Schizophrenia is a fairly common mental illness. It is manifested by disturbances in thinking, perception, emotional-volitional disorders and inappropriate behavior. The term “schizophrenia” was proposed by the Swiss psychopathologist E. Bleuler. Literally it means “splitting of the mind” (from the ancient Greek words “σχίζω” - split and “φρήν” - reason, mind).
Historical information about schizophrenia
The first information about schizophrenia-like symptoms dates back to 2000 BC. From time to time, many prominent physicians from different eras also described similar psychotic disorders. In his work “The Medical Canon,” Avicenna spoke about severe madness, partly reminiscent of schizophrenia. Pathology began to be studied in more detail only at the end of the 19th century. The German psychiatrist E. Kraepelin (1856-1926) observed adolescent patients suffering from various psychoses. In the process of research, he found that after some time all patients developed a similar state of special dementia. It was called “dementia praecox” (dementia praecox). Other psychiatrists supplemented and expanded information about the symptoms, course and outcomes of this disease. At the beginning of the twentieth century, the Swiss psychopathologist E. Bleuler proposed introducing a new name for the disease - “schizophrenia”. He proved that pathology occurs not only at a young age, but also in adulthood. Its characteristic feature is not dementia, but a “violation of the unity” of the psyche. The proposed concept of schizophrenia was recognized by all psychiatrists.
Changes in the brain
The emergence of new research methods, mainly MRI, CT and EEG, has made it possible to obtain quite a lot of interesting data about schizophrenia. In simple terms, scientists were able to find out what the brain of a person who has a schizophrenic disorder looks like.
It turned out that almost all schizophrenics exhibit atrophic processes in the following areas:
- medial temporal lobes;
- hippocampus;
- tonsils;
- superior temporal gyrus;
- parahippocampal gyrus.
In addition, all patients showed an increase in the lateral ventricle and a decrease in gray matter in the prefrontal cortex, temporal lobes and anterior cingulate cortex.
This information helps explain some of the symptoms of schizophrenia. Thus, damage to the hippocampus, which is responsible for short-term memory and spatiotemporal orientation, causes the development of dementia in schizophrenia. Disturbances in the prefrontal cortex affect cognitive functions, etc.
In this way, doctors were finally able to see what was happening in the brain of a patient who had schizophrenia. But the answer to the main question related to the etiology of the disease has not yet been received. Is it possible that doctors are now able to identify a schizophrenic disorder at an early stage, that is, before its exacerbation, which leads to the main problems in the life of a schizophrenic patient.
Why does schizophrenia develop?
Despite the high level of development of modern medicine, it has still not been possible to establish the exact cause of this disease. Psychiatrists are more inclined to the genetic theory of the occurrence of schizophrenia. It says: if there is a person with schizophrenia in the family, then his blood relatives have a high risk of developing this pathology. However, the mode of inheritance and molecular genetic basis of the disease are unknown. An important role in the development of schizophrenia is played by personality traits, low social status (poverty, poor living conditions, dysfunctional family, etc.), various diseases (drug addiction, alcoholism, chronic somatic pathologies, traumatic brain injuries, prolonged psychotraumatic situations, etc.) Sometimes The onset of schizophrenia is preceded by stress, but in most patients schizophrenia occurs “spontaneously.”
Typical forms of the disease
Typical forms of schizophrenia include paranoid, hebephrenic, catatonic and simple forms.
Paranoid form (F20.0)
Most often in their practice, psychiatrists encounter the paranoid form of schizophrenia. In addition to the main signs of schizophrenia (impaired thinking, autism, decreased emotions and their inadequacy), the clinical picture of this form is dominated by delirium. It typically manifests as delusions of persecution without hallucinations, delusions of grandeur, or delusions of influence. Signs of mental automatism may occur when patients believe that someone from the outside is influencing their own thoughts and actions.
Hebephrenic form (F20.1)
The most malignant form of schizophrenia is hebephrenic. This form is characterized by manifestations of childishness and silly, absurd excitement. Patients grimace, can laugh for no reason, and then suddenly become indignant, show aggression and destroy everything in their path. Their speech is inconsistent, full of repetitions and words they have invented, and very often accompanied by cynical abuse. The disease usually begins in adolescence (12-15 years) and progresses rapidly.
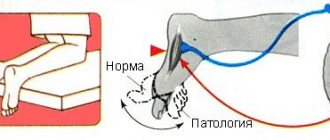
Catatonic form (F20.2)
The clinical picture of the catatonic form of schizophrenia is dominated by motor dysfunction. Patients remain in unnatural and often uncomfortable positions for long periods of time without feeling tired. They refuse to follow instructions and do not answer questions, although they understand the words and commands of the interlocutor. Immobility in some cases (catalepsy, a symptom of a “mental (air) cushion”) is replaced by attacks of catatonic excitement and impetuous actions. In addition, patients can copy facial expressions, movements and statements of their interlocutor.
Simple form (F20.6)
The simple form of schizophrenia is characterized by an increase in exclusively negative symptoms, in particular, apathetic-abulic syndrome. It is manifested by emotional poverty, indifference to the world around us, indifference to oneself, lack of initiative, inactivity and rapidly increasing isolation from the people around us. At first, a person refuses to study or work, breaks off relationships with relatives and friends, and wanders. Then, gradually, he loses his accumulated knowledge and develops “schizophrenic dementia.”
Atypical forms of the disease
In the clinic of atypical forms of schizophrenia, non-standard, not entirely characteristic signs predominate. Atypical forms include schizoaffective psychosis, schizotypal disorder (neurosis-like and variant), febrile schizophrenia and some other forms of schizophrenia.
Schizoaffective psychosis (F 25)
Schizoaffective psychosis is a special condition that is characterized by the paroxysmal occurrence of schizophrenic (delusional, hallucinatory) and affective symptoms (manic, depressive and mixed). These symptoms develop during the same attack. At the same time, the clinical picture of the attack does not meet either the criteria for manic-depressive psychosis or the criteria for schizophrenia.
Schizotypal disorder (neurosis-like variant) (F 21)
The neurosis-like variant of schizotypal disorder is manifested by asthenic, hysterical symptoms or obsessive phenomena that resemble the clinic of the corresponding neuroses. However, neurosis is a psychogenic reaction to a traumatic situation. Schizotypal disorder is a disease that occurs spontaneously and does not correspond to existing frustrating experiences. In other words, it is not a response to a stressful situation and is characterized by absurdity, deliberateness, and isolation from reality.
Febrile schizophrenia
In extremely rare cases, acute psychotic states with signs of severe toxicosis occur, called febrile schizophrenia. Patients experience a high temperature, and the symptoms of somatic disorders increase (subcutaneous and intraorgan hemorrhages, dehydration, tachycardia, etc.). The clinic of mental disorders is characterized by clouding of consciousness, the appearance of delusions of fantastic content and catatonic syndrome. Patients are confused, rush around in bed, make meaningless movements, cannot say who they are and where they are. Febrile schizophrenia should be distinguished from neuroleptic malignant syndrome. This is a fairly rare life-threatening disorder associated with the use of psychotropic drugs, most often antipsychotics. Neuroleptic malignant syndrome is usually manifested by muscle rigidity, increased body temperature, autonomic changes and various mental disorders.
Rare forms of delusional psychoses
Rare forms of delusional psychoses include chronic delusional disorders (paranoia, late paraphrenia, etc.), acute transient psychoses.
Chronic delusional disorders (F22)
This group of psychoses includes various disorders in which chronic delusions are the only or most noticeable clinical sign. The delusional disorders observed in patients cannot be classified as schizophrenic, organic or affective. It is likely that the reasons for their occurrence are genetic predisposition, personality traits, life circumstances and other factors. Chronic delusional disorders include paranoia, tardive paraphrenia, paranoid psychosis, and paranoid schizophrenia with sensitive relational delusions.
Paranoia (F22.0)
Patients suffering from paranoia are often suspicious, touchy, and jealous. They tend to see the machinations of ill-wishers in random events, remember grievances for a long time, do not accept criticism, and treat the people around them with acute distrust. Often they have overvalued delusional ideas of grandeur and/or persecution, on the basis of which patients are able to build complex logical conspiracy theories directed against themselves. Often those suffering from paranoia write a huge number of complaints against imaginary ill-wishers to various authorities, and also begin lawsuits.
Acute transient psychoses (F23)
The clinical picture of acute transient psychosis develops after a fleeting period of confusion, anxiety, restlessness and insomnia. Psychosis is characterized by the appearance of acute sensory delirium with rapid changes in its structure. Most often, delusional ideas of influence, persecution, relationships, staging, false recognition and delusions of a double arise. Hallucinatory experiences, true auditory and pseudohallucinations are possible. As a rule, they are unstable and prone to changing each other quickly.
Symptoms
Before describing the changes in the brain of a person with schizophrenia, it is worth spending a little time on its symptoms. Psychopathology has many forms. It is a polymorphic disease that can develop according to different scenarios. But, in general, all its signs are divided into two groups:
- Negative: apathy, abulia (lack of will), lack of motivation, suicidal thoughts and other symptoms of a depressive type. Their presence indicates the passivity of the mental apparatus.
- Positive (productive): delusions, obsessive actions, hallucinations and catatonic disorders. Their appearance indicates mental activity.
Usually before an attack there is an increase in negative symptoms. Then the active phase begins with positive signs. If it is possible to put the patient into remission, delusions and hallucinations are replaced by residual negative symptoms.
In severe cases, one phase is superimposed on another, as a result of which the patient is both apathetic and, for example, hears voices or is delirious. This usually happens with resistant schizophrenia, when the patient develops resistance to drug therapy. But often it is the alternation of active and negative stages of the disease that occurs. The first is also called an exacerbation or attack.
Continuous schizophrenia
This type of schizophrenia is characterized by steadily progressive dynamics. Depending on the degree of its progression, a malignant, moderately progressive and sluggish course is distinguished. With a continuous course, there are periods of exacerbation of schizophrenia symptoms and their weakening. However, full-fledged high-quality remissions are not observed. The clinical and social prognosis for the majority of such patients is unfavorable. The vast majority of patients undergo inpatient treatment or are in psychoneurological boarding schools. All of them sooner or later receive the first group of disability. In some patients, many years after the onset of the disease, the clinical manifestations somewhat decrease and, thanks to this, they are kept at home, remaining unable to work.
Early dysontogenesis syndrome
Early dysontogenesis syndrome in children with schizophrenia may be a consequence of a genetic predisposition to this mental disorder or brain damage in the early period of development.
Unlike adults, children with schizophrenia exhibit premorbid neurosensory disorders and neuromotor deficits, such as motor clumsiness and angularity or uncertainty when walking, in at least a third of cases. They develop self-service skills slowly.
Children with schizophrenia are characterized by a disharmonious type of development of cognitive activity: the predominance of the normative and advanced development of the operational side with a lag in the development of selectivity and the subject-content side. An unequal ratio of memorization success in different modalities was revealed in patients with schizophrenia and healthy children (Zvereva N.V., 2006).
According to some authors, in recent years, cases of early onsets of schizophrenia occurring in children with pronounced residual effects of residual organic cerebral insufficiency have become more frequent (Iovchuk N.M., 2007).
Periodic (recurrent) schizophrenia
With this type of schizophrenia, attacks of productive mental disorders occur periodically and are not accompanied by profound personality changes. Their number varies. Some people have one attack in their entire life, others have several, and others have more than ten. Attacks of schizophrenia can last from several days to several months. They can be of the same type (similar to each other) or heterogeneous (dissimilar to each other). The medical and social prognosis for periodic schizophrenia is usually quite favorable. This is explained by the insignificant severity of negative personal changes or their absence due to persistent intermission or practical recovery. The prognosis worsens with the severity, lengthening and frequency of attacks of recurrent schizophrenia.
Onset of the disease in children
Childhood schizophrenia is not common, but there are known cases of its occurrence in children as young as 2 years of age.
Here are signs that should make parents think about their child’s mental state:
- The child avoids communication with friends, becomes withdrawn, and prefers loneliness. He prefers quiet, sedentary pastimes to active, active games. Plays alone, sometimes in games invented by himself;
- refuses to perform hygiene procedures;
- the mood spoils for no reason. The child whines, is capricious for no reason;
- cannot defend himself, tries to hide from a conflict situation;
- the cognitive level is impaired. The child seems to take a step back in his development. Poorly assimilates new material and behaves according to his younger age;
- shows unmotivated aggression towards loved ones and peers, inadequate emotional reactions: if another child hits him, it hurts him, he cries, then this baby starts laughing;
- the child develops speech problems. Incomprehensible words appear, speech is scanty and abrupt.
The behavior of such children is noteworthy. For example, they pretend to be a bird. At the same time, their actions are appropriate: they imitate flight, claim that they are not a boy or a girl, but a bird, and “peck” at food.
At an older age, children call themselves by other names and communicate with imaginary friends.
In adolescence, schizophrenia manifests itself as emotional detachment. The teenager withdraws into himself and stops communicating with friends. At the initial stage of development of the disease, perverted desires appear. Children run away from home and become members of gangster groups, where they strictly obey the leader. They show aggression and sadistic tendencies. They demonstrate sexual perversions and are addicted to drugs and alcohol.
Particularly indicative is the duality of behavior. At home, the teenager behaves aggressively, laxly, argues and is rude, and rants a lot. And at school he becomes a different person: quiet, withdrawn, secretive.
As for such a severe form of the disorder as hebephrenic, at the dawn of its development such children become apathetic. Even if during the day they were not subjected to heavy mental or physical stress, they still feel overwhelmed, tired, and literally fall off their feet. They learn new material poorly. Sleep is disturbed and there is a rush of thoughts before falling asleep. Interest is lost and indifference appears. They remain inactive, abandon their studies, considering all efforts useless.
Aggression towards loved ones, especially mothers, while maintaining a normal attitude towards strangers is a very indicative symptom. Children call their parents guardians, believing that their real dad and mom are very influential and rich people. They just couldn't raise the child for some good reason, so they placed him in foster care.
An interesting fact has been established. Among children suffering from schizophrenia, the largest number are those who, before the illness, were known as obedient, flexible, problem-free children.
In childhood and adolescence, such manifestations are difficult to interpret correctly. They are usually mistaken for children's whims, the costs of upbringing, or a teenage crisis.
Paroxysmal-progressive schizophrenia
The most common paroxysmal-progressive course of schizophrenia occurs. This variant of the course is characterized by the presence of episodic attacks of schizophrenia with incomplete, low-quality remissions. Each attack leads to a personality defect, as well as increased delusions and hallucinations. The degree of progression of fur coat-like schizophrenia and the depth of the mental defect may vary. The clinical and social prognosis of this type of schizophrenia is determined by the rate of increase in personality changes, as well as the duration, frequency and severity of attacks. Fur-like schizophrenia with a rapidly developing mental defect has an unfavorable prognosis. A relatively favorable prognosis for sluggish fur-like schizophrenia. It is characterized by the rare occurrence of attacks that are non-psychotic in nature. The remaining cases are at intermediate levels between the indicated extreme options.
Differential diagnosis of schizophrenia
The diagnosis of schizophrenia is established after the duration of the disease has exceeded six months. In this case, there must be a significant impairment of social adaptation or ability to work. At its core, schizophrenia is a diagnosis of exclusion. To establish it, it is necessary to exclude affective disorders, alcoholism and drug addiction, which could lead to the development of psychopathological symptoms. Enormous difficulties arise in the differential diagnosis of catatonic and paranoid forms of schizophrenia from the corresponding forms of somatogenic, infectious, toxic, traumatic and other exogenous psychoses during their long-term course. The basis for constructing a diagnosis is specific clinical manifestations: emotional dullness, disturbances in the harmony of thinking and volitional disorders.
Suicidal behavior in patients with schizophrenia
The term “suicidal behavior” refers to a conscious action that is aimed at voluntarily taking one’s own life. In schizophrenia, we can talk about it only if the suicide is aware of his actions (is not in a psychotic state, and also does not have pronounced personality defects). In other cases, such behavior is considered auto-aggressive.
According to statistics, about half of patients suffering from schizophrenia attempted to commit suicide over a twenty-year period of illness. Of these, 10% were completed. Suicidal behavior is a direct indication for seeking consultation with a psychiatrist. And the best option is to hospitalize the suicidal person in a psychiatric hospital.
Schizophrenia can develop due to flaws in upbringing
One of the causes of schizophrenia is considered to be improper upbringing. In particular, we are talking about a lack of attention from the mother. In fact, blaming parents in this matter is baseless. No matter how coldly they treat their own child, this cannot provoke illness years later. Schizophrenia is a serious mental disorder, the development of which is caused by a whole complex of negative factors. Here are some of them:
- predisposition at the genetic level;
- head injuries;
- frequent stressful situations;
- brain dysfunction and so on.
There are still many questions in this regard to which scientists have not received accurate answers.
Treatment of schizophrenia
The vast majority of people suffering from schizophrenia need qualified help in a psychiatric hospital. Hospitalization allows for constant monitoring of the patient, detecting minimal changes in his condition. At the same time, the clinical manifestations of the disease are detailed, additional studies are carried out, and psychological tests are performed.
Despite the achievements of modern medicine, methods that would completely cure schizophrenia are still unknown. However, the methods of therapy used today can significantly alleviate the patient’s condition, reduce the number of relapses of the disease and almost completely restore his social and daily functioning. a major role in the treatment of schizophrenia . For this purpose, three groups of psychotropic drugs are used: antipsychotics, antidepressants and tranquilizers. They are used for a long time (from a week to several years, up to lifelong use). It is important to remember that the earlier treatment for schizophrenia is started, the better the prognosis awaits the patient.
Work for mentally ill people
It is difficult to get a job with schizophrenia, so disability is most often issued. It is impossible to obtain data on the employment of disabled people with mental illness in Cherepovets: the employment department does not keep such statistics.
Sergey, 45 years old. Diagnosis: schizophrenia
I have a second disability group. When I returned from the army, I worked at a factory in a furniture workshop for a year and a half, but left due to layoffs. He went to work at a construction site as a carpenter, but didn’t work for long. It happens that your thoughts run wild, you can’t sleep at night because of it, and in the morning you simply are not able to go to work. He did not stay in each of the new places for longer than three months. Then to the hospital, and from there it’s no longer convenient to come to the old place. I worked as much as I could: for private owners, with my father. Now it’s hard for me without work - my pension is only nine thousand. But no one will take it for two weeks or pay any money.
Peter, 25 years old. Diagnosis: schizotypal disorder
I work via the Internet: no eight-hour working day, no strangers, no need to explain anything to them or stand at the cash register. I can even write to people online and it's much easier than talking to them in person. I write poetry and would like to perform somewhere with them, but for now this is not possible. Poems give me meaning in life, it helps me. I think this is a good activity for my health, because if there is at least some meaning to existence, it gives me strength to fight.
Treatment with psychotropic drugs
Antipsychotic therapy is indicated in the presence of an acute condition. The choice of drug depends on the clinical symptoms of the attack (exacerbation). In case of dominance of psychomotor agitation, hostility, aggressiveness, antipsychotics are used, which have a predominant sedative effect (tizercin, chlorpromazine, chlorprothixene). If hallucinatory-paranoid symptoms predominate, “powerful” typical antipsychotics are prescribed that can fight them (haloperidol, trifluoperazine). The polymorphism of clinical symptoms requires the use of typical antipsychotics that have a broad antipsychotic effect (mazeptil or piportil). Sluggish schizophrenia is treated with low or medium doses of antipsychotics and antidepressants. In the case of sluggish schizophrenia, accompanied by phobias and obsessions, sedative tranquilizers (Relanium, phenazepam, alprazolam, lorazepam) are used.
Dealing with the side effects of antipsychotic medications
Long-term use of antipsychotics very often leads to drug intolerance. It manifests itself as side effects on the nervous system and the development of complications (tardive dyskinesia and neurolepsy). In such situations, antipsychotics are prescribed that do not cause or practically do not cause unwanted neurological symptoms (Leponex, Zyprexa, Rispolept). If dyskinesia occurs, antiparkinsonian drugs (akineton, napam, cyclodol, etc.) are included in the therapy. If depressive disorders appear, antidepressants are used (rexetine, anafranil, ludiomil, amitriptyline, etc.). You should know that all prescriptions are made and adjusted by a doctor. Spontaneous discontinuation of medications is prohibited. This is fraught with a high risk of relapse.
Advice for relatives of someone with schizophrenia
Schizophrenia is a serious illness, both for the person himself and for his close circle. However, if a person is not able to understand that he is sick, the family is simply obliged to recognize the disease and seek help from a psychiatrist. It's time to dispel existing stereotypes that it is impossible to help a person with schizophrenia. Maybe. With properly selected therapy, long-term, high-quality remissions are achieved with full restoration of ability to work over a long period of time. The main thing is to recognize the disease in time and begin treatment. If this is not done, the person will usually face emergency hospitalization in a state of psychosis. Don't wait until the worst happens to take action. Relatives are the only people who can change the life of a person with schizophrenia for the better. The quality of life of patients suffering from this disease largely depends on their support and their participation in the recovery process. If you suspect someone close to you has schizophrenia, contact a psychiatrist immediately.
We also recommend reading the article about low-grade schizophrenia.
Voice in my head
A classic symptom of schizophrenia is a voice in the head. Everyone has an inner voice, and this is normal - this is how a person thinks. But a schizophrenic’s voice is foreign in nature, and the patient cannot control it. Usually the voice in your head comments and gives advice. Doctors call imperative, ordering voices the most terrifying. Under their influence, the patient may commit wrong actions, crimes or suicide.
Another symptom is vivid paranoid or fantastic delusions.
Peter, 25 years old. Diagnosis: schizotypal disorder
I live on the edge. It’s hard for me when there are people around, it seems like someone is reading my thoughts. Because of this I don't ride buses. For example, I’m reading Sartre (I call it “bullshit book”), I’m interested, I think existentialism is cool, and I like the book. And then a feeling creeps in: suddenly on pages 10 and 15 they changed something. Someone’s evil will (Satanists, Masons or someone else) changed something there on purpose, and it will hypnotize me, influence me, change my whole life. And I start to obsess. Now I understand that this is nonsense, I can include criticism, but at that moment this nonsense begins to devour me. At this moment, a division occurs: on the one hand, I want knowledge, enlightenment, I want to strive for the great existentialist philosophers, but delusion prevents this, a struggle begins inside. I read, but I’m not completely in the book anymore. I try to understand what I’m reading, to assimilate it, but it doesn’t always work out.
Patients experience delirium in different ways. Peter talked about the “yielding” method. He learned to say to intrusive thoughts and feelings, “Okay, so be it.”
It doesn’t always help,” continues Peter. - But I know that you don’t need to fight delusion; trying to defeat it logically is impossible. You'll just get exhausted. It would seem that I can’t read books, but oh well, what can you do. It’s unpleasant, but in the next week you can do something else - I’m sure there are a lot of people who don’t read books at all. But the delusion begins to impose itself even after reading - the thought appears that I am forced to sacrifice reading in order to avoid the delirium, which means I surrender to it, and it really exists. And if someone changed the book, then he could change something in the music and in the video on YouTube. Because of this sequence, “Delusion of Reality” is born, in which everything that happens is done on purpose. This is scary! These states constantly haunt me in the background. There was no such thing that I felt the certainty of what was happening, there is always tension. It gets easier when you put it into practice.