Weakness in the legs or sudden awkwardness in movement after a hot bath may be symptoms of multiple sclerosis, an autoimmune disease of the nervous system that can lead to complete paralysis and blindness. In Russia, it is still confused with senile dementia and they are very surprised that both active young people and children are susceptible to it. On May 30, the International Day against Multiple Sclerosis, co-chairman of the All-Russian Union of Patients and president of the All-Russian Organization of Disabled Persons with Multiple Sclerosis, Yan Vlasov, told Taki Dela how patients with this disease live and what symptoms they need to pay attention to.
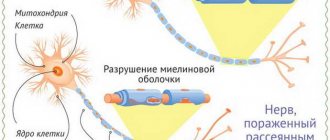
Photomicrography of the destruction of the myelin sheath of neurons of the nervous systemPhoto: Marvin 101/Wikipedia.org Yan Vlasov, MD, co-chairman of the All-Russian Union of Patients and President of the All-Russian Organization of Disabled Persons with Multiple SclerosisPhoto: from personal archive
What is multiple sclerosis
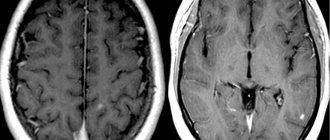
In multiple sclerosis, the immune system malfunctions and begins to attack the brain, damaging nerve cells. Sclerotic plaques - the connective tissue that remains at the site of such injuries - can appear in any part of the brain and spinal cord, which is why the disease is called multiple sclerosis.
Multiple sclerosis can develop in different ways: in one patient, exacerbations will be followed by complete or partial improvements, while in another, the disease will lead to complete paralysis within ten years. Scientists still do not know exactly why multiple sclerosis appears, but it is known that stress and strong negative experiences worsen the condition of patients, and positive emotions improve them.
In Russia, according to patient organizations, there are 150 thousand people with multiple sclerosis. The Ministry of Health register has three times less, just over 51 thousand people. This discrepancy appears because regional ministries of health, when providing data to the federal department, may take into account patients whose disease has progressed so far that medications will no longer help them, or may not take them into account.
How does multiple sclerosis manifest?
Multiple sclerosis is often called “the disease with a thousand faces” because its symptoms are not specific and can come and go.
“This is weakness in the limbs, especially worse after taking a hot bath or sauna, sudden attacks of incoordination without dizziness, recurrent visual impairment...,” lists Yan Vlasov. “All these symptoms are like a touch, they can even change during the day, they should alert a neurologist - this is where multiple sclerosis begins.”
It is a big mistake on the part of patients and their environment not to take these symptoms seriously and postpone a visit to a neurologist. If the doctor doubts the diagnosis, he can refer the patient to a center for help with multiple sclerosis. Information on regions can be found on the website of the All-Russian Public Organization of Disabled Persons with Multiple Sclerosis.
The hospital can diagnose multiple sclerosis within a maximum of three months - and this is a big step forward, because until recently the diagnosis took several years. But this level of medicine is available only in large cities; in rural settlements and small towns there are often no specialized specialists and the necessary equipment.
For almost twenty years, the Russian Committee of Multiple Sclerosis Researchers has been traveling to different regions and holding two-day schools there on all aspects of the treatment and diagnosis of multiple sclerosis. Thanks to this, there have been fewer cases where a sick person from a small town found out his diagnosis only a year or three after the first manifestation.
“We really hope that in the next six years they will create a system for standardizing specialized medical care specifically for patients with multiple sclerosis,” says Yan Vlasov. — If we create a standardization system, create first-, second-, third-level medical institutions that deal with this problem, we will be able to easily cover rural areas, and yet two-thirds of our citizens live there. [Currently] the number of part-time jobs there is very high, the equipment available is low, and to the nearest populated area where there is - I’m not talking about a tomograph, at least a specialized specialist! - 500 kilometers each.”
Symptoms
Symptoms of multiple sclerosis most often appear between the ages of 20 and 40. Typically, a person notices symptoms after developing two or more different episodes of symptoms before MS is suspected.
The most common early symptoms of MS include:
- Tingling
- Numbness
- Body imbalance
- Weakness in one or more limbs
- Decreased vision or diplopia
- Other symptoms that are much less common are:
- Slurred speech
- Sudden onset of paralysis
- Impaired coordination of movements
- Cognitive impairment
As the disease progresses, symptoms such as spasticity, sensitivity to heat, fatigue, changes in thinking or perception, and sexual dysfunction appear.
- Fatigue. This is a characteristic and common symptom of MS. It usually appears in the afternoon and can be manifested by severe muscle weakness, mental fatigue, drowsiness. Feelings of physical exhaustion are not related to the amount of work done and many MS patients complain of extreme fatigue, even after getting enough sleep.
- Sensitivity to high temperature. Heat sensitivity: The onset or worsening of symptoms after exposure to heat (such as after showering) occurs in most people with MS.
- Muscle spasticity. Muscle spasticity is a common and often debilitating symptom of MS. Muscle spasticity usually affects the muscles of the legs and arms, and can affect the motor ability of the limbs.
- Dizziness. Many patients with multiple sclerosis experience a feeling of dizziness. The occurrence of this symptom is associated with a disturbance in the transmission of nerve impulses in a complex system that ensures body balance (vision, proprioception, etc.)
- Cognitive impairment. Problems with thought processes occur in about half of people with MS. There is a disturbance in concentration and memory impairment. 10% of patients experience severe cognitive impairment and lose the ability to care for themselves.
- Visual impairment. Vision problems are quite common in patients with MS. Visual impairment is mainly associated with optic neuritis and occurs in 55% of cases. As a rule, visual impairment rarely leads to complete blindness.
- Pathological sensations. Many patients experience various pathological sensations such as tingling with pins, itching, and pinpoint pain. As a rule, these symptoms are not life-threatening and can be relieved quite well with treatment.
- Speech and swallowing disorders. Some patients have problems with both swallowing and speech. This is due to damage to the nerves responsible for these functions.
- Tremor. This symptom is quite common in patients with multiple sclerosis and, unfortunately, is difficult to treat.
- Walking disorder. Gait disturbance is a fairly common symptom in multiple sclerosis. This is mainly due to muscle weakness or muscle spasticity. In addition, the cause may be a lack of coordination and balance of the body.
Rare symptoms of multiple sclerosis include breathing problems and seizures.
Symptoms fall into three categories: primary, secondary, and tertiary.
The main symptoms are a direct result of the demyelination process. Demyelination impairs the transmission of electrical signals to muscles (allowing muscles to perform motor function) and body organs (allowing them to perform their normal functions.) Symptoms include: weakness, tremors, tingling, numbness, balance problems, blurred vision, paralysis, and problems with function bladder or intestines. Modern treatments can control these symptoms.
Secondary symptoms are a consequence of the primary symptoms. For example, paralysis (the main symptom) can lead to bedsores, and bladder dysfunction can cause frequent, recurring urinary tract infections. These symptoms can also be treated, but the main goal is to prevent complications from occurring.
Tertiary symptoms are social, psychological, and professional-labor symptoms arising as a result of the patient’s disability and loss of ability to work to one degree or another. Depression, for example, is quite common in patients with multiple sclerosis.
Unfortunately, each patient’s symptoms manifest themselves differently, as does the progression of the disease. Some patients may have mild symptoms for years without progression. In other cases, the disease can progress rapidly over several months. And with a variety of symptoms, some may have some symptoms and not others.
How is multiple sclerosis treated?
Today, multiple sclerosis is considered incurable. However, with competent, properly selected treatment, you can improve the quality of life and extend the period without disability. If previously disability occurred three to five years after treatment, now with carefully selected therapy it can be delayed by 10, 15 and even 20 years. The lifespan of patients has also increased: now people with multiple sclerosis can live up to 72-75 years, whereas previously they died five years after receiving disability.
There is a particularly severe type of the disease - primary progressive multiple sclerosis. In such patients, at first there may be no obvious exacerbations, but the disease progresses twice as fast as usual and within ten years the person loses the ability to move independently and take care of himself. This year, the first and only drug in the world for this type of disease was registered in Russia - previously such sclerosis was considered incurable. According to a recent survey conducted by a public organization, 70% of neurologists admit that the drugs they previously prescribed to patients with primary progressive multiple sclerosis simply could not be effective. Now the main task is to ensure the availability of innovative therapy for all patients in need.
Patients with multiple sclerosis receive medications free of charge under the “Seven Nosologies” state program. However, as with any government procurement, there are interruptions in the supply of drugs - and then people who cannot stop therapy in order to prevent an exacerbation are left without drugs. A similar situation occurred in 2021. Interruptions still occur today - they are associated with irregular supplies, incorrect timing of the auction, or mismatching of the auction between the companies that supply the drug. “These are purely commercial matters that have nothing to do with the authorities or the patient. We are trying to ensure that there are fewer of these problems, but the greater the appetite of these structures, the more they are ready to gnaw each other’s throats, it is difficult to do something about it,” says Yan Vlasov.
Masha Runde, 29 years old
Graphic Designer
I learned about my diagnosis in 2013, during my last year at the institute.
In the summer, my arm became numb, my leg began to behave strangely - I thought it was a problem with my spine. I was lucky: at the spine clinic, a young doctor sent me for an MRI, and it immediately became clear what we were faced with. At first it was difficult because you lose what you had. I have gone through all the stages, and it seems to me that acceptance has only just arrived. When I came to the clinic, the doctors groaned and said: “Oh, what a horror, how unlucky your parents are.” I think it was my love of life that pulled me through.
I immediately told my mother about the illness. What's the point of hiding? She took it courageously, we are generally strong.
Something may happen to my body, but I am not only my body.
I don’t like to communicate with my own kind, because many cannot tune in to the fact that you can live with an absent-minded person. I am not a member of any patient groups. I am very empathic and can take on other people’s experiences and try them on myself, and this affects my condition. At the beginning of my illness, I talked to a girl with the same diagnosis, she had difficulty urinating, and I screwed myself up so much that it began to seem like I had the same problems. Since then I decided that I can’t and don’t want to do that. For the same reason, you can’t drag me to meetings of people with MS.
I have interests outside of my illness, and they help me live. I love my job, my friends, my child. In general, my life is not much different from the life of a healthy person. Yes, there are some physical difficulties, but overall this does not interfere with my life. When my husband and I started dating, I already had a diagnosis. I told him it would be difficult, but he was not afraid. Our child, as often happens, “happened” by accident. But it wasn't scary.
When I found out about the pregnancy, I immediately thought that she was about to be born. And I'm very happy. My daughter is like a booster: she gives me the feeling that I definitely have to live, that there is meaning. With her you think less about yourself, there is less time to feel sorry for yourself. Grandmothers don't help us. My position is this: grandmothers have their own children, and this is my child, and I must raise him myself. But my husband, of course, helps in many ways.
I won't say that I am a very responsible patient. At first I nursed my illness. It feels like it was convenient for me, because at any moment I could use it to justify my weakness and laziness. Now I don’t deny it, but I don’t need it to exist.
Illness is not my friend, I don’t drag it around with me - I just live.
I protect myself from stress, take care, love, take care of my health, regularly do MRIs. This is prevention. I haven't had any exacerbations for quite some time. MS is, in essence, auto-aggression: our immunity is trying to “extinguish” us. Therefore, it is necessary to exclude those things that kill in themselves: alcohol, smoking. And add what brings benefit and joy to the body: physical activity, proper nutrition. I think the most important thing for me was to stop self-criticism and to psychologically set myself up correctly.
A mistake that relatives of “scattered people” often make is overprotection. For example, I am strong enough to defend my personal space and say: “My business is my business, and you mind yours.” But many fall into this web: parents try to protect a person from all matters and worries. My grandmother is like this. I ask her for at least some work when I come to her, and she says: “Don’t do anything, don’t cook, I’ll do everything myself, weed the beds.” This is a kind of codependency, the belief that a person will not survive without you.
In fact, resources appear precisely when there is no strong guardianship. I couldn’t walk far for a long time; I felt weak in my legs. Although now I understand that there was a lot of ordinary laziness in this. But when my husband had to go to the hospital and the child had to be taken to kindergarten, strength came from somewhere. And now, when I see that my husband is doing too many things for me, I stop him. Relatives must remember that a person should be allowed to live, not everything taken away from him. When you know that everything will be done for you, there is no desire to strive for something, to do it yourself.
Of course, my mother worries about me. But she doesn't try to do everything for me. She allows me to live and deal with problems on my own. It’s harder for grandma to stop herself: this is the generation of “rescuers.”
When the pandemic began, it was a downfall for many “dispersed people.”
Less walking, less physical activity - that's all. Since then I’ve been scared to go outside, I’m afraid of falling. I live on Taganka, and when I left the house after winter and saw the raised tiles on the sidewalk, my body immediately began to feel chilled, I was afraid of tripping. Now I still go outside and feel how it energizes me! Physical activity is very important, it is stupid to underestimate it. Any activity helps create new neural connections in the brain. Someone will shift all responsibility onto the doctors and say: “That’s it, give me any medicine.” But relying only on medications is not my way.
Of course, I have limitations, I have a disability. In Moscow, there is already a more or less calm attitude towards a limping person, a person in a wheelchair, but not on the periphery. For example, in the village where my grandmother lives, I am a “star”. When all eyes are on me, I feel uncomfortable. This is limiting: you are ashamed of yourself, you don’t want to go out. I get depressed from time to time.
But I like the feeling of being overwhelmed: it gives me time to breathe and think about where to go next. I look for resources in it. I am quite emotional and tend to worry about everyone and everything. And depression is a period when I think only about myself and think through further tactics. I would even say that this is my favorite state.
It seems to me that it is impossible to give any universal advice to people who are sick. We are all different. You should focus on your feelings. You need to go through this whole path of acceptance, turn to a psychologist. In short, you can live. You need to live. Living is important. The main thing is not to write yourself off.
Problems of patients with multiple sclerosis
According to a study by the Research Institute of Neurology ten years ago, the suicide rate among patients with multiple sclerosis was seven times higher than the population average. Now this figure, according to experts, has decreased, but the problem of social disorder remains. In three quarters of cases, patients with multiple sclerosis experience marriage breakdowns, and 80% of them are forced to look for a new job - taking into account their condition. “It’s mostly young people,” says Yan Vlasov. “The person is left alone: the children are still small, the parents are already elderly, there is no one to help him.”