Herpes zoster, symptoms and treatment in adults
Herpes zoster is an extremely unpleasant and fairly common disease of a viral nature. Symptoms of the disease appear in different parts of the body. Usually this is the face, limbs, genitals, lumbar back. Sometimes rashes form on other areas of the skin, but on the face most often.
This disease also has certain signs of damage to the nervous system. In addition to shingles, the causative agent of the disease - varicella zoster - can lead to the appearance of chickenpox in children, as well as adults who have not previously suffered from this disease.
What it is?
Herpes zoster is a sporadic disease caused by reactivation of the herpes virus type III (Varicella Zoster virus). The disease is characterized by primary damage to the skin and nervous system with severe complications.
When varicella-zoster viruses enter the human body, they quickly spread through the blood, cerebrospinal fluid and nerve sheaths. Settling in the nerve cells of the spinal ganglia, they persist there for life. Hypothermia, insolation, alcohol abuse, physical and mental trauma, hormonal cycles - everything that attacks the immune system provokes an exacerbation of the disease. Having a tropism for cells of the nervous system, varicella-zoster viruses cause diseases that often occur as an infectious disease of the central and peripheral nervous systems.
Lifelong latent carriage of varicella zoster has been established in approximately 20% of residents of our country who had chickenpox in childhood. Asymptomatic carriage of a “dormant” virus can be lifelong. The main refuge for it is the nerve cells of the body. Under the influence of internal and/or external agents, the virus is activated.
Story
Shingles was known in ancient times, but was considered as an independent disease. At the same time, chickenpox was often mistaken for smallpox for a long time: despite the fact that the clinical differences between these two infections were described back in the 60s of the 18th century, reliable differentiation became possible only at the end of the 19th century.
The infectious nature of chickenpox was proven by Steiner in 1875 in experiments on volunteers. Assumptions about the connection between chickenpox and herpes zoster were first made in 1888 by von Bokay, who observed chickenpox in children after contact with patients with herpes zoster. These ideas were confirmed only in the late 1950s, when T. Weller isolated the pathogen from patients with both clinical forms of infection.
However, epidemiological data turned out to be the most convincing: the incidence of chickenpox in areas of herpes zoster was significantly higher than the average among the population (in areas of herpes zoster the secondary risk of infection is high). In 1974, Takahashi and his colleagues obtained a weakened Oka strain of the “wild” virus, and in 1980 a clinical trial of a vaccine against chickenpox was started in the United States.
How can you get infected?
The herpes zoster virus is highly contagious (transmissible), so it easily spreads from person to person through airborne droplets, as well as through contact with the skin of a patient. In this case, the liquid contained in the bubbles formed on the epidermis of those infected with chickenpox or shingles penetrates into the body. For the first time, an infected person becomes ill with chickenpox, after which the virus persists in the body for a long time.
An exacerbation of the disease in the form of herpes zoster can occur due to exposure to a number of provoking factors:
- decreased immunity, severe immunodeficiency states;
- taking cytostatics, chemotherapy, cancer;
- autoimmune diseases, pathological disorders in the blood;
- stress, shock;
- poisoning, intoxication;
- prolonged hypothermia;
- old age (over 65 years).
Chickenpox is a common disease in children, and an adult with a history of this disease can activate the dormant virus by contact with the child. Herpes zoster in children under 10 years of age can occur only in the case of congenital disorders of the functioning of cells of the immune system, as well as in cases of chickenpox in the first months of life.
Clinical symptoms and course of herpes HSV1
Primary infection (herpetic gingivostomatitis) occurs most often in children under 5 years of age, in the form of painful blisters in the area of the tongue, throat, larynx, accompanied by fever and dilation of nearby lymph nodes. Symptoms disappear within 2 weeks. The disease is often not recognized.
Skin symptoms in adults begin in the face, but can also be found on the fingers (for example, in people who bite their nails) and on the trunk. The result is follicular and papular lesions, sometimes painful, and swollen lymph nodes.
Skin symptoms of herpes HSV1
With recurrent herpes, general symptoms such as weakness or flu-like symptoms sometimes appear. Factors that initiate the occurrence of recurrent herpes can be UV rays, overheating or cooling of the body, fever, dehydration, menstruation, stress.
Patients with eczema or atopic dermatitis may experience diffuse herpes lesions due to damage to the epidermal barrier and local immune defenses. Herpes can also cause an exacerbation of pemphigus or the occurrence of erythema multiforme. Complications: keratitis, keratoconjunctivitis, pharyngitis, meningitis.
Is herpes zoster contagious?
If a contact person had chickenpox in childhood and has developed a strong immunity, then the risk of contracting herpes zoster is practically reduced to a minimum. However, in people who have not previously had chickenpox, contact with someone with shingles can lead to the development of chickenpox. This risk especially increases in children and adults over fifty years of age with low immunity.
It should be noted that herpes zoster is contagious during the period of herpetic rashes. During the period of healing and formation of crusts, this disease ceases to be dangerous.
Herpes
The content of the article
Herpes, caused by herpes virus I or II, is one of the most common infectious diseases in humans.
There are two types of viruses:
- type I is most often associated with infection in the facial area;
- type II with localization of genital lesions.
After primary infection, both types of viruses remain latent in the ganglia. Due to a variety of factors that contribute to the development of infection, viruses can travel along nerves and multiply in the skin or mucous membranes, causing symptoms of the disease.
In carriers of active infection without symptoms, HSV viruses can be detected in saliva and vaginal discharge. This can lead to the spread of infections, especially HSV2. Infection occurs through personal contact or contamination with secretions.
Primary HSV1 infection occurs in young children and is often asymptomatic or in the form of stomatitis. It turned out that with high population density and poor housing conditions, 100% of children under five years old have antibodies to HSV1.
Primary HPV2 infection occurs after puberty, most often through sexual contact. Its consequence is always skin symptoms in the genital area. Rarely, HSV1 infection can occur in the genital area, most often due to infection during oral sex.
HSV1 or HSV2 infection in children in the genital area may result from sexual abuse.
Patients with a history of HSV infection have circulating serum antibodies that do not protect against recurrence of infection.
Is it possible to get sick again?
When the varicella zoster virus enters the human body, it causes chickenpox (varicella). However, after recovery, this virus is not eliminated, but remains in the human body in a latent state. This virus lurks asymptomatically in nerve cells in the dorsal roots of the spinal cord.
Activation of the virus occurs when the body is exposed to negative factors that contribute to a decrease in immunity. In this case, the disease recurs, only not in the form of chickenpox, but in the form of herpes zoster. As a rule, re-occurrence of shingles is not observed in the future. In patients with normal health, relapse of herpes zoster is observed in two percent of cases.
In ten percent of people, a relapse of herpes zoster is observed in the presence of the following pathologies:
- HIV infection;
- AIDS;
- oncological diseases;
- diabetes;
- lymphocytic leukemia
In this regard, to reduce the risk of relapse of the disease, as well as to prevent the development of herpes zoster, a vaccine against the Varicella-zoster virus was released in 2006. This vaccine showed good results, reducing the risk of developing the disease by 51%.
Genital herpes in women: modern aspects of etiology, pathogenesis and clinic
Etiology. Pathogenesis There are two main antigenic groups of HSV: types I and II. Moreover, strains belonging to the same antigenic type may differ in immunogenicity, virulence, resistance to various chemical and physical factors, which ultimately determines the characteristics of the clinical manifestations of the disease. HSV-I strains can often be isolated from lesions of the skin of the face and upper extremities; HSV-II strains can be isolated from genital localization of lesions, although a direct connection between antigenic specificity and the localization of clinical manifestations of herpes is not found.
The source of HSV infection is a patient or a virus carrier. The virus is transmitted by airborne droplets, contact, transfusion and organ transplantation. During pregnancy, infection of the fetus can occur through the transplacental and transcervical (ascending) routes.
It has been established that in 40% of cases, primary HSV infection occurs through airborne droplets in early childhood, and the source of infection, as a rule, is family members with active signs of GI.
The main links in the pathogenesis of HI are:
1. Infection of the sensory ganglia of the autonomic nervous system (ANS) and lifelong persistence of HSV in them.
2. Damage to immunocompetent cells, leading to secondary immunodeficiency.
3. HSV tropism for epithelial and nerve cells, causing polymorphism in the clinical manifestations of GI.
The virus begins to multiply at the site of inoculation - the entrance gate of infection (skin, red border of the lips, mucous membranes of the oral cavity, genitals, conjunctiva), where typical blistering rashes appear, and penetrates the bloodstream and lymphatic system. In the early stages of HI, viral particles also penetrate into the nerve endings of the skin or mucous membrane, move centripetally through the axoplasm, reaching the peripheral, then segmental and regional sensory ganglia of the central nervous system (CNS), where they remain in a latent state in nerve cells for life.
Infection of sensory ganglia is one of the important stages in the pathogenesis of HI. In case of facial herpes, these are the sensitive ganglia of the trigeminal nerve; in case of herpes, these are the ganglia of the lumbosacral spine, which serve as a reservoir of the virus for its sexual transmission. The spread of HSV in a centrifugal direction during a relapse determines the anatomical fixation of lesions in relapses of herpes simplex.
A recurrent course of infection is observed in 30-50% of the population infected with HSV. Recurrent herpes (HH) affects representatives of all age groups.
The progressive course of HSV infection consists of the appearance of more severe clinical symptoms with increasing duration of the disease, as well as the involvement of organs and systems in the infectious process.
Exacerbations of GI can be triggered by hypothermia, insolation, physical or mental trauma, alcohol intake, and hormonal cycles.
The frequency and intensity of exacerbations during WG vary widely and depend on the virulence and pathogenicity of the pathogen, as well as the resistance of the human body. The disease most often occurs as a local process, the rashes are usually limited in nature.
Herpes simplex can occur in local and widespread forms; the latter is less common and is characterized by the simultaneous appearance of several lesions in distant areas of the skin and mucous membrane or the involvement of tissues adjacent to the lesion in the pathological process.
The appearance in patients during relapses, along with herpetic rashes, of symptoms of intoxication caused by viremia (general weakness, malaise, low-grade body temperature, enlarged and painful peripheral lymph nodes), indicate dissemination of the infectious process, the inability of the immune system to localize the process.
Recurrent forms of herpes have a negative effect on the patient's immune system. HSV, which develops in immunocompetent blood cells, leads to secondary immunodeficiency, which is clinically manifested in frequent colds, decreased performance, the appearance of low-grade body temperature, lymphadenopathy, and psychoasthenia. Recurrent genital herpes (RGH), disrupting the normal sex life of patients, often causes neuropsychiatric disorders and leads to family troubles.
Viremia in women during pregnancy can cause fetal death and stillbirth: herpes viruses cause up to 30% of spontaneous abortions in early pregnancy and over 50% of late miscarriages; they are second only to the rubella virus in terms of teratogenicity.
To date, evidence has been obtained that HSV is often an etiological factor in inflammatory diseases of the central nervous system (meningoecephalitis, ganglioneuritis), ear, nose and throat, lungs (chronic bronchitis), cardiovascular system (peri- and myocarditis, possibly coronary heart disease), gastrointestinal tract, genitourinary system. Damage to the skin and mucous membranes is the most common clinical manifestation of GI, and HSV lesions of the genitals are one of the most common sexually transmitted diseases.
Genital Herpes Clinic (GG)
According to the existing international classification, primary and recurrent HH are distinguished; the latter, in turn, is divided into typical and atypical clinical forms and asymptomatic viral shedding.
The term “genital herpes” implies the presence of a lesion on the skin and mucous membranes of the external genitalia. With the development of virological research methods, information began to appear about asymptomatic and atypical forms of the disease. The diagnosis of “asymptomatic form of GG” is made based on the results of a virological examination when HSV is isolated from the discharge of the urogenital tract, while there are no symptoms of skin lesions and visible mucous membranes of the genitals.
The diagnosis of “atypical form of GG” is made by gynecologists to designate a chronic inflammatory process of the internal genitalia (colpitis, vulvovaginitis, endocervicitis, etc.) in the presence of a laboratory confirmed herpetic nature of the disease, in contrast to the “typical” picture of the disease, in which the mucous membrane of these organs There are lesions with vesicular-erosive elements. At the same time, herpetic lesions of the urethra, anal area and rectal ampulla fall out of this group, although these organs are anatomically and functionally closely related to the genital area.
Infection of the genitals in adults usually occurs as a result of sexual intercourse. The highest incidence of HS was registered in the age group of 20-29 years. Individuals who begin sexual activity at an early age and have many sexual partners are at increased risk of developing HS.
Clinical manifestations of HH are more pronounced in seronegative individuals than in seropositive individuals, which indicates the influence of the immune response formed to HSV-I in childhood on the severity of clinical manifestations of herpes during infection of the genitals with HSV-II.
In most cases, primary infection of the genitals is asymptomatic, subsequently turning into latent carriage of the herpes virus or into a recurrent form of HH. However, in cases of clinically significant onset, primary HH usually manifests itself after a 1-10-day incubation period and differs from subsequent relapses in its more severe and prolonged course.
The typical clinical picture of primary HS is characterized by the appearance of grouped vesicular elements on the mucous membranes of the genital organs and adjacent areas of the skin, appearing on an erythematous background. After 2-4 days, the vesicles open, forming weeping erosions, less often - ulcers, epithelializing under the crust or without its formation. Subjectively, patients are bothered by itching, burning, and pain in the affected area. Some experience an increase in body temperature up to 38°C, and a painful enlargement of the inguinal lymph nodes. The duration of the acute period in primary HS can reach 3-5 weeks.
RGG is one of the most common infectious diseases of the genitourinary system. The disease is difficult to treat and is characterized by a chronic course and impaired sexual function of the patient, which often leads to the development of neurasthenia. In women, herpetic rashes can appear on the labia majora and minora, vaginal mucosa, cervix, perineum and anal area, and the skin of the buttocks and thighs is often affected. The disease is accompanied by the appearance and development of symptoms of intoxication (low-grade fever, general weakness and malaise), enlargement and tenderness of the inguinal lymph nodes (usually on one side).
RGG is characterized by early opening of vesicles with the formation of erosive surfaces and pronounced subjective symptoms (pain, itching, burning sensation in the lesion). RGG is characterized by a severe course; often relapsing forms of the disease occur in 50-75% of patients.
The typical form of RG of the external genitalia is characterized by pronounced symptoms of the disease, the classic development of the lesion (erythema, formation of vesicles, development of erosive-ulcerative elements, epithelization) and subjective sensations, manifested by repeated blistering rashes. The lesions are usually limited, less common and localized in the same area of the skin or mucous membrane. Frequent exacerbations of RGG are often accompanied by a disturbance in the general condition of patients. Within 12-48 hours, local and general prodromal phenomena may appear: itching, burning sensation, pain in the areas of future rashes, regional lymphadenitis, symptoms of intoxication caused by viremia.
The presence of vesicular or erosive rashes on the skin and mucous membrane of the genitals, severe subjective symptoms (itching, burning) allow doctors to visually diagnose RGG, promptly prescribe treatment and inform the patient about the infectious nature of the disease and the danger of infecting a sexual partner.
It should be noted that under the influence of the therapy, the typical course of RGG can change significantly and become abortive. In this case, the elements in the lesion site bypass individual stages of development. In these cases, the lesion may be represented by a papular element, microerosion, or an edematous spot on an erythematous background. Help in making a diagnosis when treating a patient with abortive RH can be provided by a correctly collected anamnesis, which indicates that the patient has had rashes typical of herpes in the past.
Atypical forms of RGG, which significantly complicate the diagnosis, are due to a number of factors:
1) a change in the development cycle of herpetic elements in the lesion;
2) unusual localization of the lesion and anatomical features of the underlying tissues;
3) the predominance of subjective sensations in the lesion
In atypical forms of RHH, one of the stages of development of the inflammatory process in the lesion (erythema, blistering), or one of the components of inflammation (edema, hemorrhage, necrosis), or subjective symptoms (itching) predominates, which give the corresponding name to the atypical form RHH (erythematous, bullous, hemorrhagic, necrotic, itchy). According to the intensity of clinical manifestations, atypical forms can occur rapidly as manifest (bullous, ulcerative-necrotic) or as subclinical (microcracks). And if in atypical forms of RGG, manifested by the formation of vesicles and erosions, into which blisters and ulcers can be transformed with the addition, for example, of a necrotic component, GG can be suspected, then in clinical forms that are not accompanied by a violation of the skin and mucous membrane or the lesion has an unusual form, the diagnosis is established with great difficulty.
Atypical forms of herpes of the external genitalia are more common in women than in men.
In the edematous form of RGG, the lesion on the vulvar mucosa is represented by hyperemia and diffuse edema.
The “itchy” form of RGG is characterized by periodic local appearance of severe itching and (or) burning in the area of the external genitalia with slight hyperemia of the vulvar mucosa at the site.
Atypical forms of RGG also include HSV infection, manifested by single deep recurrent cracks in the mucous membrane and underlying tissues of the labia minora and majora, accompanied by severe pain.
The subclinical (asymptomatic) form of RGG is manifested by microsymptoms: short-term (less than a day) appearance of one or more microcracks, accompanied by slight itching. Sometimes there are no subjective sensations, which reduces the number of patients visiting medical institutions and complicates diagnosis. The subclinical form is usually detected during a virological examination of sexual partners of patients with any sexually transmitted disease, or during an examination of married couples with impaired fertility.
Clinical diagnosis of abortive course, atypical and subclinical forms of RGG is difficult and can only be made using virological research methods.
In the epidemiological aspect, it is these clinical forms of genital herpes that are the most dangerous for the spread of GI, when, against the background of minimal clinical manifestations of the disease, HSV is released into the environment, and the absence of severe symptoms allows patients to have an active sex life and infect sexual partners.
A feature of GG of the female genital organs is multifocality. The pathological process often involves the lower part of the urethra, the mucous membrane of the anus and rectum. Involvement of these organs in the infectious process may occur secondarily following the onset of herpes of the external genitalia, or may occur as an isolated lesion.
Herpetic infection of the pelvic organs.
Based on the characteristics of clinical manifestations, it is advisable to divide herpetic lesions of the pelvic organs into:
1) herpes of the lower part of the urogenital tract, anal area and rectal ampulla;
2) herpes of the upper genital tract.
Herpes of the anal area and ampulla of the rectum, lower part of the urogenital tract (damage to the mucous membranes of the entrance to the vagina, vagina, vaginal part of the cervix, cervical canal, urethra, bladder) manifests itself in two clinical forms: focal, characterized by the appearance of mucous membranes typical of herpes simplex membranes of vesicular-erosive elements, and diffuse, in which the pathological process proceeds as a nonspecific inflammation.
Herpes of the urethra and bladder. Herpetic urethritis is subjectively manifested by pain and cramping at the beginning of urination, dysuric phenomena. On examination, hyperemia of the external urethral opening and scanty mucous discharge are observed; With urethroscopy in the anterior part of the urethra, it is sometimes possible to detect small superficial erosions and catarrhal inflammation. The leading symptoms of herpetic cystitis are cystalgia, the appearance of pain at the end of urination, and dysuric phenomena.
Herpes of the anal area and rectum. The lesion in the anal area usually represents a recurrent fissure, which is often a reason for diagnostic errors. Such patients with an erroneous diagnosis of “anal fissure” end up with surgeons. The itchy form of herpes anus and herpetic lesions of hemorrhoids are also difficult to diagnose.
Damage to the anal area can occur primarily as an independent disease or secondarily as a result of leakage of vaginal discharge and maceration of the anal mucosa if the patient has herpetic colpitis, accompanied by heavy exudation.
When the sphincter and mucous membrane of the rectal ampulla are damaged (herpetic proctitis), patients are bothered by itching, burning sensation and pain in the affected area, small erosions occur in the form of superficial cracks with a fixed localization, bleeding during defecation. Rectoscopy reveals catarrhal inflammation and sometimes erosion.
Diagnosing herpetic proctitis can be especially difficult. We observed patients with RG of the anal area, in whom the onset of the disease was associated with the periodic appearance of scanty mucous, sometimes sanguineous, discharge from the rectum, which coincided in time with sharp bursting pain in the sigmoid region and flatulence, accompanied by severe itching in the anal area. Subsequently, these patients began to develop bleeding fissures in the anal area. Based on the data of retro- and colonoscopy (in some cases with a biopsy) and the results of a virological examination, these patients were diagnosed with “herpetic proctitis”, “RH of the anal area”.
Herpes of the upper genital tract (damage to the uterus, fallopian tubes). The typical clinical picture of herpetic lesions of the upper genitourinary tract is manifested by symptoms of nonspecific inflammation. Typically, patients complain of vaginal discharge, periodic pain in the pelvis, area of the uterus, and ovaries. These patients have been treated by gynecologists with antibacterial and antifungal drugs for a long time without effect. At the same time, a significant number of women who have no discharge and subjective symptoms do not go to the doctor at all and remain a source of infection for a long time.
Such diagnoses as “HSV endometritis” and “HSV salpingoophoritis” are practically never made by doctors. At the same time, ascending forms of herpetic lesions of the internal genital organs in women are confirmed by the detection of HSV in the endometrium, fallopian tubes and uterosacral ligaments. It is very difficult to establish the real frequency of damage to the internal genital organs, because In 25-40%, and according to some data, up to 60% of women, the disease is asymptomatic. It can be assumed that this pathology occurs much more often than it is diagnosed.
For the subclinical form of herpes of the internal genitalia, the patient typically has no complaints; sometimes there are indications of periodically appearing light mucous discharge from the vagina. During a gynecological examination, symptoms of inflammation are not detected. During a dynamic laboratory study of smears of the discharge canal of the cervix, vagina and urethra, an increased number of leukocytes is periodically detected (up to 200-250 or more in the field of view), indicating the presence of an inflammatory process. During a virological examination of smears, the HSV antigen is determined in leukocytes using the immunofluorescence method.
The asymptomatic form of herpes of the internal genitalia is characterized by the absence in patients of any complaints about the genital area, objective clinical data confirming inflammation. During a laboratory examination of the discharge of the urogenital tract, HSV is isolated, while in smears there are no signs of inflammation (leukocytosis). The asymptomatic form of herpes of the internal genitalia is detected in 20-40% of women suffering from herpes of the buttocks and thighs. This important circumstance must be taken into account when planning pregnancy in women with this form of GC due to the existing likelihood of developing complications of HSV infection during pregnancy.
Complications of genital herpes.
Every fourth patient suffering from RGG develops complicated forms of the disease. Complications can be local and systemic. Local complications of HS include a complex of symptoms consisting of increased trauma, dryness and the formation of painful bleeding cracks on the mucous membranes of the external genitalia, which occur as a result of mechanical irritation. These symptoms appear several years after the onset of the disease and complicate the sex life of patients. The area of the posterior commissure and the mucous membrane of the vaginal opening are most often affected.
Involvement of the nervous system in the infectious process occurs in every third patient suffering from HSV, which is due to the neurotropism of HSV and the fact that it is the ganglia of the ANS that are the depot of HSV in the human body. It should be noted that pain syndrome with RGG occupies a special place. Noteworthy is the frequent lack of objective data during gynecological examination indicating inflammation of the internal genital organs. In this case, patients complain of periodically arising nagging pain in the lower abdomen, in the area of the projection of the ovaries, radiating to the lumbar region and rectum, pain in the perineum. In some cases, the pain syndrome can imitate the clinical picture of an “acute abdomen.” Long-term pain syndrome causes a decrease in sexual potency and libido in patients.
This phenomenon is usually associated with specific herpetic neuralgia of the pelvic nerve plexus present in patients.
The characteristics of the pain syndrome during RGG are determined by the properties of the nerve formations involved in the infectious process. Irritation of parasympathetic fibers causes subjective sensations in patients in the form of a burning sensation, which is a pathognomonic symptom during relapses of HS. With herpes of the thighs and buttocks, there is often an increase in the superficial pain sensitivity of the skin (hyperesthesia), subjectively perceived by the patient as a tingling sensation, a sensation of “crawling goosebumps”. Clinical manifestations of ganglioradiculitis are manifested by nagging pain along the back of the thigh, which is caused by the involvement of the sciatic nerve in the pathological process.
Initial period
Prodromal, characterized by general malaise, neuralgic pain of varying intensity, this lasts on average 2-4 days:
- Headache
- Low-grade body temperature, less often fever up to 39C
- Chills, weakness
- Dyspeptic disorders, gastrointestinal dysfunction
- Pain, itching, burning, tingling in the area of the peripheral nerves in the area where the rash will later appear.
- Most often, during an acute process, regional lymph nodes become painful and enlarged.
- In severe cases of the disease, urinary retention and other disorders of certain systems and organs may occur.
After the temperature decreases, other general intoxication disorders also weaken.
Period of rash
The time when rashes characteristic of shingles appear. The symptoms and nature of the rash depend on the severity of the inflammatory process. At first, the rashes look like pockets of pink spots 2-5 mm in size, between which there are areas of healthy skin.
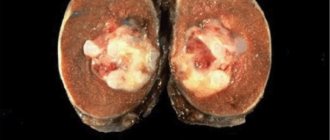
- In the typical form of the disease, the next day, small, closely grouped vesicles and vesicles with transparent serous contents form in their place, which becomes cloudy after 3-4 days.
- In severe gangrenous form of herpes, the contents of the vesicles may be mixed with blood and black in color. Herpetic rashes have a wave-like course, as with chickenpox, that is, fresh rashes with vesicular elements appear at intervals of several days. The bubbles seem to crawl from one place to another, encircling the body, hence the name of this disease.
In mild forms of the inflammatory process, the transformation of skin nodules into pustules does not form and their ulceration does not occur, and the manifestation of herpes is also possible only of a neurological nature - pain without a rash, otherwise it is also called herpetic neuralgia and is often mistaken for manifestations of intercostal neuralgia, osteochondrosis or heart pain. And therefore, inadequate treatment may be prescribed.
Pain is a terrible symptom of herpes zoster
When the disease occurs, the patient always experiences pain, the intensity of which ranges from barely perceptible to excruciating, debilitating pain, which stops for a short period under the influence of drugs. Most often, pain appears in the area of skin rashes corresponding to the affected nerves. The intensity of the pain does not always correspond to the severity of the skin rash.
After the exacerbation stops, 10-20% of patients develop postherpetic neuralgia, in which pain persists for a long time - from several months to several years. Pain is associated with viruses affecting the intervertebral ganglia of the cranial spinal nerves and dorsal roots of the spinal cord. A severe course of the disease is recorded when the spinal cord, brain, and its membranes are damaged. When the autonomic ganglia are damaged, the function of internal organs is disrupted.
How long does it take to treat herpes zoster?
The patient’s recovery time depends on his age and individual characteristics of the body. Shingles is most easily transmitted by young people under the age of 35-40 years. But even in elderly patients, with properly selected treatment, the virus is suppressed within 5 weeks.
However, in some cases the infection leads to various complications:
- bacterial skin infection is the most common complication, usually resulting from poor personal hygiene. After the vesicles dry, the ulcer becomes infected with a bacterial pathogen, which leads to an acute inflammatory reaction and suppuration;
- postherpetic neuralgia is also a common complication, more often diagnosed in old age. In this case, symptoms of shingles may persist for up to six months.
Rarer types of complications include:
- pneumonia;
- nerve paresis;
- glaucoma and other ophthalmological disorders;
- meningoencephalitis and other central nervous system lesions.
To avoid complications, it is recommended to consult a doctor at the first signs of the disease. Since the initial symptoms of shingles (fatigue, fever, body aches) can be confused with the flu or a cold, patients often turn to a general practitioner, who involves a dermatologist in treatment.
Atypical symptoms
Signs of herpes zoster in atypical forms of the course are expressed in the following forms:
| Gangrenous | often manifests itself in severe immunodeficiency and is characterized by an intensified rash, which, encircling the localization, constantly changes movement. This is expressed by the constant appearance of new rashes |
| Abortive | in this form, the blistering rash in the form of vesicles does not appear, but neuralgia remains. |
| Bullous | this form is expressed by the connection of vesicles located nearby into single large papules. |
| Generalized | with serious disorders of the immune system after typical rashes, herpes zoster begins to affect large areas of the skin and mucous membranes. |
| Bubble | the vesicles increase in size, are grouped and form a large area of rashes, seemingly with ragged borders of the lesion. |
Before treating shingles, you need to make sure that it is it. Until herpes zoster gives obvious symptoms, it is impossible to determine the disease, since neuralgic symptoms may indicate other diseases.
Symptoms
The appearance of skin lesions with herpes zoster may be preceded by prodromal symptoms in the form of pain - headache, pain in the ear, throat, shoulder, spine, abdomen, heart area. The pain may appear more than 5 days before the appearance of skin lesions similar to those that appear with chickenpox.
Lesions are most often located unilaterally along the nerves of the face and trunk (the most common location also for chickenpox). After 2-3 days, erosions appear, covered with scabs, often with signs of a secondary bacterial infection.
The appearance of skin lesions may be accompanied by fever and dilation of nearby lymph nodes. In the case of herpes zoster around the face, the lesions also affect the mucous membranes of the mouth and may affect the eyeball.
According to the course and clinical picture, herpes zoster is distinguished:
- hemorrhagic;
- absent-minded
A common form may be a sign of a violation of the body’s immunity, the course of general diseases, such as lymphocytic hyperplasia, cancer, immunosuppression of various etiologies (autoimmune diseases, immunosuppressants, HIV-infected people). Therefore, in patients with severe or disseminated herpes zoster, general examinations should be performed to determine the cause of the exacerbation of the infection.
Treatment of herpes zoster
In adults, herpes zoster may resolve spontaneously and without medical intervention. However, for people with weakened immune systems and elderly patients, treatment for herpes zoster should begin as soon as possible. This allows you to alleviate the severity of the condition and prevent post-herpetic complications.
Among antiviral drugs, adult patients are prescribed tablets for 7–10 days:
- Zovirax – 2 g/day.
- Acyclovir – 0.8 g x 5 r. in a day.
- Famciclovir – 0.5 g x 3 r. in a day.
- Valaciclovir – 1 g x 3 r. per day.
To relieve pain in the initial stages of herpes zoster, the following is prescribed:
- Aspirin.
- Ibuprofen.
- Anileridine.
- Diclofenac.
- Sufentanil.
- Paracetamol.
Antidepressants for the treatment of HSV-3 with prolonged pain syndrome are prescribed as follows:
- Duloxetine.
- Citalopram.
- Mirtazapine.
- Doxepin.
- Maprotiline.
- Clomipramine.
- Escitalopram.
- Venlafaxine.
How to treat herpes zoster to eliminate specific rashes? Experts prescribe medications for external use in addition to antiviral drugs for internal use.
Effective ointments against the Zoster virus are Acyclovir, Bonafton, Alpizarin, Helepin, Interferon, Epervudine. It is useful to treat the body with Allergoferon and Infagel gels, as well as Epigen, Acyclovir, Zovirax creams.
To dry and disinfect wounds left after opening herpetic elements, it is allowed to use Castellani liquid and brilliant green, boric acid and Calamine, Fukortsin and Chlorhexidine lotions. Treatment is varied with zinc preparations (Badigeon, Tsindol) and a strong solution of potassium permanganate.
Folk remedies
All of the following recipes for plant herbs (optional) are prepared as follows: leave one tablespoon of herbs in a glass of boiling water for 20-30 minutes, cool and consume 1/2-1/3 cup 2-3 times a day to relieve mild pain and nervous excitability , as well as for insomnia.
- Valerian root, mint leaves - 3 parts each, watch leaves - 4 parts.
- Mint leaf, watch leaf - 2 parts each, valerian root and hop cones - 1 part each.
- Fennel fruits and chamomile flowers - 1 part each, marshmallow root, licorice root, wheatgrass rhizome - 2 parts each (recommended for children).
- Valerian root – 2 parts, chamomile root – 3 parts, caraway fruit – 5 parts.
- Valerian root, hawthorn flowers, mint leaves, mistletoe herb, motherwort herb - 1 part each.
- Valerian root, motherwort herb, green oat straws - 1 part each.
- Tatar leaves, green oat straw, caraway fruits - 2 parts each, hawthorn flowers, chamomile flowers - 1 part each.
- Mint leaves - 1 part, heather grass, lemon balm leaves - 2 parts each, valerian root - 4 parts.
- Heather leaves, cudweed herb, thyme herb, valerian root - 2 parts each, chicory root - 1 part.
- Motherwort grass, cudweed grass, heather grass - 2 parts each, hop cones, caraway fruits - 1 part each.
The use of medicinal pharmacopoeial herbs is justified in mild forms of the pathogenesis of herpes zoster.
Treatment
For local treatment, the doctor can use desiccant agents, disinfectants, zinc preparations, drugs acting on the DNA of the virus, and prophylactic drugs that protect against sunlight.
Treatment of herpes
Medicines – zoovirax cream up to 5 times a day, iodoxide, neomycin aerosol, vratizoline.
General treatment with acyclovir or famciclovir is indicated for patients with reduced cellular immunity, pregnant women, newborns, and in cases of recurrent infections, especially HSV2, but also HSV1. This treatment is more effective than topical treatment. This may reduce the relapse rate.
Drugs - Acyclovir (Zoovirax), Herpesin, Heviran, are prescribed in doses of 5 x 200 mg orally for 5 days. In case of complications, the drug is administered intravenously. Treatment should be started within the first 2 days of the first skin changes.
For recurrent herpes HSV1 or HSV2, acyclovir can be prophylactically prolonged at a dose of 200-400 mg per day in a chronic manner.
Consequences
A quick and painless recovery from herpetic lichen is due to the general good health of the patient. A young and strong body with normal immunity copes better with the virus. In general, this disease rarely goes away without any complications - in only 30% of cases. Neuralgic pain after a virus infection can last from six months to several years.
The consequences of herpes zoster can be very serious:
- transverse myelitis with transition to motor paralysis;
- heart failure;
- progression of oncological processes;
- Ramsay-Hunt symptom: paralysis of facial muscles, complete or partial hearing loss;
- damage to the oculomotor nerves;
- brain lesions: encephalitis, serous meningitis, meningoencephalitis;
- blindness caused by retinal necrosis.
Improperly treated herpes zoster can develop a relapsing course with subsequent coverage of other nerve trunks. In addition to a neurologist and a skin clinic, you should definitely visit an immunologist for proper correction of immunity.
How dangerous is the disease?
Doctors note a number of severe consequences of herpes zoster, which develop with the unfavorable development of the disease. Among them:
- paralysis, including the facial nerve;
- damage to internal organs;
- severe bacterial infections, purulent inflammations;
- in the ocular form – optic neuritis, decreased visual acuity;
- in the encephalitic form – the development of meningoencephalitis.
Early contact with a doctor allows you to recognize a severe form of the disease in time and take the necessary measures to relieve the consequences.
Vaccination
A live vaccine known as Zostavax has been proposed against the occurrence of the disease.
This vaccine rarely causes side effects but is contraindicated in immunocompromised patients and may not be effective in patients taking antiviral drugs active against Varicella zoster virus. From an economic point of view, it is advisable to use it for patients over 60 years of age.
A Cochrane Library systematic review of eight randomized, placebo-controlled trials involving 52,269 participants found that the Zostavax vaccine in older adults prevented one episode of herpes zoster in every 70 people vaccinated, meaning it was effective in reducing the risk of herpes zoster by almost 50%. Side effects caused by the vaccine were mainly mild to moderate symptoms at the injection site[16].