Piriformis syndrome (PMS) is a condition characterized by pain in the buttock and/or hip. Some articles define FMS as peripheral neuritis of the sciatic nerve branches caused by abnormal tension of the piriformis muscle. Synonyms such as deep gluteal syndrome, extraspinal radiculopathy of the sciatic nerve and some others are often used. In women, FMS is diagnosed more often than in men (f/m ratio is 6:1).
Clinically Relevant Anatomy
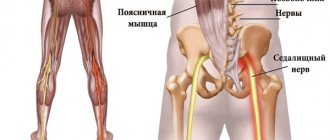
The piriformis muscle arises from the pelvic surface of the sacral segments S2-S4, lateral to the anterior sacral foramina, the sacroiliac joint (superior border of the greater sciatic notch), the anterior sacroiliac ligament, and sometimes the anterior surface of the sacrotuberous ligament. It passes through the greater sciatic notch and attaches to the greater trochanter of the femur. The piriformis muscle is involved in external rotation, abduction and partially hip extension.
Friends, Dmitry Gorkovsky’s seminar “Myofascial release (scientific approach to increasing joint mobility)” will take place very soon. Find out more...
The sciatic nerve usually exits the pelvis below the muscle belly, but many congenital variations can exist. The relationship between the piriformis muscle and the sciatic nerve was classified by Beaton and Anson using a six-category classification system (Beaton and Anson, 1938). Abnormal relationships are designated by the letters B, C, D, E, F. Type “A” refers to the normal relationship between the piriformis muscle and the sciatic nerve.
Variations in the relationship between the sciatic nerve and the piriformis muscle shown in the figure above:
(A) The sciatic nerve exits the greater sciatic foramen along the medial surface of the piriformis muscle.
The sciatic nerve splits as it passes through the piriformis muscle
(B) below or
(C) above;
(D) the entire sciatic nerve passes through the muscle belly;
(E) The sciatic nerve emerges from the greater sciatic foramen along the superior surface of the piriformis muscle. The nerve may also divide proximally, where the nerve or nerve division may pass through the belly of the muscle, through its tendons, or between part of a congenitally bifurcated muscle.
Prevention of sciatica
To reduce the risk of sciatica, it is recommended to monitor your back health. To do this, you need to keep her muscles toned. Daily morning exercises and posture control greatly help prevent inflammation of the sciatic nerve. Swimming also perfectly strengthens the spine, joints and nerve fibers of the musculoskeletal system. Therefore, it is very useful to regularly visit the pool and swim in natural bodies of water during the warm season.
You should control your weight, avoid physical overload and hypothermia, fully treat any injuries and infectious diseases, and also visit doctors for preventive purposes.
At the first symptoms of sciatica, you should consult a doctor, this will help avoid many problems.
If a diagnosis of sciatic nerve sciatica has been made, use modern methods of treating it. Highly professional assistance can be obtained from medical institutions. UVT here is carried out by experienced specialists, and prices for services are much lower than in other Moscow clinics without compromising the quality of treatment.
Epidemiology/Etiology
According to Boyajian-O'Neill LA et al. There are two types of piriformis syndrome - primary and secondary.
Primary SGM
Primary SHM has an anatomical cause, variations of which may include a divided piriformis muscle, a divided sciatic nerve, or an abnormal sciatic nerve pathway. Among patients with BMS, less than 15% of cases are due to primary causes. There are currently no accepted values for the prevalence of the abnormality and little evidence to support whether sciatic nerve abnormality results in FMS or other types of sciatica. These observations suggest that piriformis muscle and sciatic nerve abnormalities may not be as significant in shaping the pathophysiology of FMS as previously thought.
Secondary SGM
Secondary SHM occurs as a result of aggravating factors, including macro- or microtrauma, the effect of prolonged accumulation of ischemia, and the existence of local ischemia.
- FMS most commonly (50% of all cases) occurs due to macrotrauma to the buttocks, leading to soft tissue inflammation, muscle spasm, or a combination of these factors, ultimately resulting in nerve compression.
- Piriformis muscle spasms are most often caused by direct trauma, post-surgical injury, pathology, or excessive stress on the lumbar spine and/or sacroiliac joint.
- FMS can also be caused by shortening of muscles due to altered biomechanics of the lower extremity and lumbosacral region. This can cause compression or irritation of the sciatic nerve. When piriformis dysfunction exists, it can cause a variety of symptoms in the sciatic nerve, including pain in the gluteal region and/or the hamstring, calf, and lateral foot. Microtrauma can occur due to overuse of the piriformis muscle, such as long-distance walking or running or direct compression.
Etiology of FMS
| Injury to the sacroiliac and/or gluteal region | Predisposing anatomical variants |
| Myofascial trigger points (read about MPTT here) | Hypertrophy and spasm of the piriformis muscle |
| Consequences of laminectomy | Abscess, hematoma, myositis |
| Piriformis bursitis | Neoplasms in the area of the infrapiriform foramen |
| Colorectal carcinoma | Neuroma of the sciatic nerve |
| Colon lipoma | Complications of intramuscular injections |
| Thigh nails | Myositis ossificans of the piriformis muscle |
| Klippel-Trenaunay syndrome |
Other causative factors include anatomical variations in the sciatic nerve, anatomical changes or hypertrophy of the piriformis muscle, repetitive trauma, sacroiliac arthritis, and hip replacement. Morton's finger may also predispose to the development of FMS.
Skiers, drivers, tennis players and bikers traveling long distances are most susceptible to the occurrence of SHM.
Tonley JC took a different view regarding the causes of SHM. He writes: “The piriformis muscle can function in an elongated position or under high eccentric loads during functional activities secondary to weak agonist muscles. For example, if the hip is excessively abducted and internally rotated during weight-bearing exercises, much of the eccentric load may be transferred to the piriformis muscle due to weakness of the gluteus maximus and/or gluteus medius. Constant stress on the piriformis muscle due to overextension and eccentric work can result in compression or irritation of the sciatic nerve.”
You can read about the gluteus maximus muscle here. Look here about the gluteus medius muscle.
Characteristics/Clinical picture
- Patients with piriformis syndrome have a variety of symptoms, usually including persistent back pain, buttock pain, numbness, paresthesias, difficulty walking and other functional activities (eg, pain with sitting, squatting, standing, defecation, or pain that occurs during sexual intercourse).
- Patients may also experience pain in the buttock on the same side as the affected piriformis muscle, and in almost all cases, notice tenderness over the sciatic notch. Pain in the buttock may spread down the back of the thigh and lower leg.
- Patients with FMS may also suffer from leg swelling and sexual dysfunction.
- Pain may worsen with physical activity, prolonged sitting or walking, squatting, hip abduction and internal rotation, and any movements that increase tension in the piriformis muscle.
- Depending on the patient, pain may be relieved when the patient lies down, bends the knee, or walks. Some patients experience relief only when walking.
- FMS is not characterized by neurological disorders typical of radicular syndrome, such as decreased deep tendon reflexes and muscle weakness.
- The patient's leg can be shortened and externally rotated in the supine position. This external rotation may be a positive sign regarding damage to the piriformis muscle (the result of its contraction).
Differential diagnosis
FMS can “masquerade” as other common somatic disorders. These include:
- Thrombosis of the iliac vein.
- Bursitis of the greater trochanter of the femur.
- Painful sciatic nerve vascular compression syndrome caused by varicose veins of the gluteal veins.
- Intervertebral disc herniation.
- Postlaminectomy syndrome and/or coccydynia.
- Facet syndrome at the level of L4-5 or L5-S1.
- Unrecognized pelvic fractures.
- Undiagnosed kidney stones.
- Lumbosacral radiculopathy.
- Osteoarthrosis of the lumbosacral spine.
- Sacroiliac joint syndrome.
- Degenerative lesions of intervertebral discs.
- Compression fractures.
- Intra-articular damage to the hip joint: tears of the acetabular labrum, impingement syndrome of the hip joint.
- Lumbar spinal stenosis.
- Tumors, cysts.
- Gynecological reasons.
- Diseases such as appendicitis, pyelitis, hypernephroma, as well as diseases of the uterus, prostate and malignant neoplasms of the pelvic organs.
- Pseudoaneurysm of the inferior gluteal artery after gynecological surgery
- Sacroiliitis.
- Psychogenic disorders: physical fatigue, depression, frustration.
What are the signs and symptoms of an inguinal hernia?
The first sign of an inguinal hernia is a small bulge on one or, less commonly, both sides of the groin—an area just above the crease of the groin between the lower abdomen and thigh. The bulge may increase in size over time and usually disappears when the person lies down.
Other signs and symptoms may include
- discomfort or pain in the groin - especially with straining, lifting, coughing or exercise - that improves with rest
- feelings such as weakness, heaviness, burning, or pain in the groin
- swollen or enlarged scrotum in men or boys
Indirect and direct inguinal hernias can slide into the abdominal cavity and exit into the inguinal canal. The doctor may move them back into the abdomen with gentle massage.
Survey
X-ray studies have limited use for diagnosing BMS. This type of research is used to exclude other pathological conditions; CT and MRI are used for this purpose.
Electromyography (EMG) may also be useful in the differential diagnosis of other possible pathologies, such as a herniated disc. Spinal nerve entrapment will result in changes in the EMG of the muscles closest to the piriformis muscle. However, in patients with FMS, EMG findings will be normal for the muscles closest to the piriformis muscle and abnormal for the muscles distal to it. Electromyographic studies that include active maneuvers such as the FAIR test (flexion, adduction, and internal rotation test) may have greater specificity and sensitivity than other available tests for diagnosing FMS.
Electrophysiological testing and blocks play an important role when the diagnosis is uncertain. Injections of anesthetics, steroids, and botulinum toxin type A into the piriformis muscle can serve both diagnostic and therapeutic purposes.
Rating scales
Roland-Morris questionnaire.
Objective examination
A thorough history and detailed neurological examination are important to make an accurate diagnosis.
Inspection
Patients with FMS may experience atrophy of the gluteal muscles, as well as shortening of the limb on the affected side. In chronic cases, muscle atrophy is observed in other muscles of the affected limb.
Palpation
The patient reports increased sensitivity during palpation of the greater sciatic notch, the sacroiliac joint area, or over the belly of the piriformis muscle. Spasm of the piriformis muscle can be detected with careful deep palpation.
With deep palpation in the gluteal region, soreness or sharp pain may occur, accompanied by spasm and numbness.
Pace's sign
A positive Pace sign is when the patient has pain and weakness with abduction and internal rotation against resistance while sitting. A positive Pace's sign occurs in 46.5% of patients with BMS.
Straight Leg Raise Test
The patient reports pain in the buttock and hamstrings during passive straight leg raises performed by the examiner.
Freyberg's sign
Includes pain and weakness with passive forced internal rotation of the hip in the supine position. The pain is thought to result from passive stretching of the piriformis muscle and pressure on the sciatic nerve at the sacrospinous ligament. The result was positive in 56.2% of patients.
FAIR test
Pain with flexion, adduction and internal rotation of the hip.
Beatty maneuver
This is an active test that involves raising the affected side with a bent leg while the patient lies on the unaffected side. Abduction causes deep pain in the buttock in patients with BMS and pain in the lower back and leg in patients with lumbar intervertebral disc disease.
Hughes test
External rotation of the affected lower extremity following maximum internal rotation may also be painful in patients with FMS.
Hip abduction test
Hip abduction test
The patient lies on his side with the lower leg flexed to provide stability to the body and the upper leg straightened in line with the torso. The therapist stands in front of the patient at foot level and observes (without using his hands) as the patient slowly raises his leg at his request.
Normally, hip abduction should be 45°. This may involve hip flexion (indicating shortening of the tensor fascia lata) and/or external rotation of the leg (indicating shortening of the piriformis muscle), and/or “pulling” of the hip at the beginning of the movement (indicating overactivity of the quadratus femoris and , therefore, indirectly, its shortening).
Trendelenburg test
The Trendelenburg test may also be positive.
Diagnostics
Before carrying out treatment, the doctor must find out the cause of the pain syndrome in the area of the sciatic nerve, therefore an adequate diagnosis should be carried out, since sciatica is a syndrome that can accompany various conditions.
The neurologist first conducts an examination, checks the reflexes on the legs by tapping with a hammer, and determines skin sensitivity, which makes it possible to roughly assess the stage of damage to the nervous system.
To clarify the diagnosis, the simplest method available in any clinic is standard radiography, which will confirm or rule out serious bone changes.
If this diagnosis is not enough, the doctor may prescribe an MRI - magnetic resonance imaging or CT - computed tomography. If a tumor is suspected, it is possible to conduct a radioisotope scan of the spine, this is especially indicated for people taking corticosteroid drugs for a long time, as well as for HIV-infected people.
Treatment
Conservative treatment
Conservative treatment for FMS includes pharmacologic agents (nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and medications for neuropathic pain), physical therapy, lifestyle changes, and psychotherapy.
Injections of local anesthetics, steroids, and botulinum toxin type A into the piriformis muscle can serve for both diagnosis and treatment. The practitioner should be familiar with variations in anatomy and the limitations of techniques based on anatomical landmarks. Recently, the ultrasound-guided injection method has been used. This technique has been shown to have both diagnostic and therapeutic value in the treatment of BMS.
FMS often becomes chronic, so pharmacological treatment is recommended for a short period of time.
Surgical intervention
Surgical interventions should be considered only when nonsurgical treatment has failed and symptoms become intractable and disabling. Classic indications for surgical treatment include abscesses, neoplasms, hematomas, and painful compression of the sciatic nerve vessels caused by gluteal varices.
Some authors have reported that surgical release of the piriformis muscle by cutting the tendon to free the sciatic nerve from compression results in immediate pain relief.
Sometimes the obturator internus muscle should be considered as a possible cause of pain in the area of innervation of the sciatic nerve. However, the diagnosis of obturator internus syndrome can only be made by ruling out other possible causes of gluteal pain, which is similar to how FMS is diagnosed. Surgical release of the obturator internus muscle can lead to both short-term and long-term pain relief in patients with retroacetabular pain syndrome and should be considered if conservative treatment has failed.
Postoperative management of the patient consists of partial weight reduction through the use of crutches for 2 weeks and selection of exercises. The above surgical approach has shown promising short-term results.
Treatment algorithm for retroacetabular pain syndrome:
Physical therapy
Although there are few recently published controlled studies that critically examine the effectiveness of noninvasive treatments, there are a number of treatment options for BMS that are well established in clinical practice.
Noninvasive treatments include physical therapy and lifestyle changes. According to Tonley et al., the most commonly reported physical therapy interventions include soft tissue mobilization, piriformis stretching, cryotherapy (hot packs or cold spray), and manual treatment of the lumbosacral spine.
In addition, Tonley describes an alternative approach to the treatment of BMS. Treatment focused on functional "Therapeutic Hip Exercises" exercises aimed at strengthening the hip extensors, abductors, and external rotators and correcting abnormal movement patterns. Despite the positive results (complete elimination of pain in the lower back, cessation of pain in the buttock and thigh), further research is required, since this protocol was tested in only one patient.
In order not to miss anything interesting, subscribe to our Telegram channel.
To achieve a 60-70% improvement, the patient usually undergoes 2-3 treatments per week for 2-3 months.
- Start with ultrasound treatment: 2.0-2.5 W/cm2 for 10-14 minutes. Apply the ultrasound gel using wide strokes in a longitudinal direction along the piriformis muscle from the connecting tendon to the lateral edge of the greater sciatic foramen. The patient should be in the contralateral lateral decubitus position and in the FAIR position (flexion, adduction, internal rotation).
- Before stretching the piriformis muscle, treat the same area with hot compresses or a cold spray for 10 minutes. Using hot and cold before stretching is very helpful in reducing pain.
- After this, move on to stretching the piriformis muscle, which can be performed in a variety of ways. It is important not to push down, but to direct the pressure along the surface (tangentially) to the ipsilateral shoulder (Fischman et al. (2002), level of evidence A2). When pressing downward, the sciatic nerve is compressed along the tendinous edge of the superior gemellus muscle. Another way to stretch the muscle is the FAIR position. The patient is in the supine position with the hip flexed, adducted and internally rotated. The patient then moves the foot on the affected side across and over the knee of the unaffected leg. The specialist can increase the stretch by using muscle-energetic techniques.
- After stretching the piriformis muscle, you can perform myofascial release of the lumbar muscles, as well as do Mackenzie exercises.
- Because FMS can occur when a tight piriformis muscle is forced to do the work of other large muscles (such as the gluteus maximus or gluteus medius), an alternative approach to treating FMS using a strengthening program for the hip muscles (especially weak gluteal muscles) with relearning of the movement may help. in pain relief.
Your therapist can also give you some tips to avoid worsening your symptoms.
- Avoid sitting for long periods of time; Standing and walking are required every 20 minutes.
- Make frequent stops as you move to stand and stretch.
- Prevent injury to the gluteal region and avoid further aggravating actions.
- Daily stretching is recommended to prevent recurrence of BMS.
Home exercises
The patient can also do some exercises at home.
- Rolling from side to side with bending and straightening of the knees, lying on one side of the body.
- Rotate from side to side while standing with relaxed arms for 1 minute every few hours.
- “Riding a bicycle” while lying on your back.
- Knee curls - up to 6 repetitions every few hours.
- Taking a warm bath.