible overuse injuries. The severity of symptoms must be correlated with a possible increase after exercise and the presence of regression at rest. It is important to determine the localization of pain and the presence of pain irradiation. Factors that reduce or increase symptoms should also be identified.
This is especially important for identifying neurological and mechanical symptoms. Weakness or numbness are key symptoms indicating the presence of peripheral nerve compression or cervical radiculopathy. Mechanical symptoms such as clicking during movement, locking during extension may indicate intra-articular pathologies
Causes of pain associated with excessive stress
| Front of elbow | Biceps tendinitis |
| Pronator syndrome | |
| Anterior capsule deformity | |
| Back of the elbow | Triceps tendinitis |
| Olecranon impingement | |
| Stress fracture of the olecranon | |
| Olecranon bursitis | |
| Lateral part of the elbow | Tennis elbow |
| Radial tunnel syndrome | |
| Osteochondritis dissecans | |
| Posterior rotational instability | |
| Medial part of the elbow | Golfer's Elbow |
| Ulnar collateral ligament sprain | |
| Ulnar nerve neuritis |
Treatment Options
Treatment largely depends on the type and nature of the fracture in the elbow joint. For non-displaced fractures (for example, the olecranon), conservative treatment can be achieved by applying a fixing plaster cast for several weeks. If a joint has been displaced, then the issue of surgical intervention is decided. To do this, reposition the fragments (closed or open). With open comparisons, surgical fixation of fragments is required; this operation is called osteosynthesis. Osteosynthesis is the joining of bone fragments using special fixing agents (bone grafts or metal structures). If the fractures of the articular part of the humerus are fragmented, then it is possible to replace the elbow joint with a prosthesis. To restore the function of the elbow joint in case of deforming arthrosis, as well as in congenital and acquired deformities and contractures of other etiologies, osteotomy is currently performed. Osteotomy is a surgical operation that helps eliminate deformation of the elbow joint or improve the function of the musculoskeletal system through an artificial fracture with further fixation to give a functionally advantageous position. After any surgical intervention, the patient is prescribed rehabilitation measures drawn up by the attending physician individually for each person.
Diagnosis of ulnar nerve neuritis
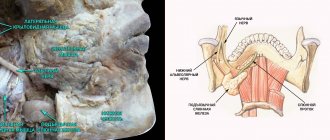
Damage to the ulnar nerve (as a result of surgery, injury, including after drug injection, blows and prolonged compression, bone fractures and joint dislocations) is accompanied by inflammatory changes in it (ulnar nerve neuritis) and manifests itself as a violation of motor and sensory function in the area of its innervation On the hand.
With damage to the spinal nerves C8–Th1–Th2 of the lower trunk and the internal bundle of the brachial plexus, the function of the ulnar nerve suffers equally in combination with damage to the cutaneous internal nerves of the shoulder and forearm and partial dysfunction of the median nerve, its lower leg (weakening of the flexor muscles of the thenar muscles), which creates a clinical picture of Dejerine-Klumpke palsy.
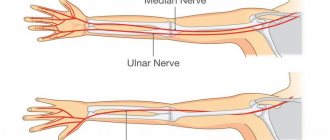
The motor function of the ulnar nerve mainly consists of palmar flexion of the hand, flexion of the fifth, fourth and partly third fingers, adduction of the fingers, abduction of the fingers and adduction of the thumb. In addition, the motor function of the ulnar nerve is to extend the middle and terminal phalanges of the fingers. With regard to the innervation of movements of the II–III fingers, the function of the ulnar nerve is associated with the function of the median nerve, while the ulnar nerve is predominantly related to the function of V and IV, and the median nerve is related to the function of II and III fingers.
Areas of sensory impairment in ulnar nerve neuritis.
Sensitive fibers of the ulnar nerve innervate the skin of the ulnar edge of the hand, fifth and partially fourth, and less often third fingers. Complete damage to the ulnar nerve causes weakening of the palmar flexion of the hand, lack of flexion of the fourth and fifth fingers, and partly the third, the impossibility of bringing and spreading the fingers, especially the fifth and fourth, and the impossibility of adducting the thumb.
Superficial sensitivity in case of ulnar nerve neuritis is usually impaired on the skin of the fifth and ulnar half of the fourth fingers and the corresponding ulnar surface of the hand. In case of ulnar nerve neuritis, the joint-muscular sensation is upset in the little finger. Pain with damage to the ulnar nerve is not uncommon, usually radiating to the little finger. Possible cyanosis (cyanosis), impaired sweating and a decrease in skin temperature in an area approximately coinciding with the area of sensory disorders.
Atrophy of the muscles of the hand with damage to the ulnar nerve appears clearly, depression of the interosseous spaces, especially the first, as well as a sharp flattening of the hypothenar are noticeable. As a result of damage to the ulnar nerve (with ulnar nerve neuritis), the hand takes on the appearance of a “clawed bird’s paw”; when the main phalanges are extended, the middle and terminal phalanges are bent, due to which the fingers take a claw-like position. This is especially pronounced in relation to the V and IV fingers. At the same time, the fingers are slightly separated, especially the IV and mainly V fingers.
Diagnosis of the level of damage to the ulnar nerve during neuritis is made using electroneurography (ENG).
The ulnar nerve gives off its first branches only to the forearm, so damage to it along the entire length to the elbow joint and the upper part of the forearm gives the same clinical picture.
Damage to the ulnar nerve in the region of the middle and lower thirds of the forearm leaves intact the innervation of the deep flexor muscles of the fingers and palm, due to which palmar flexion of the hand and flexion of the terminal phalanges of the fifth and fourth fingers do not suffer. But the degree of “clawedness” of the hand increases.
The use of acupuncture is very effective in the treatment of ulnar neuritis.
To determine the movement disorders that occur when the ulnar nerve is damaged (with ulnar nerve neuritis), when clenching the hand into a fist, there are the following basic tests:
- When the hand is clenched into a fist, fingers V and IV, and partly III, are not bent enough.
- Bending the terminal phalanx of the fifth finger or “scratching” the little finger on the table with the palm tightly fitting to it is not possible.
- It is impossible to adduct the fingers, especially V and IV.
- Thumb test: the patient stretches a strip of paper, grasping it with both hands between the bent index finger and straightened thumb; When the ulnar nerve is affected and, consequently, the adductor pollicis muscle is paralyzed, adduction of the thumb is impossible and the strip of paper is not held by the straightened thumb. In an effort to hold the paper, the patient flexes the terminal phalanx of the thumb using the flexor pollicis muscle, innervated by the median nerve.
Elbow bruise: symptoms of injury
With mechanical damage to soft tissues, the following clinical manifestations are observed41:
- painful sensations at the site of the injury (intensity depends on the degree of damage);
- edema and swelling, which are especially pronounced in the area of loose connective tissue;
- local hemorrhage or bruise (if a joint is damaged, hemorrhage occurs in the joint cavity)
When different parts of the elbow are bruised, nerves can be damaged. This leads to the formation of post-traumatic paresis (loss of muscle strength) and neuritis. This phenomenon may be accompanied by periodic lumbago in the limbs and numbness of the fingers.41
Symptoms of Elbow Tendinitis
In the initial stages of the disease, the clinic is erased or absent. Minor discomfort in the elbow area is usually ignored. Gradually, clinical symptoms increase:
- Local pain initially occurs during flexion, extension, and rotational movements. As the load increases, the intensity increases. Further, the elbow hurts at rest, at night, simple movements are difficult.
- Inflammation leads to swelling of nearby tissues. The exudate prevents the tendons from slipping and puts pressure on the nerve fibers. As a result, movements are limited and neurological symptoms appear.
- When palpating the tendons, the doctor identifies characteristic mobile nodules several millimeters in size. Elastic, elastic in the initial stages, later they acquire a stone density.
- When the inflamed tendon moves, it produces specific sounds that are inaudible in the initial stages. When fibrous nodules and calcifications form, the noise is more accentuated.
- With intense inflammation, the skin over the affected joint is hyperemic; upon examination, it is convenient to compare it with a healthy joint.
The clinical picture is variable and depends on the cause of the disease. With secondary tendonitis against the background of arthritis and arthrosis, patients note morning swelling of the joints and stiffness of movement. Symptoms disappear within a day. Tendinitis against the background of infectious diseases occurs with intoxication syndrome (increased body temperature, weakness, headaches, gastrointestinal disorders, etc.).
Lateral epicondylitis (tendinitis)
With lateral epicondylitis (tennis elbow), the pathological process affects the extensor tendons. This is the most common disease of the elbow joint; it occurs in tennis players (among them 45% of professionals, 20% of amateurs). Patients complain of pain in the outer surface of the elbow, radiating to the forearm or shoulder, gradually increasing weakness of the hand up to difficulty shaking hands and lifting a cup.
Medial epicondylitis
Medial epicondylitis (golfer's elbow) is an inflammation of the wrist flexors and pronator teres, and is 7-10 times less common than lateral epicondylitis. Occurs when performing repetitive rotational movements with the hand, golfers, baseball players, gymnasts, assembly workers, and seamstresses suffer. The painful area is localized on the inside of the elbow joint.
Injuries
If the elbow joint hurts when pressed, you need to check for bruises, dislocations and sprains. Acute sensations may not appear immediately after the injury, but after 1-3 days. You can injure your hand at home, during training, or through excessive physical activity. Often, such a symptom is accompanied by swelling, a feeling of heat at the site of injury, difficulty in flexion and extension, and discomfort in the entire arm. Elbow pain that persists for more than 2 days, or even worsens, is a reason to immediately consult a doctor.
Diagnostics
The doctor makes a diagnosis of tendonitis of the elbow joint based on examination and medical history (trauma, sports, predisposing professional activity). To confirm the diagnosis and assess the severity of changes in the tendon, additional studies are indicated.
Ultrasound is informative in case of injuries; it reveals ruptures of collagen fibers, bursitis, and synovitis.
X-rays provide information about the condition of bones and cartilage. Deformation of the joint structures indicates tendonitis against the background of arthritis and arthrosis.
CT and MRI are the most informative; they allow one to assess the degree of tendon damage and identify islands of fatty degeneration, calcifications, and fibrous nodules.
Laboratory studies of synovial fluid and blood help to establish the root cause of secondary tendinitis (gout, rheumatism, tuberculosis, etc.). The level of leukocytes, uric acid, C-reactive protein, rheumatoid factor, etc. is informative.
Elbow bruise: how to treat?
On the second day after injury, treatment is usually aimed at resolving hemorrhage, restoring lymph flow and blood circulation. For this purpose, physiotherapy (electrophoresis, UHF therapy, etc.) may be prescribed. Exercise therapy, which prevents the formation of fibrous adhesions, may also be helpful.41
One of the symptoms that patients experience when they bruise their elbow joint is pain. For pain in the structures of the musculoskeletal system, it is necessary to use an integrated pharmacological approach. Local treatment of bruises usually includes the use of non-steroidal anti-inflammatory drugs and muscle relaxants.
But in order to determine what to apply to a severe elbow bruise, you need to take into account the fact that there are special requirements for painkillers:
- high effectiveness against pain, inflammation;
- good tolerability, both for short-term and long-term use.
It is also important that the drug chosen has a rapid analgesic effect (especially in the presence of acute post-traumatic pain).42
First aid for a bruised elbow
You can treat a bruised elbow joint for minor injuries at home. But in case of multiple and severe injuries, you must definitely seek help from a traumatologist.41
First aid involves measures aimed at pain relief and immobilization of the injured limb. To rule out the absence of a fracture, it is necessary to undergo an examination. A splint (plaster bandage) can be applied to the injured limb, which eliminates active function, which causes severe pain.41
First aid for elbow bruises also involves the use of cold. A heating pad or ice pack, as well as cold packs for minor injuries, can help reduce pain. Cold also causes vasospasm, which helps reduce hemorrhage and swelling.41
Hemorrhages into the joint cavity must be removed. If blood remains in the cavity of the elbow joint for a long time, the destruction of red blood cells and the release of hemoglobin, which is converted into hemosiderin, may begin. This substance is densely deposited in the synovium and articular cartilage and can cause chronic reactive inflammation.41
30g
recommendations for use
Apply a small amount of gel (3-5 cm) 2-3 times a day, followed by rubbing into inflamed or painful areas of the body. The duration of use of the drug should not exceed 14 days without consulting a doctor.
instructions
50g
recommendations for use
Apply a small amount of gel (3-5 cm) 2-3 times a day, followed by rubbing into inflamed or painful areas of the body. The duration of use of the drug should not exceed 14 days without consulting a doctor.
instructions
100g
recommendations for use
Apply a small amount of gel (3-5 cm) 2-3 times a day, followed by rubbing into inflamed or painful areas of the body. The duration of use of the drug should not exceed 14 days without consulting a doctor.
instructions