A.Yu. Lubnin, A.A. Potapov, I.V. Nikitenkova, I.A. Savin, K.A. Popugaev, A.V. Oshorov
FGAU "National Medical Research Center of Neurosurgery named after. acad. N.N. Burdenko" of the Ministry of Health of Russia, Moscow, Russia
For correspondence: Lubnin Andrey Yurievich - Dr. med. Sciences, Professor, Head of the Department of Anesthesiology, Resuscitation and Intensive Care of the Federal State Institution "National Medical Research Center of Neurosurgery named after. acad. N.N. Burdenko" of the Ministry of Health of Russia, Moscow; e-mail
For citation: Lubnin A.Yu., Potapov A.A., Nikitenkova I.V., Savin I.A., Popugaev K.A., Oshorov A.V. Sudden cerebral edema after uncomplicated bilateral cranioplasty. Clinical observation and literature review. Bulletin of Intensive Care named after. A.I. Saltanova. 2020;2:137–145. DOI: 10.21320/1818-474X-2020-2-137-145
Essay
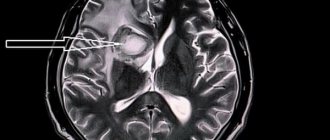
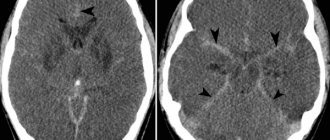
The paper describes a clinical observation of the acute development of cerebral edema after uncomplicated bilateral cranioplasty. The discussion and review of the literature examines the mechanisms of development of cerebral edema that occurs after the closure of extensive bone defects of the skull, especially large and bilateral ones, as well as the possible role of subgaleal drainages.
Key words: cranioplasty, complications, acute cerebral edema
Received: 03.03.2020
Accepted for publication: 02.06.2020
Read article in PDF
Statistics Plumx Russian
Methods for plastic surgery of a bone defect of the skull
A bone defect in the skull is a hole in it that forms after neurosurgical intervention on the organs of the central nervous system or as a result of trauma.
Let's talk in more detail about skull defects in medical practice. After removing a section of bone and creating a hole in the skull, patients experience not only psychological discomfort, but also the so-called “trepanned skull syndrome.” In both cases, the hole must be closed with an implant. And now about everything in more detail.
Literature
- Arac A., Blanchard V., Steinberg GK Assessment of outcome following decompressive craniectomy for malignant middle cerebral artery infarction in patients older than 60 years of age. Neurosurg. Focus. 2009; 26:E3. DOI: 10.3171/2009.3.FOCUS0958
- Bohman LE, Schuster JM Decompressive craniectomy for management of traumatic brain injury: an update. Curr. Neurol. Neurosci. Rep. 2013; 13: 392. DOI: 10.1007/s11910-013-0392-x
- Bor-Seng-Shu E., Figueiredo EG, Amorium RL, et al. Decompressive craniectomy: a meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain surgery. J. Neurosurg. 2012; 117:589–596. DOI: 10.3171/2012.6.JNS101400
- Coutinho JM Cerebral venous thrombosis. J. Thromb. Haemost. 2015: 13(Suppl. 1): S238–S244. DOI: 10.1111/jth.12945
- Merenda A., DeGeorgia M. Craniectomy for acute ischemic stroke: how to apply the data to the bedside. Curr. Opin. Neurol. 2010; 23:53–58. DOI: 10.1097/WCO.0b013e328334bdf4
- Rahme R., Zuccarello M., Kleindorfer D., et al. Decompressive hemicraniectomy for malignant middle cerebral artery territory infarction: is life worth living? J. Neurosurg. 2012; 117:749–754. DOI: 10.3171/2012.6.JNS111140
- Raza E., Shamim MS, Wadiwala MF, et al. Decompressive surgery for malignant cerebral venous sinus thrombosis: a retrospective case series from Pakistan and comparative literature review. J. Stroke Cerebrovasc. Dis. 2014; 23:e13–e23. DOI: 10.1016/ j.jstrokecerebrovasdis.2013.07.045
- Sahuquillo J., Martinez-Ricarte F., Poca MA Decompressive craniectomy in traumatic brain injury after DECRA trial. Where do we stand? Curr. Opin. Crit. Care. 2013; 19: 101–106. DOI: 10.1097/MCC.0b013e3285eba1a
- Wijdicks EF, Sheth KN, Carter BS, et al. AHA Stroke Council. Recommendations for management of cerebral and cerebellar infarction with swelling: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45: 1222–1238. DOI: 10.1161/01.str.0000441965.15164.d6
- Hill CS, Luoma AM, Wilson SR, Kitchen N. Titanium cranioplasty and prediction of complications. Br. J. Neurosurg. 2012; 26:832–837. DOI: 10.3109/02688697.2012.692839
- Klinger DR, Madden C, Beshay J, et al. Autologous and acrylic cranioplasty: a review of 10 years and 258 cases. World Neurosurg. 2014; 82:e525–e530. DOI: 10.1016/j.wneu.2013.08.005
- Schwarz F., Dunisch P., Walter J., et al. Cranioplasty after decompressive craniectomy: is there a rationale for an initial artificial bone-substitute implant? A single-center experience after 631 procedures. J. Neurosurg. 2015; 124:1–6. DOI: 10.3171/2015.4.JNS159
- Durga P., Sahu BP Neurological deterioration during intubation in cervical spine disorders. Indian J. Anaesth. 2014; 58:684–692. DOI: 10.4103/0019–5049.147132
- Harris EA Airway management for the patient with an unstable cervical spine. In: Ruskin KJ, Rosenbaum SH, Rampil IJ (Eds.). Fundamentals of Neuroanesthesia. 2014. Oxford Univ. Press. P. 288–303.
- Amoozegar F., Ronskley PE, Sauve R., Menon BK Hormonal contraceptives and cerebral venous thrombosis risk: a systematic review and meta-analysis. Front. Neurol. 2015; 6, A7: 1–11. DOI: 10.3389/fneur.2015.00007
- Coutinho JM, Majoie CB, Coert BA, Stam J. Decompressive hemicraniectomy in cerebral sinus thrombosis: consecutive case series and review of the literature. Stroke. 2009; 40:2233–2235. DOI: 10.1161/STROKEAHA.108.543421
- Ferro JM, Canhao P. Cerebral venous sinus thrombosis: update on diagnosis and management. Curr. Radiol Rep. 2014; 16: 523. DOI: 10.1007/s11886-014-0523-2
- Fischer C., Goldstein J., Edlow J. Cerebral venous sinus thrombosis in the emergency department: retrospective analysis of 17 cases and review of the literature. J. Emerg. Med. 2010; 38: 140–147. DOI: 10.1016./jemermed.2009.08.061
- Kenmur CL, Jovin T., Jadhav A. Cerebral venous sinus thrombosis in users of a hormonal vaginal ring. Obstet. Gynecol. 2015; 126:830–833. DOI: 10/1097/AOG.0000000000000931
- Siudut J., Swiat M., Undas A. Altered fibrin clot properties in patients with cerebral venous sinus thrombosis: Association with the risk of recurrence. Stroke. 2015; 46:2666–2668. DOI: 10.1161/STROKEAHA.115.009528
- Agner C., Dujovny M., Gaviria M. Neurocognitive assessment before and after cranioplasty. Acta Neurochir. 2002; 144:1033–1040.
- Decaminada N., Pernter P., Imondi A., Tomassini A. CT perfusion evaluation of cerebral hemodynamics before and after cranioplasty. Neuroradiol. J. 2008; 21: 459–471. DOI: 10.1177/19714009080210042
- Erdogan E., Duz B., Kokaoglu M., Izci Y., Nimurkaynak E. The effect of cranioplasty on cerebral hemo-dynamics: evaluation with transcranial Doppler sonography. Neurol. India. 2003; 51:479–481.
- Kemmling A., Duning T., Lemcke L., et al. Case report of MR perfusion imaging in sinking skin flap syndrome: growing evidence for hemodynamic impairment. BMC Neurol. 2010; 10: 80. DOI: 10.1186/1471-2377-10-80
- Jelcic N., Della Puppa A., Mottaran R., et al. Case series evidence for improvement of executive functions after late cranioplasty. Brain Inj. 2013; 27: 1723–1726. DOI: 10.3109/02699052.2013.844857.
- Jeyaraj P. Importance of early cranioplasty in reversing the “Syndrome of the trephine/motor trephine syndrome/sinking skin flap syndrome.” J. Maxillofac. Oral. Surg. 2015; 14:666–673. DOI: 10.1007/s12663-014-0673-1
- Kuo JR, Wang CC, Chio CC, Cheng TJ Neurological improvement after cranioplasty - analysis by transcranial Doppler ultrasonography. J. Clin. Neurosci. 2004; 11:486–489. DOI: 10.1016/j.jocn.2003.06.005
- Song J., Liu M., Mo X., et al. Beneficial impact of early cranioplasty in patients with decompressive craniectomy: evidence from trenscranial Doppler ultrasonography. Acta Neurochir. 2014; 156:193–198. DOI: 10.1007/s00701-013-1908-5
- Winkler PA, Stummer W, Linke R, et al. The influence of cranioplasty on postural blood flow regulation, carabrovascular reserve capacity, and cerebral glucose metabolism. Neurosurg. Focus. 2000; 8: e9. DOI: 10.3171/foc.2000.8.1.1920
- Sakamoto S., Eguchi K., Kiura Y., et al. CT perfusion imaging in the syndrome of the sinking flap before and after cranioplasty. Clin. Neurol. Neurosurg. 2006; 108:583–585. DOI: 10.1016/j.clineuro.2005.03.012
- Annan M., De Toffol B., Hommet C., Mondon K. Sinking skin flap syndrome (or syndrome of the trephined): A review. Br. J. Neurosurg. 2015; 29: 314–318. DOI: 10.3109/02688697.2015.1012047
- Honeybul S. Neurological susceptibility to a skull defect. Surg. Neurol. Int. 2014; 5: 83. DOI: 10.4103/2152–7806.133886
- Honeybul S., Janzen C., Kruger K., Ho KM The incidence of neurological instability to a skull defect. World Neurosurg. 2015; pii: S1878–8750(15)01249–8. DOI: 10.1016/j.2neu.2015.09.081.
- Chan KW, Datta NN Iatrogenic acute subdural hematoma due to drainage catheter. Surg. Neurol. 2000; 54:444–446.
- Karamchandani K., Chouhan RS, Bithal PK, Dash HH Severe bradicardia and hypotension after connecting negative pressure to the subgaleal drain during craniotomy closure. Br. J. Anaesth. 2006; 96:608–610. DOI: 10.1093/bja/ael063
- Mohindra S., Mukherjee KK, Chhabra KK, Khosla VK Subgaleal suction drain leading to fatal sagittal sinus hemorrhage. Br. J. Neurosurg. 2005; 19: 352–354. DOI: 10.1080/02688690500305308
- Prabhakar H., Bithal PK, Chouhan RS, Dash HH Rupture of intracranial aneurysm after partial clipping due to aspiration drainage system—a case report. Middle East J. Anaesthesiol. 2008; 19: 1185–1190.
- Roth J., Galeano E., Milla S., et al. Multiple epidural hematomas and hemodynamic collapse caused by a subgaleal drain and suction-induced intracranial hypotension: case report. Neurosurgery. 2011; 68:E271–E276. DOI: 10.1227/NEU.0b013e3181fe6165
- Toshniwal GR, Bhagat H., Rath GP Bradycardia following negative pressure suction of subgaleal drain during craniotomy closure. Acta Neurochir. 2007; 149:1077–1079. DOI: 10.1007/s00701-007-1246-6
- Van Roost D., Thees C., Brenke C., et al. Pseudohypoxic brain swelling: a newly defined complication after uneventful brain surgery, probably related to suction drainage. Neurosurgery. 2003; 53:1315–1326. DOI: 10.1227/01.neu.0000093498.08913.9e
- Yadav M., Nikhar SA, Kulkarni DK, Gopinath R. Cardiac arrest after connecting negative pressure to the subgaleal drain during craniotomy closure. Case Rep Anesthesiol. 2014; 2014: Article ID 146870. DOI: 10.1155/2014/146870
- Chitale R., Tjoumakaris S., Gonzalez F., et al. Infratentorial and supratentorial strokes after cranioplasty. Neurologist. 2013; 19: 17–21. DOI: 10.1097/NRL.0b013e31827c6bb6
- Honeybul S. Sudden death following cranioplasty: a complication of decompressive craniectomy for head injury. Br. J. Neurosurg. 2011; 25: 343–345. DOI: 10.3109/02688697.2011.568643
- Lee GS, Park SQ, Kim R., Cho SJ Unexpected severe cerebral edema after cranioplasty: Case report and literature review. J. Korean Neurosurg. Soc. 2015; 58: 76–78. DOI: 10.3340/jkns.2015.58.1.76
- Santana-Cabrera L., Perez-Ortiz C., Rodriguez-Escort C., Sanchez-Palacios M. Massive postoperative swelling following cranioplasty. Int. J. Crit. Illn. Inj. 2012; 2: 107–108. DOI: 10.4103/2229–5151.97277
- Zebian B., Critchley G. Sudden death following cranioplasty: a complication of decompressive craniectomy for head injury. Br. J. Neurosurg. 2011; 25: 785–786. DOI: 10.3109/02688697.2011.623801
- Robles A., Cuevas-Solorzano A. Massive brain swelling and death after cranioplasty: A systematic review. World Neurosurg. 2018; 111:98–108. DOI: 10.1016/wneu2017.12.061
- Spetzler RF, Wilson CD, Weinstein P, et al. Normal perfusion pressure breakthrough theory. Clin. Neurosurg. 1978; 25: 651–672.
- Petrozza PH Hyperemic complications following resection of arterio-venous malformation: New througts. J. N. S. Anesthet. 1995; 7:202.
- Dodson BA Normal perfusion pressure breakthrough syndrome: Entity or excuse? J. N. S. Anesthet. 1995; 7:203–207.
- Al-Rodhan NRF Occlusive hyperemia remains the most logical explanation for the hemodynamic complications of resected intracerebral arteriovenous malformations. J. N. S. Anesthet. 1995; 7:208–210.
- Moulakakis KG, Mylonas SN, Styroeras GS, Andrikopoulos V. Hyperperfusion syndrome after carotid revascularization. J.Vasc. Surg. 2009; 49:1060–1068. DOI: 10.1016/j.jvs.2008.11.026
- Medel R., Crowley RW, Dumont AS Hyperperfusion syndrome following endovascular cerebral revascularization. A review. Neurosurg. Forum. 2009; 26:E4. DOI: 10.3171.2009.1.FOCUS08276
- Lieb M., Shah U., Hines GL Cerebral hyperperfusion syndrome after carotid intervention: A review. Cardiol. Rev. 2012; 20: 84–89. DOI: 10.1097/CRD.0b013e318237eef8
- Farooq MU, Goushganian C., Min J., Gorelik PB Pathophysiology and management of reperfusion injury and hyperperfusion syndrome after carotid endarterectomy and carotid artery stenting. Exp. Transl. Stroke Med. 2016; 8: 7. DOI: 10.1186/s13231-016-0021-2
Consequences of skull defects
The bones of the skull not only protect the brain from mechanical damage. The absence of one area can cause a lot of unpleasant symptoms or complications for the patient. It is their presence that serves as a direct indication for surgical plastic surgery.
It could be:
- Headache. It occurs not only at the site of the defect, but also affects other areas. Most often, the symptom intensifies or occurs when there is a change in atmospheric pressure and air temperature. The so-called meteosensitivity appears.
- "Astheno-neurotic syndrome." These include complaints of absent-mindedness, decreased concentration, difficulties in solving intellectual problems, frequent mood swings, decreased ability to withstand stress and tolerance to alcohol.
- Protrusion of the contents of the skull outward. When coughing or sneezing, physical stress or exertion, part of the brain substance can protrude through an opening in the skull, under the skin. This leads to traumatization of internal tissues at the edges of the bone defect.
- Symptomatic epilepsy.
- Mental disorders.
Features of the operation
Surgical intervention should not be started when inflammatory processes are detected in the cranial cavity, in the meninges or brain. Contraindications also include noticeable mental abnormalities of the patient, the presence of a piece of bone tissue or a foreign object in the cranial cavity, and bulging of the brain in the problem area. If visual examination and diagnosis do not reveal any of the listed points, surgery is prescribed.
Skull plastic surgery after trephination and other similar manipulations are called cranioplasty. It is aimed at restoring the integrity of the skull after decompression and stabilization operations, gunshot wounds, falls from a height, and mechanical damage. The choice of intervention technology depends on the timing of the plastic surgery, and it can be primary (1-2 days after injury), primary delayed (up to 2 weeks), early (up to 8 weeks), late (more than 2 months).
There are several rules that must be followed during any type of cranioplasty surgery:
- maximum possible preservation of bone tissue elements;
- use of separated fragments as an autograft;
- strict correspondence between the plate size and the size of the closure area;
- absence of sharp and too thin parts of the skull.
Elimination of a skull defect is a rather complex and responsible operation, the first step of which will be excision of the meningeal scar. All manipulations are performed as carefully as possible to avoid trauma to the brain tissue. For good adhesion of the skull bones and the implant, the edges of the entire problem area are exposed, and the material is necessarily installed “flush” with the skull bones. To prevent such a negative phenomenon as graft displacement, reliable fixation is carried out. Conventional soft tissue suturing is not enough.
Cranioplasty
This is the name of the operation to restore the tightness of the skull. It is designed to restore the brain’s protection from external influences, normalize blood and lymph flow, eliminate the above symptoms, cosmetic defects and relieve psychological discomfort.
The essence of the procedure is to close the hole in the skull with an implant. A competent neurosurgeon will help you understand the great variety of implants offered by medicine today and choose the best one. Fill out an application on the website or call us to get advice from a leading specialist to choose the right implant and discuss the features of the upcoming operation.
We will tell you what types of cranioplasty implants there are and how the operation to install them is performed.
How is rehabilitation after brain surgery?
First, the patient is examined by doctors from the rehabilitation team, then, based on the results of the examinations, a rehabilitation program is collectively formed. Next, a physical therapy instructor, an ergotherapist, a neuropsychologist, a speech therapist begin to work with the patient, and physiotherapy and massage procedures are carried out. Doctors of the rehabilitation team examine the patient during the implementation of the program, assess the dynamics of the patient’s condition and, if necessary, adjust the objectives of rehabilitation measures. At the conclusion of the rehabilitation program, a final examination of the doctors of the rehabilitation team is carried out and recommendations are formulated for the patient.
Occupational therapy
Bobath therapy
What is the PNF technique?
Hirudotherapy
Amplipulse (SMT therapy)
Vacuum therapy
Implants
There is a list of mandatory qualities that they must have:
- sufficient strength;
- biocompatibility;
- ease;
- plastic;
- do not cause infectious complications;
- do not have a carcinogenic effect.
Implants can be made from the patient's own bone (autografts) or artificial (xenografts).
Autografts
This is bone that has been temporarily removed to access the patient's brain tissue. If the bone needs to be preserved to close a skull defect later, it is placed under the skin of the patient's abdomen or anterior outer thigh. If such preservation is not possible, other techniques using the person’s own bone tissue are used. And if it is impossible to replace the defect with autografts, they resort to materials replacing them.
Xenografts
The so-called “artificial bones” are made of metal (aluminum or titanium), using methyl methacrylate or hydroxyapatite.
Each of the mentioned implants has its own advantages and disadvantages. For example, hydroxyapatite can be used for defects up to 30 square centimeters. This material is completely biocompatible. And it is able to turn into its own bone tissue after 18 months with small defects. And the risk of infectious complications for this type of implant is the lowest among similar ones.
Titanium is the least likely to cause local inflammatory reactions. And from it it is possible to recreate lost fragments of the facial skeleton, the base of the skull, the vault and the walls of the orbit. This is done using simulation and neuronavigation in the preoperative period.
The doctor will help you understand the variety of implants, as well as find out what the latest medical developments in the field of implantology are, during an in-person consultation. Fill out an application on our website and we will make an appointment with a leading specialist in the field of neurosurgery.
In each specific case, it is important to take into account not only the direct benefits for a person, but also the aesthetic and psychological aspects. As well as restrictions imposed on the patient in connection with the choice (for example, a metal implant does not allow the patient to subsequently resort to MRI examination).
Indications for trepanation
The reasons for the operation are conditions, diseases in which the functioning of the brain and blood circulation are disrupted due to pathologies that compress the brain structures and blood vessels:
- traumatic brain injuries;
- inflammatory processes;
- increased intracranial pressure;
- blood clots, emboli, aneurysm of cerebral vessels;
- hemorrhages;
- abnormalities of the skull;
- tumors;
- cavities with blood clots and other fluid.
Preparation
During an emergency operation, there is no time for a full examination; they are limited only to cito (emergency) blood tests, which include determining the blood group, Rh factor, determining the level of hemoglobin, red blood cells, leukocytes, and indicators of the coagulation system. From instrumental studies - X-ray of the skull or CT. For a planned operation - a complete laboratory analysis of urine, blood, MRI, consultation with a cardiologist, therapist, ophthalmologist and other specialists.
The day before surgery, the last meal is no later than 6 pm. Avoid fatty, salty, spicy foods and alcohol. Stop taking medications that affect blood clotting and alcohol for 7 days. On the day of manipulation, it is forbidden to drink, eat, or smoke. The hair in the incision area is shaved off. The choice of anesthesia depends on the type of trepanation, often general, less often local, if it is necessary to control the patient’s reactions during manipulations.
The patient's position on the operating table depends on three requirements: anesthetic, local, general. The first requirements are that the patient’s position should not impede the movement of the chest; in case of cardiac or respiratory arrest, the position should not interfere with emergency resuscitation measures. Local requirements are optimal exposure of brain structures, a convenient approach for the neurosurgeon to the patient. General – the position should not provoke a deterioration in the patient’s condition or complications.
When trepanning the frontal lobes to gain access to the cranial fossa, the person's chiasmata are placed on their back. When manipulating the temporal, occipital, parietal zones, position on the side or back of the head with the body turned in the opposite direction from the area of operation.