Multiple sclerosis is an autoimmune disease of the central and peripheral nervous system, which is characterized by the disseminated formation of demyelinating pathological foci with the occurrence of symptoms in accordance with their localization. To this day, there are many questions regarding this pathology. What triggers an autoimmune process? What pathogenetic mechanisms underlie the disease? How to stop this process? Thanks to numerous scientific studies, it was possible to study many aspects of this pathology.
Previously, it was believed that multiple sclerosis mainly affects middle-aged people (30-50 years old). However, world statistics indicate an increase in the number of cases of demyelinating diseases among children. The proportion of multiple sclerosis in the age category from 0 to 16 years is about 1.2–6% of all patients.
The main pathogenetic link in the development of multiple sclerosis in children is a dysfunction of the immune system. As a result of exposure to trigger factors, a cascade of autoimmune reactions is launched. The synthesized T lymphocytes penetrate the blood-brain barrier and selectively destroy the myelin sheath of neurons and their axons. Fibrous plaques form in place of normal nerve tissue. The number of demyelinating foci and their size are determined by the activity of the pathological process.
In multiple sclerosis, not only the nerve cells of the central nervous system, but also the peripheral ones, succumb to autoimmune aggression. This statement was a real discovery in neurology. If just a few years ago disorders of the peripheral nervous system excluded the diagnosis of multiple sclerosis, today such variants of the course of the disease have been scientifically confirmed.
Causes of multiple sclerosis
The main pathogenetic mechanism of this disease is the sensitization of T-lymphocytes by myelin antigens and the activation of autoimmune reactions against their own nerve cells. It has not yet been possible to reliably establish the reasons for this process. There are several predisposing factors that can initiate a cascade of pathological immune response. These include:
- Infectious agents . According to this hypothesis, some viruses (adenoviruses, herpes viruses, mumps, measles) can trigger the synthesis of antimyelin antibodies. The genetic material of viruses is represented by a chain of nucleic acids. Some of its parts coincide with myelin proteins. Thus, antigen-presenting cells (APCs) perceive their own genetic material as foreign. After the exchange of information between APCs and T cells, an autoimmune reaction is launched against the myelin sheath of neurons and oligodendroglia, and inflammatory cytokines (interleukin-2, tumor necrosis factor, interferon gamma) are synthesized in the pathological focus, which lead to destructive processes.
- Heredity . According to statistics, the risk of multiple sclerosis in a child whose family has had a case of this disease is higher than in the general population.
- Environmental factors . The results of some studies confirm the fact that multiple sclerosis is more common in residents of geographical zones remote from the equator. This is explained by the low amount of vitamin D in representatives of the Caucasian race compared to residents of equatorial regions.
- Vaccination of children against hepatitis B and stress factors are not reliable reasons for the activation of autoimmune aggression.
Types of multiple sclerosis
This disease in children is classified according to the clinical course of the disease:
- Remitting-relapsing variant of the course . Episodes of increasing neurological deficit of the disease are followed by periods of partial or complete recovery. During an exacerbation, the neurological deficit increases gradually over several days to several weeks, exacerbation reaches a plateau phase, and then the impaired functions are gradually restored over several weeks or months. In some cases, the exacerbation reaches its maximum within a few minutes or hours. It should be noted that during this course of the disease, in some patients the symptoms that arise do not resolve completely, and the neurological deficit increases over the years.
- Primary progressive variant of the course . After the onset of the disease, gradual progression of the pathology is observed. There may be “bright gaps” in the clinical picture.
- Secondary progressive variant of the course . Against the background of alternating periods of remission and relapse, a secondary increase in the clinical manifestations of the disease is observed.
- Progressive course with periods of exacerbation . The increase in clinical signs of the disease begins with its first manifestations. The progressive course is accompanied by severe periods of exacerbation.
Symptoms of Multiple Sclerosis
The clinical picture of this disease in children is very variable and depends on the location of the focus of demyelination and the course of the disease. Early signs of pathology are nonspecific and are often missed by parents. The main symptoms of multiple sclerosis in children include:
- A constant feeling of general fatigue , which does not depend on physical activity and daily routine. Children become inactive and stop playing with toys and other children.
- Visual impairment . Children often complain of the appearance of a “mesh before the eyes,” double vision, decreased visual acuity, and pain when moving the eyes. Sometimes visual fields are lost and color perception is impaired. Such episodes last more than a day with subsequent restoration of vision. With dystrophic changes in the optic nerve, irreversible damage occurs. When the oculomotor cranial nerves are damaged, strabismus and nystagmus occur.
- Local muscle cramps . They appear suddenly and disappear just as quickly.
- Hearing loss occurs when the auditory nerve or central auditory analyzer in the temporal lobes of the brain is damaged.
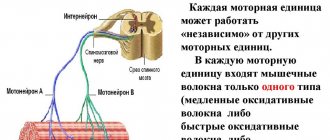
- Movement disorders such as central paralysis (increased muscle tone, decreased strength in the limbs, hyperreflexia, the appearance of pathological reflexes). Abdominal reflexes disappear in multiple sclerosis. Any type of paresis is possible: paraparesis, hemiparesis, monoparesis, tetraparesis. A characteristic feature of motor deficits in multiple sclerosis is variability. Weakness in the limbs waxes and wanes throughout the day.
- Cerebellar symptoms : impaired balance and coordination of movements, intention tremor, scanned speech, etc.
- Disorders of the sensitive area . The most common manifestation of this syndrome is a sensation of “crawling on the skin” or “tingling”. This symptom is called paresthesia. First of all, deep sensitivity suffers (muscular-articular, vibration, kinesthetic). A characteristic sign of sensory impairment in multiple sclerosis is the occurrence of paresthesia in the spinal region when the head is tilted forward.
- Dysfunction of the bladder and lower intestines are the most common reasons why parents of patients consult a doctor. Acute urinary retention or incontinence, neurogenic constipation or fecal incontinence significantly reduce the child's quality of life. These symptoms are associated with a loss of “central” control over the detrusor and sphincters.
- Cognitive and psychological disorders . Children's performance at school worsens, they become inattentive and irritable, and sometimes unemotional and depressed.
For multiple sclerosis, it is impossible to identify separate “classic” symptoms. Each sign of the disease correlates with the location of the degenerative process in the nervous system. Therefore, recognizing the disease in the early stages is very difficult. Especially in children, who are not always able to objectively assess their feelings.
Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease of the central nervous system, most common among young people, which can also occur in children. Pediatric MS, also referred to in the literature as childhood-onset MS, early-onset MS, or juvenile MS, is considered to be MS that develops before the age of 16 years (sometimes before 18 years). In 3-10% of patients with MS, the disease debuted at the age of 16 years or younger, in 1% of patients, MS began at the age of under 10 years. Pediatric R.S. has specific features, the course of the disease differs from that in adult patients [1].
Early diagnosis of MS before the age of 16 years was extremely rare, while currently there is an overdiagnosis of MS, since in childhood there is a wide range of congenital and acquired diseases with similar manifestations, which can often be mistaken for MS. To establish a diagnosis of MS in each child, it is necessary to conduct a differential diagnosis, establish the type of course and stage of the disease in order to optimize treatment methods. Accurate diagnosis could be carried out with the widespread availability of biopsy of pathological lesions to establish a clinical-pathomorphological relationship, but the high risk of biopsy of central nervous system tissue does not allow the widespread use of this method. To make a diagnosis, MRI, cerebrospinal fluid (CSF) studies are used, and less commonly, a complex study of evoked potentials and bioimmunological markers, correlating them with medical history and neurological status [2].
Common features of the pathogenesis of diseases with which differential diagnosis of MS and MS itself should be made determine their similar clinical picture and MRI data, which in turn complicates the diagnosis. In one of the latest publications devoted to the diagnosis of pediatric MS, the authors [3] analyzed in detail the clinical picture, MRI data, and response to treatment of 14 patients with mitochondrial leukoencephalopathy (ML). This rare pathology has a clinical picture that can mimic that of MS.
According to the results of numerous studies, there is a connection between mitochondrial diseases and inflammation in the central nervous system. Some primary mitochondrial diseases, such as ML, have MRI evidence of inflammation. There is modern data indicating the role of mitochondrial dysfunction in the pathogenesis of acquired demyelinating diseases, including R.S. Diagnosis M.L. in the study cohort was determined based on clinical presentation, histopathology, respiratory chain enzyme analysis, and exome sequencing.
We examined 14 patients aged 2 to 7 years, the ratio of boys to girls was 1:1. Genetic data obtained included changes in NDUFA1, NDUFV1, NDUFS2, LYRM, MPV17, BOLA3, IBA57
. Clinical features that mimicked acquired demyelinating diseases included acute onset of focal neurological symptoms associated with encephalopathy (71%), a history of pre-onset febrile illnesses (50%), partial or complete response to glucocorticosteroid (GCS) therapy, and recurrent neurological symptoms (71%) and subsequent stabilization of the condition, rather than a progressive course (85%). According to MRI, confluent foci were observed in the white matter of the brain (100%), decreased diffusion (78.5%), accumulation of contrast agent in pathological foci, involvement of the spinal cord (61.5%), lactate peak according to MR spectroscopy and cysts in the white matter of the brain (92.8%).
Some diseases that accompany MS also share the same pathogenesis of autoimmune and inflammatory processes, which may explain their comorbidity. To date, the world literature has not described many cases of concomitant diseases in children with MS. One of them is a clinical case of a teenage boy [4]. The child had multifocal neurological symptoms, including optic neuritis, as well as hypopituitarism and diabetes insipidus associated with lymphocytic hypophysitis (PH). MRI findings were consistent with the diagnosis of MS according to McDonald criteria (2010). Diagnosis R.S. was also confirmed by CSF analysis and exclusion of alternative diagnoses. The association between PH and MS has been described for the first time. PH is a rare inflammatory disease of the pituitary gland and infundibulum, most often observed in autoimmune diseases with various clinical and endocrine manifestations. On the MRI picture, PH looks like the absence of a light spot of the neurohypophysis with an enlarged cystic pituitary gland, thinning of the pituitary stalk, as well as positive dynamics during therapy with glucocorticosteroids (GCS). PH and MS have a common pathogenesis of an autoimmune process, which perhaps explains their comorbidity. Endocrine disorders such as diabetes insipidus, together with the characteristic clinical manifestations of exacerbation of MS, should encourage further research into possible concomitant inflammatory diseases involving the hypothalamic-pituitary axis [4].
We present two of our own observations of pediatric MS and cerebral palsy (CP).
Observation 1
Girl E
., 14 years old, was admitted with complaints of increased fatigue, weakness in the legs, clumsiness in the arms, periodic tremors, a sensation of “pins and needles” in the area of the fifth finger on the right hand, tremors in the legs, more pronounced on the right, periodic dizziness, inability to move without assistance help, rare urination, constipation. I was bothered by daily headaches of a pulsating nature in the temporal region, occurring mainly in the afternoon, and nagging pain in the coccyx area, radiating to the lumbar region.
History of illness: disabled child due to cerebral palsy. At the age of 3 years, the first episode of loss of consciousness occurred without the development of seizures. She was diagnosed with epilepsy and took Depakine for 2 months. An electroencephalogram (EEG) was performed: no signs of epileptic activity were recorded. EEG video monitoring: minimally expressed epileptiform activity in the central-parietal regions of the brain. The diagnosis of epilepsy was excluded. In April-May 2014, periodic headaches of a pulsating nature in the temporal region and an episode of syncope reappeared. In September 2015, there was a repeated episode of loss of consciousness without the development of seizures.
According to the mother, in November 2015, acutely after sleep, there was a feeling of numbness in the lower extremities, weakness in the legs, she could not sit up in bed or stand on her own, then frequent urination and urinary incontinence, constipation, general weakness developed, and a constant headache developed. dysarthria, emotional lability in the form of irritability, tearfulness. She was urgently hospitalized in the pediatric department at her place of residence. According to MRI of the lumbar spine: signs of right-sided scoliosis, structural changes in the spinal cord. Partial atrophy of the optic nerves was revealed. In the neurological status: mild dysarthria, tetraparesis - mild upper paraparesis to moderate in the distal parts, severe lower paraparesis. A course of symptomatic therapy was carried out. Upon discharge, the neurological status showed increased muscle strength in the legs, a decrease in the severity of sensory disorders, she began to move with bilateral support at a distance of up to 5 m, pain appeared in the coccyx radiating to the lumbar region. X-ray of the sacrum - no pathology was detected.
She was sent to the Republican Children's Clinical Hospital of Ufa, where the patient underwent an MRI of the brain with intravenous contrast: signs of demyelinating brain disease were revealed. MRI of the thoracic spine with intravenous contrast revealed focal pathology of the spinal cord. MRI of the lumbar region revealed no pathology. Electroneuromyography (ENMG) of the lower extremities: conduction disturbances of the suprasegmental type with signs of axonopathy. With EEG: moderate diffuse changes in biopotentials with rare theta waves in the central-parietal areas. During hospitalization, a clinical blood test revealed: leukocytosis 18 thousand. CSF: slightly yellow, slightly cloudy, protein 0.25 g/l, Pandi++ reaction, cytosis 36 (segmented 22, lymphocytes 14). A course of GCS therapy was carried out (dexamethasone 8 mg according to the regimen), then she received prednisolone per os
. During treatment, sensory disturbances and urinary incontinence regressed, muscle strength in the limbs increased, she began to move with bilateral support for a distance of up to 50 m, and pain in the coccyx area increased. There was clumsiness in the hands, tremors and paresthesia in the fifth finger of the right hand. She was sent for hospitalization to the Tyumen Regional MS Center to clarify the diagnosis.
Life history: born in Bashkiria, the first child of twins. The child from the first pregnancy, which was threatened with termination, was born at 32-33 weeks, the second child died at 24 days. Prematurity of the 2nd degree, body weight at birth 1400 g, asphyxia of the 2nd degree, 3-4 points on the Apgar scale. After birth, she was in the intensive care unit, on artificial ventilation for 14 days. She grew and developed with a lag in static-motor development. She started walking at 3.5 years old with bilateral support. She attended a specialized kindergarten for children with disabilities. I was worried about stiffness in my legs, more so in my left. He is registered with a neurologist and an orthopedist with a diagnosis of cerebral palsy and Little's spastic diplegia of moderate severity. She regularly received courses of rehabilitation treatment in sanatoriums and rehabilitation centers in Moscow, Evpatoria, and Anapa. In 2005, a course of autoimmune serum for atopic dermatitis. History: frequent colds, regularly received courses of antibacterial therapy. In 2012, the course of acute respiratory disease was complicated by the development of reactive gonarthritis on the left. He is registered with an ophthalmologist for hyperopia; in 2011, partial atrophy of the optic nerves was revealed. In 2013, she suffered from chickenpox.
From 7 to 14 years old she attended a comprehensive school with normal academic performance. From the 3rd grade I studied at a music school. Against the background of rehabilitation measures, an improvement in gait was noted, the distance increased to 500 m with unilateral support, and she walked around the apartment without support. Since September 2015 - distance learning. From the age of 12 - menstruation, regular. On the first day of menstruation - headache, pain in the lower abdomen.
Ultrasound of the thyroid gland: small focal formation of the right lobe. She consulted with an endocrinologist and was diagnosed with iodine deficiency goiter and euthyroidism. Ultrasound of the abdominal organs: delayed emptying of the gallbladder due to spasm of the sphincter apparatus. Ultrasound of the kidneys and bladder: no pathology was detected.
He denies hepatitis and tuberculosis. Allergological history: allergic reaction to Actovegin. She was operated on for an umbilical hernia in 2001; there were no blood transfusions. Heredity is not burdened.
Somatic status: general condition is satisfactory. Increased nutrition. Pink and white stretch marks on the skin of the chest, abdomen, and buttock area. Peripheral edema in the feet and ankle joints. Constipation. Urination is rare, free, painless.
Neurological status: general cerebral symptoms in the form of periodic headaches, dizziness. There are no meningeal symptoms. Cranial nerves (CN): the sense of smell is not impaired. Palpebral fissures, D=S. There is no anisocoria. Pupillary reactions are lively and symmetrical. Failure to bring the left eyeball outward. There is no strabismus, diplopia, or nystagmus. There is no facial pain. Palpation of the trigeminal points is painless. There are no sensory disturbances on the face or tongue. Corneal reflexes are alive, D=S. There is no facial asymmetry. There is no hearing impairment. Mild dysarthria. There is no dysphonia or dysphagia. The pharyngeal and palatal reflexes are lively and symmetrical. There are no pathological oral reflexes. Tongue in the midline. Tetraparesis: mild upper paraparesis with a decrease in muscle strength on the right to 4.0 points, on the left to 4.5 points; pronounced lower paraparesis with a decrease in muscle strength proximally to 2.5 points, distally to 1.5 points. Muscle tone is changed in a pyramidal pattern in the right arm and legs. Moderately severe spasticity in the lower extremities, mainly in the abductor muscles. Equinovalgus foot deformity. Deep reflexes from the upper limbs are alive, D
>
S
; from the lower extremities - high, clonus of the patellas, feet. The abdominal reflexes on the left are lively, but on the right they are quickly depleted. Spontaneous Babinsky reflex, Poussep, Chedok, Bekhterev, Zhukovsky, Rossolimo reflexes are evoked on both sides. Performs the finger-nose test satisfactorily. In the Romberg sample it is unstable. There are no disturbances in pain sensitivity on the trunk and limbs. Slight decrease in deep sensitivity in the toes. There are no violations of praxis or gnosis. There are no aphasic disorders.
MRI of the brain with intravenous contrast: a picture of multifocal demyelinating disease of the central nervous system with signs of activity of the pathological process (presence of contrasting foci) (Fig. 1, 2).
Rice. 1. MRI of the brain. Axial and sagittal sections. T2-WI and FLAIR images show demyelination foci typical for MS.
Rice. 2. MRI of the brain with intravenous contrast. Axial slices. Foci accumulating paramagnetic contrast in the left hemisphere of the brain. In comparison with the previous MRI, positive dynamics are noted in the form of a reduction in the size of some lesions, the absence of new lesions, and a reduction in the number and size of contrasting lesions.
MRI of the cervical spine with intravenous contrast: MRI signs of multifocal demyelinating disease of the central nervous system with the presence of foci of demyelination in the cervical spinal cord without signs of activity of the pathological process in these foci (Fig. 3).
Rice. 3. MRI of the cervical spinal cord. Sagittal and axial sections. T2-weighted images show foci of demyelination typical for MS (in the spinal cord and brain stem).
Optical CT of both eyes: OU - the thickness of the nerve fiber layer is below the parameters characteristic of adults, the thickness of ganglion cells is reduced. Visual evoked potentials: conduction along the optic nerves is preserved. Computer perimetry: OD - multiple areas of severe depression and defects from 0 to 30° in all sectors of the visual fields (VF), mainly in the lower sector. OS - multiple areas of depression from 10 to 30°, mainly in the outer and lower sectors of the PZ.
Neuro-ophthalmologist: corrected vision 1.0/1.0. Fundus of the eye: the discs are pale pink, the neuro-ophthalmic rim is preserved, the expansion of the disc excavation is 0.3, the vascular bundle is slightly displaced towards the nose, the arteries tend to narrow 2:1, the course of the vessels is correct, the macular reflex is partially preserved. Conclusion: partial descending stationary atrophy of the optic nerve cannot be excluded.
EEG: bioelectrical activity of the brain is disorganized, dysrhythmic. Epileptologist: reflex syncope. There is no evidence for epilepsy. There is no need to prescribe antiepileptic drugs.
LE cells were not detected; anticardiolipin antibodies were not detected; antinuclear antibodies—screening (ANA): 0.605 (normal 0.602); antibodies to ds DNA: negative; enzyme immunoassay (ELISA) of blood for ICD: IgM, IgG negative; Epstein-Barr virus capsid protein: IgM negative, IgG positive; Blood test for HIV: negative; antibodies to aquaporin 4: less than 1:10. CSF: colorless, transparent, no cytosis, protein content is normal, culture - no microflora detected. Isoelectric focusing of oligoclonal IgG in the CSF: the pathological type of IgG synthesis was determined - oligoclonal IgG in the CSF and polyclonal IgG in the blood serum. Taking into account the medical history, MRI data of the brain, and the presence of oligoclonal IgG in the CSF, MS was diagnosed based on the MacDonald criteria (2010).
Treatment was carried out: pulse therapy with GCS (5.0 g of solumedrol per course), intravenous immunoglobulin 0.4 mg/kg, intravenous infusions of thioctacid, cytoflavin; Ceraxon, gliatilin, emoxypine, glycine, phenibut, grandaxin, omeprazole. High-dose therapy with interferon-β-1a 44 mcg (Rebif) subcutaneously 3 times a week was prescribed for a long time.
The condition at discharge is satisfactory, there is a significant positive change in the neurological status - the severity of pyramidal symptoms in the extremities has decreased, stands on toes, moves without support for a distance of up to 5 m. Muscle strength in the upper extremities proximally 5 points, distally 4.5-5.0 points ; in the lower extremities proximally 3.5 points, distally 1.5 points.
Observation 2
Girl D
., 18 years old, was admitted with complaints of visual impairment, speech impairment, inability to move independently, stand up, sit, imperative urge to urinate, difficulty urinating, constipation, periodic headaches.
From the anamnesis it is known that she was born at 32 weeks. The water-free period is during the day. At birth - height 54 cm, body weight 1600 g. Started speaking at 1.5 years. Delayed motor development - did not crawl until age 3, did not sit up, did not walk. At the age of 3 years, disability was determined with a diagnosis of cerebral palsy with tetraparesis, more pronounced in the lower extremities. CT scan of the brain: hydrocephalus. She received treatment courses at a rehabilitation center every year. As a result of symptomatic therapy, from the age of 3 she began to hold objects with her hands, crawl, and walk with bilateral support. At the age of 5 she moved independently using a walker.
In 1999, surgery was performed on both lower extremities to correct spasticity. At the age of 10, she took care of herself independently, moved within the apartment with one-sided support, and performed therapeutic exercises daily. From 6 years old - home schooling according to the general program. I finished 11th grade and took distance learning at the university.
In the fall of 2015, pain appeared in the lumbar spine, she began to spend more time in bed, increased fatigue, and began to move around with outside support. At the end of 2016, she stopped moving independently. In 2021, I couldn’t cope with the university study program and stopped studying. Since 2017, there has been a gradual deterioration in vision, memory, the appearance of an imperative urge to urinate, difficulty urinating, and episodes of urinary incontinence. In March 2021, trembling of the head and limbs appeared, spasticity in the legs increased in the morning, and she began to move around in a wheelchair within the apartment. At the end of July 2021, she noted a sharp deterioration in her condition in the form of increasing weakness in her arms, difficulty in self-care (eating), speech and swallowing problems. MRI of the brain: signs of multifocal demyelinating brain disease. An examination at the R.S. Center is recommended.
Somatic status without features.
Neurological status: involuntary laughter, euphoria, emotional lability. There are no cerebral or meningeal symptoms. CMN: sense of smell is not impaired; palpebral fissures are symmetrical; no anisocoria; pupillary reactions are lively, symmetrical; convergence is weakened on both sides with a predominance on the right; divergent strabismus on both sides; large-scale spontaneous horizontal nystagmus in the extreme leads. There is no facial pain. Palpation of the trigeminal points is painless. There are no sensory disturbances on the face or tongue. Corneal reflexes are lively and symmetrical. There is no facial asymmetry. There is no hearing impairment. Moderate dysarthria, dysphonia, mild dysphagia. The pharyngeal and palatal reflexes are reduced. There are no pathological oral reflexes. Tongue in the midline. Spastic tetraparesis: mild upper paraparesis with a predominance in the distal parts, lower paraplegia. Muscle tone is increased in a pyramidal pattern in the limbs. Pronounced spastic tone in the lower extremities. The position of the legs is forced with slight bending at the knee and hip joints. Deep reflexes from the upper extremities are lively and symmetrical; from the lower extremities, the knees are high, the Achilles are torpid, clonus of the patellas is predominant on the right. Abdominal reflexes are not evoked. Pathological foot reflexes on both sides - positive reflexes of Babinsky, Poussep, Chedok, Bekhterev, Zhukovsky, Rossolimo. The finger-nose test is performed with ataxia. Tremor of the head and torso - in a sitting position. Trunk ataxia - in a sitting position. Sits with outside support. Do not stand in the Romberg pose. There are no disturbances of superficial sensitivity on the trunk and limbs. There is a moderately pronounced decrease in deep sensitivity in the legs and feet. There are no violations of praxis or gnosis. There are no aphasic disorders. Sits in a wheelchair with support, but cannot move independently in a wheelchair. Urinary urgency, difficulty urinating, constipation.
Ophthalmologist: visual acuity - counting fingers from 1 m (in the ward). OU - large-scale nystagmus with a vertical component, pupils are symmetrical, reaction to light and convergence are weakened, limited outward movements, more on the left. Fundus of the eye: the discs are pale pink with a grayish tint, a narrow myopic cone, the vessels are narrowed, the macular reflex is preserved, the course of the vessels is correct. Conclusion: divergent paretic strabismus of the left eye, moderate myopia in both eyes, partial atrophy of the optic nerve in both eyes cannot be ruled out.
Ultrasound: bladder - volume 100 ml. The walls are thin and smooth. The content is homogeneous. No stones or additional formations were found. The orifices and lower thirds of the ureters are not dilated. The residual volume of urine is 100 ml (at the time of examination there is no urge to urinate).
Anticardiolipin antibodies were not detected, LE cells were not detected, antinuclear antibodies: within normal limits, antibodies to ds DNA: not detected, blood ELISA for ICD: IgM, IgG negative, Epstein-Barr virus capsid protein: IgM negative, IgG positive. Blood test for HIV: negative result. CSF analysis: colorless, transparent, no cytosis, normal protein; culture - no microflora detected. Diagnosis of R.S. (isoelectric focusing of oligoclonal IgG in the CSF): the pathological type of IgG synthesis was determined - oligoclonal IgG in the CSF and polyclonal IgG in the blood serum.
Treatment was carried out: pulse therapy with GCS (5.0 g of solumedrol per course), intravenous immunoglobulin 0.4 mg/kg, intravenous infusions of thioctacid, cytoflavin; Ceraxon, gliatilin, emoxypine, glycine, phenibut, grandaxin, omeprazole. High-dose therapy with interferon-β-1a 44 mcg (Rebif) subcutaneously 3 times a week was prescribed for a long time. At discharge, the neurological status showed no significant changes.
In clinical practice, a neurologist needs to take into account the possibility of the development of MS in children with other diseases of the central nervous system, including cerebral palsy, and be able to recognize new neurological symptoms against the background of the clinical picture of the existing disease.
The authors declare no conflict of interest.
*e-mail
Diagnosis of multiple sclerosis
Diagnosis of the disease involves visualization of foci of demyelination of the central nervous system using instrumental research methods (MRI with the introduction of intravenous contrast), confirmation of the autoimmune activity of the body after specific immunological tests and determination of functional disorders. MRI is considered the “gold standard” in diagnosing multiple sclerosis. This method allows you to identify the slightest foci of demyelination. MRI with contrast gives a clear picture of the pathology, in which the “old” and “new” foci of demyelination differ from each other. Based on these data, one can judge the activity of the disease.
Immunological tests are carried out to assess the activity of the pathological process. The biological material for these tests is mainly cerebrospinal fluid or blood. Detection of lymphocytic pleocytosis and increased myelin levels are nonspecific signs of multiple sclerosis.
An extended blood immunogram allows you to identify those disorders of the immune system that have become critical in the development of demyelinating disease of the nervous system.
The evoked potential method is becoming increasingly important in the diagnosis of multiple sclerosis. It allows you to detect demyelination of neurons at the initial stage of the disease. After analyzing the nature of the passage of the electrical impulse from the peripheral receptor to the central analyzer, the degree of damage to the components of this circuit is determined.
To verify the diagnosis of multiple sclerosis, W. McDonald’s diagnostic criteria are used all over the world. They compare the number of symptomatic episodes (attacks) and the conclusion of magnetic resonance imaging (MRI).
All results of additional research methods must correspond to the clinical picture of the disease. Multiple sclerosis is characterized by transient episodes of nervous system dysfunction that last at least 24 hours. Symptomatic attacks should appear no more than once a month.
Treatment methods for multiple sclerosis
Treatment of children with this disease is medicinal. There are two directions of therapy: pathogenetic and symptomatic.
The goal of pathogenetic treatment is to correct the dysfunction of the immune system and reduce the activity of autoantibodies against one’s own cells of the nervous system. For this purpose, anti-inflammatory drugs, immunosuppressants, and immunomodulators are used.
To reduce the severity of symptoms of multiple sclerosis, muscle relaxants, anticonvulsants, amino acids, B vitamins, antidepressants, neuroprotectors, psychostimulants and nootropics are used.
Physiotherapy is prescribed in the remission stage. The goal of non-drug treatment is to prevent complications of multiple sclerosis. Plasmapheresis, massage, and physical exercises are used for this.
Psychotherapy is an important component of the treatment process. This direction ensures the child’s social adaptation and prevents the development of depression and cognitive disorders.
General information about the disease
Nerve impulses are transmitted from cell to cell along long fibers called axons. They are covered with a myelin sheath, which facilitates and accelerates the movement of the impulse. The development of multiple sclerosis begins when the body begins to produce antibodies against the myelin sheath and gradually destroy it. As a result, the process of transfer of excitation is disrupted. For some time, the nervous system compensates for the disruptions, but as the disease progresses, the severity of symptoms steadily increases.
Symptoms of multiple sclerosis can appear in both men and women. Males get sick somewhat less frequently, but it is in them that the pathology is more severe and less responsive to treatment.
Make an appointment
Consequences of multiple sclerosis
The progression of multiple sclerosis can provoke a number of complications from other organs and systems. The most common consequences include:
- Infectious diseases. Due to dysfunction of the pelvic organs, children often experience infections of the urinary tract (cystitis, urethritis) and kidneys (pyelonephritis, chronic kidney disease). Multiple sclerosis often leads to breathing problems. Deterioration of pulmonary ventilation can provoke the occurrence of aspiration pneumonia.
- Movement disorders up to the development of plegia.
- Decreased vision, blindness.
- Hearing impairment, deafness.
- Depression and other mental disorders.
- Disability.
Cerebellar disorders
Coordination problems are common in multiple sclerosis and arise mainly from pathology in the cerebellum itself or when brain connections are disrupted. Patients may have either acute dysfunction associated with an acute exacerbation or chronic cerebellar problems with progressive disease.
Involvement of the cerebellar and brainstem connections occurs quite often during an exacerbation. Relapse of the cerebellum early in the development of the disease is associated with an increased risk of cerebellar damage during the subsequent course of MS. Experience shows that cerebellar involvement early in the disease worsens the prognosis. In a recent database study of approximately 15,000 patients who experienced a total of 50,000 exacerbations, cerebellar relapses accounted for approximately 10% of the total. They were more common in younger men and those with longer duration of progression.
It is estimated that 80% of patients with established MS experience tremors, which are especially common in patients with advanced disease. This is a consequence of unstable functioning of the cerebellum. Tremor can affect the limbs, trunk, vocal cords and head, but such a severe form is a relatively rare consequence of sclerosis.
Thus, cerebellar dysfunction may be a clear indicator of progressive MS. In general, this entails increased disability and poor prognosis.