11.02.2016
Maltseva Marina Arnoldovna
Head of the consultation department - neurologist, specialist in the field of extrapyramidal pathologies, doctor of the highest category
Migraine during pregnancy can occur even in women who have not previously suffered from this disease. About 25% of expectant mothers experience migraine with aura. It is difficult to even imagine how difficult it is for pregnant women to endure the terrible symptoms of migraine, since their body is already in critical condition. If you can no longer endure the pain, you should find a way out that would not harm either the pregnant woman or the baby.
What does migraine with aura mean?
Migraine with aura is a disorder characterized by recurrent episodes of reversible local neurological symptoms (aura), usually increasing over 5-20 minutes and lasting no more than 60 minutes.
“Aura” is a term by which doctors mean the following:
- Visual impairment
. These can be lines, lights, spots, flickering. In severe cases, loss of vision. All manifestations are reversible. - Sensory perception disorders
. It seems that goosebumps are crawling all over the body, the person feels tingling, and there may be areas of numbness. All this is also reversible. - Speech disorders
, which also go away along with the attack.
In 73% of migraine attacks with aura, the headache begins not after the end of the aura, but during the aura itself and can be accompanied by other migraine symptoms - nausea (51%), photophobia (88%) and phonophobia (73%) i Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138. . It happens that a panic migraine develops. Its complications are fear, anxiety, etc.
Migraines with and without aura are the same. A person usually feels a throbbing pain in one side of the head. Often it is concentrated in the eyeball. The pain intensifies with movement, sound and light stimuli. It can last from 4 hours to 3 days. At this time, it is impossible to lead a normal lifestyle. A person wants to be left alone in a dark and cool room, freeze, hide under the blanket. Typically, patients describe the pain as “bursting,” “splitting,” “about to burst,” “every sound like a hammer on the head.” And even after an attack, the consequences persist. The person is apathetic, tired and overwhelmed. It takes more than one day to recover.
Diagnostics
In the diagnosis of pathology, a carefully collected history and complaints of the patient, the frequency and duration of attacks, their symptoms, and neurological examination indicators are important. Criteria indicating migraine:
- The presence of 5 or more attacks of headaches that lasted from 3 hours to 3 days without taking painkillers. The patient describes the headache as unilateral, throbbing, intense, disrupting the usual way of life, and depends on physical activity.
- Presence of an aura. Suitable for classic migraine only. Signs of an aura are reversible, appear sequentially and last no more than 60 minutes; after the aura or on its background, a headache forms.
- Accompanying the attack with autonomic, sensory, motor, visual disturbances and sensitivity disorders.
- Absence of symptoms of other diseases that occur with headaches (brain tumors, mental disorders, spinal pathology, cardiovascular diseases, etc.).
A neurological examination does not reveal local changes in the nervous system (reflexes, loss/perversion of sensitivity, loss of coordination, etc.). In doubtful situations, the specialist prescribes:
- electroencephalography, rheoencephalography - assessment of bioelectric activity and brain rhythms (in a number of pathologies, including migraine, an accelerated frequency of oscillations and their high amplitude are observed);
- MRI – allows you to evaluate the vessels of the brain, neck, and identify multiple foci of ischemic origin;
- – makes it possible to exclude/identify brain tumors, cysts and aneurysms.
If necessary, radiography of the spine and skull is prescribed.
Differences from migraine without aura
Migraine without aura is called “classic”. Approximately 80% of patients suffer from it. A migraine without an aura manifests itself as throbbing pain at one point. It is not preceded by any visual, auditory or sensory impairment. Sometimes people don’t even realize that it’s a migraine, but think that they just have a headache. For this reason, patients do not go to the doctor, which is fraught with consequences.
You have migraine without aura if the following symptoms are present:
- 5 episodes of pain.
- The attacks last from 4 to 72 hours if you do not take medication.
- The pain throbs and is concentrated on one side of the head. The forehead, neck, and then the face or back of the head may hurt.
- With any physical activity the pain gets worse.
- There may be nausea, fear of light, sounds, voices.
Treatment of atrial scotoma
Therapy of the disease is carried out by a neurologist, who sees the patient
dynamically. In this case, certain drug treatment is prescribed. The prognosis of the disease is favorable.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling Moscow 8 (daily from 9:00 to 21:00) or using the online registration form.
What are the characteristics of migraine with aura?
About 20% of patients experience an aura. But only a few say that it occurs with every attack. The most common symptom of an aura is visual disturbances. Less commonly – sensory organ disorders (tingling, numbness, goosebumps). Aura symptoms are divided into positive and negative. In the first case, something is felt, and in the second, the fields of vision disappear or the hands go numb. Another property of the aura is dynamism. That is, a gradual increase in symptoms, and then their gradual decline. Usually the aura is replaced by a headache, but sometimes the aura appears on its own.
Migraine with aura is characterized by the following symptoms:
- Two episodes of migraine without aura.
- The presence of an aura for 1 hour or more before pain occurs. In this case, the following neurological symptoms appear - one or more:
- visual disturbances – photophobia, blinking, black spots in the field of vision, flickering arches, lines, zigzags, incorrect perception of objects in the field of vision;
- sound disorders, mainly intolerance to any sounds;
- speech problems;
- sensory disturbances – tingling, burning, numbness, etc.;
- impairment of motor abilities, such as sudden weakening of muscles on one side of the body.
During pregnancy
Ocular migraine appears during pregnancy mainly in the first trimester. In the later stages of pregnancy, if attacks develop, this is usually the classic form of the disease. Most often, migraine of the eye occurs due to sleep and rest disturbances, as well as emotional instability. Self-treatment of the disease is strictly prohibited. To reduce the intensity of attacks and their frequency, strict adherence to a daily routine is required, which takes into account all the features of the pregnant woman’s condition. You will also need to reduce physical activity and avoid stressful situations as much as possible. Due to the fact that visual disturbances can lead to loss of orientation in space, at the first sign of an attack, a woman should sit down, or better yet, lie down.
The sooner a pregnant woman seeks medical help when an ocular migraine occurs, the higher the likelihood that painful attacks will not cause disturbances in the development of the child. Also, following the specialist’s instructions will make the period of bearing the baby more comfortable and will reduce the likelihood that headaches will persist throughout pregnancy. If treatment is not carried out at all, then there is a high probability that even after childbirth the problem will persist.
Causes of migraine
The mechanisms of migraine development are not fully understood. A predisposing factor in the development of the disease is hereditarily determined dysfunction of vasomotor regulation. Approximately 70% of migraine patients have close relatives with a history of migraine-like headaches i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. .
There are two groups of factors that influence the course of migraine: those that worsen the course of migraine as a whole and those that provoke an attack.
Factors that worsen the course of migraine . In a patient with migraine, factors such as emotional stress, frequent consumption of alcoholic beverages, and other environmental influences can cause a long-term (over several months or years) worsening of the disease in the form of an increase in the frequency and/or intensity of attacks.
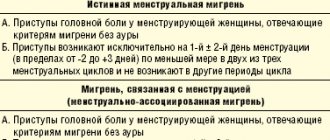
In patients with migraine, precipitating factors increase the likelihood of attacks; their effects usually appear within less than 48 hours. Despite the fact that migraine triggers have been well studied in a number of epidemiological studies (for example, the influence of menstruation i Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - P. 92-96.) and clinical (the effect of aspartame, chocolate, etc.) studies, in each individual case it is not always easy to establish a direct causal relationship between the provocateur and a migraine attack.
Factors provoking migraine paroxysms (migraine triggers) i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. :
- dietary: hunger, irregular nutrition, some foods (chocolate, cheese, nuts, alcohol (red wine), creams, yogurt, chicken liver, avocado, citrus fruits, bananas, concentrated soups, fried pork, sausages, pizza, coffee, cola, tea);
- hormonal: menstruation, ovulation, estrogen replacement therapy, oral contraceptives;
- psychological: emotional stress, anxiety,
- depression, fatigue;
- weather changes;
- exercise stress;
- lack or excess of night sleep;
- stuffiness, odors (smell of perfume);
- visual stimuli (flickering or bright light);
- cold;
- noise;
- staying on top.
Migraine - symptoms and treatment
Getting rid of migraine pain is a complex, complex task that requires not only drug therapy, but also lifestyle adjustments and non-drug treatment.
Migraine treatment includes:
- Lifestyle correction, informing the patient about the nature of the disease, behavioral therapy.
- Treatment of attacks - aimed at relieving a separate migraine attack, can be used in a single variant if attacks are rare.
- Preventive treatment - prescribed at the request of the patient or when attacks become more frequent and their severity increases.
How to get rid of migraine pain
As a rule, a patient with migraine begins to take simple or combined analgesics or NSAIDs on his own before contacting a neurologist. In this case, it is necessary to adhere to therapeutic doses of drugs, avoid drugs containing caffeine and codeine, due to the high risk of developing dependence with withdrawal symptoms. Abuse of such drugs can cause chronic daily headaches, which will significantly complicate further treatment.
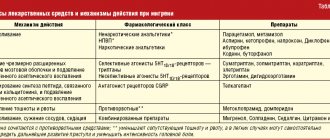
Medicines for the treatment of migraine attacks
| Group of drugs | List of essential drugs | A comment |
| Simple analgesics, NSAIDs (non-steroidal anti-inflammatory drugs) | Acetylsalicylic acid, ibuprofen, indomethacin, naproxen, diclofenac, paracetamol | Helps well with mild to moderate attacks |
| Antiemetics | Metoclopramide, domperidone, chlorpromazine (aminazine) | They are used for vomiting accompanying an attack; in mild attacks they can independently have an anti-migraine effect. Aminazine is rarely used - for uncontrollable vomiting and concomitant mental disorders |
| Triptans (selective 5HT1 serotonin receptor agonists) | Sumatriptan, zolmitriptan, naratriptan, rizatriptan, eletriptan | They are used when analgesics and NSAIDs are ineffective; they can be taken together. Concomitant use with antidepressants and ergotamine derivatives is contraindicated. |
| Narcotic analgesics | Codeine, tramadol | Used for severe attacks and lack of effect from other drugs. There is a risk of addiction and development of dependence |
| Combination drugs | Andipal, pentalgin, spasmalgon, citramon | They are not included in current recommendations due to the risk of overuse headaches. This type of pain is caused by painkillers if you take them too often. However, combination drugs are sometimes used for severe attacks |
Specialized drugs for the treatment of migraines are triptans . They bind to serotonin receptors and activate them. This suppresses the release of the key neurotransmitter CGRP, which is associated with the development of migraine. This mechanism blocks the main pathological link in the development of migraine. Taking triptans selectively constricts the vessels of the dura mater, reduces the permeability of the vascular wall and reduces inflammation and pain, as well as the intensity of the accompanying symptoms of migraine.
There are several types of triptans; the selection of the drug is carried out by a neurologist individually.
Basic principles of taking triptans:
- The doctor should teach the patient to distinguish between different types of headaches and to identify migraines.
- The sooner a patient takes the drug, the more likely it is to work. Medicine taken in the first minutes of an attack is effective in about 80% of cases. A triptan taken two hours after the onset of an attack is effective in 20% of cases.
- During a migraine attack, the gastrointestinal tract is paralyzed, causing the drugs to be poorly absorbed. Therefore, they are recommended to be taken together with prokinetics - drugs that improve the motility of the stomach, duodenum, and in some cases, the small and even large intestine.
- The lack of effect after the first dose of the drug does not indicate its ineffectiveness. It is necessary to take the drug for three more attacks.
What other medications help treat migraines?
At the request of the patient or in the event of an increase in the frequency of attacks and an increase in their severity, preventive treatment may be prescribed.
Medicines to prevent migraine attacks
| Group of drugs | List of essential drugs | A comment |
| Mono and combined drugs have predominantly vascular action. | — Vasobral (α-dihydroergocriptine mesylate, caffeine). — Bellataminal (ergotamine tartrate, phenobarbital, belladonna alkaloids). — Picamilon (N-nicotinoyl-gamma-aminobutyric acid sodium salt). — Nicergolin | A vasodilator, there is no indication in the instructions for use for migraines, but the drug reduces attacks well; it is contraindicated for changes in the heart valves. Not recommended for long-term use due to the risk of developing headaches; according to the instructions, it can be prescribed for up to three months Classified as a sedative. Thanks to ergotamine, it affects blood vessels and can be used for migraines. A nootropic drug that affects the blood vessels of the brain; according to the instructions, it can be used in the complex treatment of migraines Alpha adrenergic blocker, can be used to prevent migraines. Due to the good safety profile, long-term use is possible |
| Beta blockers | Propranolol, metaprolol, atenolol, timolol | Indicated for use in the presence of concomitant diseases: hypertension, arrhythmias, angina pectoris, anxiety disorder. Contraindicated in cases of low blood pressure, often observed with migraines, rare pulse (bradycardia), and heart failure. |
| Angiotensin type 2 receptor antagonists | Candesartan | Unlike beta-blockers, it can be used for congestive heart failure and bradycardia, in combination with migraine and hypertension |
| Anticonvulsants (anticonvulsants) | Valproic acid, topiramate | Reduce cortical excitability, prevent migraine attacks. Dose titration (slow increase under supervision) is necessary. Topiramate is also used for chronic migraine. |
| Antidepressants | Amitriptyline, venlafaxine | They are used as a second choice for migraine prevention. Increases the pain threshold and has its own analgesic activity. The analgesic effect is achieved earlier and in smaller doses than the antidepressant effect. Can be used for depression accompanying severe and frequent migraine attacks |
| Botulinum toxin type A | OnabotulinumtoxintypeA | Recommended for the treatment of chronic migraine. It is used in the form of injections into certain muscles of the face and neck. Has a wide range of side effects. To be used only by a certified professional in the field |
| Steroid hormones | Prednisolone, dexamethasone | They are used as part of complex therapy for severe migraine, often in a hospital setting. Efficacy has not been fully studied |
| Monoclonal antibodies | Erenumab (Irinex in Russia, Aimovig in foreign countries), Fremanezumab (Ajovy), Galcanezumab (Emgality) and Eptinezumab (Vyepti), calcitonin gene-related peptide (CGRP) receptor blockers. | Highly effective for migraine prevention, long-term safety of use has not yet been sufficiently studied. Disadvantages: high market price |
At the end of September 2021, the FDA (Food and Drug Administration) approved a new drug for the treatment of migraines - Qulipta (Atogepant). It targets the neuropeptide CGRP, which is elevated in migraine and is considered a major biomarker of the disease [39].
Non-drug treatments for migraines
Non-drug treatment methods include biofeedback (BFB), a computer-based method of self-regulation, as well as transcranial electrical stimulation methods, hyperbaric oxygenation and other options for individually selected physical therapy. The effectiveness of these methods has not been sufficiently studied and is questioned.
Is it worth using folk remedies to treat migraines?
According to the WHO definition, “Traditional medicine is the sum total of the accumulated knowledge, beliefs and skills, based on the theories, beliefs and experiences of indigenous peoples and peoples of different cultures, whether we can explain them or not, that are used to maintain health and also for the prevention, diagnosis and improvement of physical and mental disorders” [25].
When it comes to faith and traditions, it is difficult to talk about their scientific evidence. Herbal medicine is closest to the concept of traditional medicine - treatment using herbal remedies that contain medicinal substances. However, large and well-controlled studies have not been conducted to prove the effectiveness of herbal medicine.
There are some pilot studies showing the effectiveness of some herbal remedies:
- Oil of lavender, peppermint, basil, anise. Shown to be effective in reducing migraine attacks [34][35][36].
- Butterbur (Petasites hybridus). Can reduce the frequency and severity of migraine attacks [27].
- Hemp and mushrooms of the genus Psilocybe. Shown to be effective for migraine [28][29]. However, their use is contrary to the legislation of the Russian Federation.
- Willow bark extract. Contains an anesthetic substance - acetylsalicylic acid, so it can be effective for migraines.
- Ginger. Ginger powder has been shown to be effective and well tolerated for migraine [30].
- Caffeine in coffee, tea, mate. Shown to be effective in combination with paracetamol and sumatriptan [31].
- Coriander. Coriander syrup has been shown to be effective in reducing the duration and frequency of migraine attacks and reducing pain [32].
- Dong cai root (Angelica sinensis). Can relieve migraine symptoms [33].
- Valerian. There is no evidence that valerian objectively helps with migraines. However, thanks to its calming and hypnotic effect, a positive effect is possible during migraine attacks.
- Pyrethrum (Tanacetum parthenium). There is insufficient data to demonstrate efficacy compared with placebo [26].
- Rosemary, linden, raw potato cuttings, honeysuckle, horseradish, mullein, yarrow, teaberry, dried cherries, alecost, bananas, spinach, salmon protein, watermelon, common hops, betoni, evodia. Evidence of effectiveness is insufficient.
The use of folk remedies for migraine should be viewed critically. The reason for this is the lack of evidence and contradictory data, as well as the fact that most of the studies were conducted in countries where the requirements for clinical trials are lower than in the USA and EU countries.
You should be especially careful with the use of herbal medicine in case of moderate to severe attacks and complicated migraine.
How to treat migraine during pregnancy
Features of migraine treatment in pregnant women:
- A full examination is carried out to exclude the secondary nature of the disease.
- Preference is given to non-drug methods:
- behavioral recommendations - adjusting work and rest schedules, avoiding stress, keeping a headache diary to identify and exclude migraine triggers;
- methods are used that are not used so often in the treatment of migraine in non-pregnant women due to the lack of evidence of their effectiveness: psychotherapy, biofeedback [37], physiotherapy methods - transcranial electrical stimulation, hyperbaric oxygenation (pressure chamber), acupuncture, osteopathy, massage.
Basic principles of drug treatment during pregnancy:
- Independent, uncontrolled use of medications without consulting a doctor is unacceptable.
- Any prescription must be justified; the benefit must outweigh the potential risk.
- Preference is given to therapy with one drug - the most researched and safe, to quickly stop the attack, in the minimum effective dose. The dose may exceed the average therapeutic dose, taking into account the metabolic characteristics of a pregnant woman.
- Prophylactic treatment should be avoided due to its duration and contraindications to most medications. However, prophylactic use is possible if there are several indications for prescribing one drug, for example, the use of beta-blockers for arrhythmia, arterial hypertension and migraine simultaneously.
- It is recommended to avoid prescribing any medications in the first trimester and two weeks before the expected birth.
- When taking medications, strict monitoring and timely diagnosis of the condition of the pregnant woman and fetus are necessary.
For ethical reasons, direct studies have not been conducted on pregnant women, so at the moment there is no drug for the treatment of migraines whose safety has been fully proven. Sumatriptan is the most researched and safest of the triptans used during pregnancy. Admission is possible if the benefit outweighs the possible risk [37]. For mild migraine attacks, paracetamol is used, for more serious ones, ibuprofen is used in the first two semesters; metoclopramide can be prescribed to enhance the effect. The use of these drugs during pregnancy is not considered completely safe; they are taken under medical supervision with caution and in a minimal dosage.
Types and symptoms of migraine auras
Let's look at the main types of auras and how they manifest themselves.
Visual or ophthalmological
This aura is called “classical”. With it, visual images appear - flashes of light, curved or straight lines, flickering objects, white or golden figures, spherical images, etc.
Symptoms develop over 5-30 minutes. Positive ones can be replaced by negative ones. The duration of the aura can reach 1 hour. The image usually appears in the center of the visual field. It gradually increases and moves to the periphery. A scotoma remains behind him
– dark, “blind” area. During the aura or within an hour after its appearance, pain occurs. When the attack ends, any disturbances go away without consequences.
Retinal
With such an aura, scotomas or blindness in one eye occur. Symptoms persist for up to 1 hour. The headache comes after scotomas in about an hour, but can also occur before them. This is a rare type of aura. There is an assumption that the symptoms appear due to spasm of the central retinal artery. In most patients, retinal migraine attacks alternate with migraine attacks with or without classic aura.
Auditory
Auditory auras are hallucinations with sound. Ringing in the ears may occur, and patients sometimes hear music or voices. Doctors associate this aura with epileptic activity in the cerebral cortex, in its temporal region.
Speech
It manifests itself as a speech disorder because it affects the speech centers of the brain. Before an attack of pain, for a few minutes, no more, it is difficult or impossible for a person to speak. He can rearrange syllables in words, letters, repeat the same thing. At the same time, the consciousness is absolutely pure.
Vestibular
This is an aura in the form of movement disorders - dizziness. A fairly common phenomenon that can be hidden or obvious. In the second case, a person “sicks” even with small loads. In the first, violations can only be detected within the framework of an examination. According to the ICD, 2 forms of vestibular migraine are distinguished:
- Basilar
- occurs rarely, mainly in teenage girls. The attack begins with visual disturbances, followed by dizziness, tinnitus, sensory disturbances, etc. Then, in 25% of cases, confusion occurs. Neurological symptoms persist for 20-30 minutes, then pain in the back of the head occurs. Without treatment, throbbing pain may persist for 2-3 days. - Paroxysmal dizziness of younger children
(benign). Occurs in children 1-4 years old. It manifests itself as short – from a few seconds to a few minutes – attacks of dizziness. The child loses stability, becomes anxious, and vomits. He may turn pale and sweat profusely. No headache. Attacks may recur over several months or years.
Vegetative
Often such auras are manifested by a feeling of heat, chills, cold, trembling; the face and neck may turn red or pale. Goosebumps may appear, and hairs may even rise on the skin. During an attack, the size of the pupil may change, and asymmetrically. Usually such an attack is part of a complex attack, and not an independent phenomenon.
Facts about migraine
Here are some key points specific to migraines:
- Migraine headaches are caused by dilatation of blood vessels and the release of chemicals from the nerve fibers surrounding these blood vessels.
- Migraines can lead to feelings of nausea, diarrhea and vomiting.
- Approximately 12% of Americans experience migraine headaches.
- Migraines typically occur in people between the ages of 15 and 55.
- Some migraine sufferers can clearly identify triggers or factors that cause their headaches, such as allergies, light and stress.
- Some people experience migraine attacks with a subjective disturbance called an aura.
- An aura can act as a prodrome preceding the onset of a migraine attack.
- Lifestyle changes can help reduce the frequency of migraine attacks.
- Conventional analgesics can stop or reduce pain.
Diagnosis of migraine with aura
The diagnosis is made by a neurologist, and it is he who should be contacted with such a problem as soon as possible. The doctor must rule out cysts, tumors, encephalitis and vascular pathologies that cause similar symptoms. Therefore, a neurological examination, CT or MRI of the brain is performed, and the patient is sent for a consultation with an ophthalmologist for examination and determination of visual fields.
An EEG (electroencephalography) is required, which provides information about the functional activity and characteristics of the brain biorhythm of a particular patient. Based on the EEG results, the doctor then selects medications for therapy.
How is diagnosis carried out?
An appointment with a neurologist begins with a conversation, during which you may be asked some questions:
- How exactly is your vision impaired? How often do attacks occur? How long does it take for them to go away? After what do they usually occur?
- When did you start noticing the first symptoms? What do you think this could be connected with?
- Do you have headaches?
- What diseases have you suffered during your life? Do you currently have chronic illnesses? Are you taking any medications?
When answering questions, try to provide the doctor with as much detailed and accurate information as possible. This will help establish the correct diagnosis. A neurological examination is then performed. A neurologist may refer you to an ophthalmologist and prescribe some studies and tests.
Features of migraine manifestations in children and pregnant women
In childhood, the peculiarity of an attack is its short duration, from 30 minutes to several hours, and bilateral pain. It becomes one-sided in adolescence. Most often, children experience pain in the temples, forehead, and periorbital area. The nature of the pain is also not the same as in adults. The pain is squeezing, pounding, slightly throbbing. Children describe the latter extremely rarely.
It is difficult for a child to talk about his feelings, so the intensity of pain is assessed using VAS - a visual analogue scale with points from 0 to 10. Scales with emoticons can be used - from smiling to crying.
During pregnancy, migraines can occur even in those who have not previously suffered from them. In 25% of cases it is migraine with aura. It is much more difficult to tolerate, and there is almost nothing to eliminate the pain due to the delicate position. The approved drugs - No-Shpa, Citramon or Paracetamol - do not help. During pregnancy, aura most often manifests itself as photophobia, withdrawal, intolerance to sounds and strong odors, very severe nausea and the urge to vomit. The main causes of pain during pregnancy:
- consumption of “dangerous” foods – cheese, chocolate, citrus fruits;
- lack of water in the body;
- constant lack of sleep because the stomach makes it very uncomfortable to sleep;
- stress, frequent worries;
- large weight gain;
- violation of metabolic processes.
Causes
Migraine attacks during pregnancy are usually triggered by specific factors. Migraine during early pregnancy can be caused by the following reasons:
- specific stresses for the body that are associated with the process of implantation of the egg and the beginning of embryo development;
- a sharp change in hormonal levels;
- dehydration due to changes in metabolic processes in the body and a woman’s insufficient attention to herself;
- the appearance of food intolerance against the background of early toxicosis.
Also, a number of women in the first trimester of pregnancy often experience migraine-provoking nervous tension due to constant worry about their condition, the development of the child and the upcoming birth.
In the second trimester, the woman experiences a significant improvement in her condition. The frequency of attacks decreases, and due to the ability to use more drugs, they become less painful. The main provocateurs of headaches during this period are the following factors:
- physical overload – it occurs if a woman does not reduce physical activity, continuing to lead the same lifestyle as before pregnancy. As a result of this, an attack occurs as a protest of the body against what is happening;
- strong emotional experience;
- sudden changes in weather - they affect a woman if she suffered from weather dependence even before pregnancy;
- inhalation of very sweet heavy odors.
In the third trimester of pregnancy, the intensity of migraines increases. Due to changes occurring in the spine, blood circulation begins to deteriorate significantly, which is why even a mild vascular spasm is enough to trigger a migraine attack. The main reasons that can cause it are:
- drinking a large volume of liquid at once - in order not to provoke an attack, you need to drink often, but little by little, thereby not causing a sudden flow of water into the blood;
- staying in an uncomfortable position, which significantly worsens blood circulation in the lower extremities;
- prolonged stay in a supine position, which also worsens blood circulation;
- eating spicy or spicy foods;
- strong excitement or prolonged nervous tension.
Migraines may persist for some time after childbirth due to hormonal changes in the body. However, this phenomenon does not always happen and is considered the exception rather than the rule for migraines in pregnant women.
How to treat migraine with aura and how to relieve pain effectively and quickly
Since it is almost impossible to avoid an attack if there is a trigger, you need to know ways to improve the condition, because migraine is not a death sentence.
The final diagnosis is made by a neurologist. He will tell you what to do, how to treat the disease, how to increase the intervals between attacks.
Treatment for migraines is based on eliminating the pain and making it happen as little as possible or go away altogether. NSAIDs or specific medications, most often triptans, may be used. Intravenous infusion therapy is also used to treat migraines. The effectiveness of pain relief is directly proportional to the time of taking the drugs. You can stop an attack when it has just begun. Unfortunately, many people miss this moment with the thought “what if it doesn’t hurt.” However, at the peak of an attack, the tablets have almost no effect, because with migraine gastrostasis in the intestines, the absorption of any substances is very difficult.
Alternative ways to alleviate the condition are physical activity, exercise therapy, physiotherapy, and psychotherapy. Massage of the collar area is especially useful, because muscle spasm in this area can provoke an attack. Recently, migraines have been successfully treated with injections of botulinum toxin type A. The injections make remission last longer, and in some cases relieve pain for a very long time.
Treatment of migraines using traditional medicine
Many traditional medicine methods can provide relief from pain.
Ginger root
Ginger has the ability to block prostaglandins, thereby reducing the severity of pain. The same principle applies to most NSPVs. Ginger tea is prepared at home. Ginger root is crushed, then added to boiling water and simmered for 10 minutes over low heat. Next, the tea is filtered and drunk plain or with lemon and honey.
Chamomile
Has an anti-inflammatory and calming effect. You need to take two tablespoons of chamomile in a glass of water and cook the mixture for 5 minutes over low heat. Next, you need to strain the broth and drink it plain or with lemon and honey.
Lavender
Lavender oil is used for inhalation. The solution is prepared as follows: a teaspoon of oil is diluted in three glasses of boiling water. Breathe over the resulting solution for 15 minutes. Lavender oil can be mixed with peppermint oil and apply the mixture to the temples, gently massaging it a little. It is best to combine massage and inhalation.
Characteristics of migraine
Migraine headaches are caused by a combination of dilation of blood vessels and the release of chemicals from the nerve fibers that surround these blood vessels.
During a headache attack, the dilation of the artery occurs, which is located on the outside of the skull under the skin in the temple area (temporal artery). This causes the release of chemicals that cause inflammation, pain, and further dilation of the artery.
Migraine, through stimulation of the sympathetic nervous system, leads to a feeling of nausea, diarrhea and vomiting. This stimulation also delays the emptying of stomach contents into the small intestine (affecting the absorption of foods), reduces blood circulation (leading to cold hands and feet), and increases sensitivity to light and sound.
According to research, approximately 12% of Americans suffer from migraines. Women get migraines more often than men.
This is a vascular headache that usually develops in people between the ages of 15 and 55. Approximately three-quarters of all migraine sufferers have a family history of migraine.
What happens if migraine is left untreated?
Migraine is not a harmless disease. The disease is identified by the World Health Organization as a risk factor for cerebral strokes. Numerous epidemiological studies have revealed correlations between migraine and stroke, especially in young women suffering from migraine with aura i Ashina M. Vascular changes have a primary role im migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430. . Migraine is associated with a 16-fold increase in the risk of stroke in pregnancy and the overall risk of cardiovascular events in women. Migraine can be a risk factor not only for stroke, but also for “silent” heart attacks and damage to the white matter of the brain. These changes most often occur in women suffering from migraine with aura, and are associated with severe and frequent migraine attacks i Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692. .
You shouldn’t treat the attacks as “survived and are fine”, you need to see a doctor and get treatment.
Why does eye migraine occur?
Scientists still cannot answer this question unambiguously. The disease is associated with disorders that occur in the eye:
- Spasms in the arteries of the retina - the inner layer of the eye, which contains light-sensitive receptors - rods and cones.
- Pathological changes in the nerve cells of the retina.
In addition, there are some known risk factors that increase the likelihood of developing ocular migraines:
- The disease is more common in women.
- As a rule, attacks begin to occur after 40 years of age.
- Having close relatives who suffer from eye migraines increases the risk.
- Some diseases: atherosclerosis, systemic lupus erythematosus, depression, epilepsy, sickle cell anemia.
Ocular migraine is accompanied by unpleasant symptoms, but it is usually not dangerous. Complete loss of vision is possible, but this is very rare. However, similar symptoms occur in other, more dangerous pathologies that can lead to blindness. A neurologist will be able to establish the correct diagnosis, prescribe effective treatment, and tell you about your prognosis and possible risks.
Migraine prevention
Prevention involves taking the medicine daily for a certain period of time. Which one is prescribed by a neurologist individually. This medicine will act not on the symptoms, but on the cause of the disease, preventing attacks from developing. However, drug prevention is not indicated for everyone. It is prescribed if:
- number of attacks – up to 8 per month or 2 per week;
- Even specific anti-migraine medications - Zomig, Relpax and other triptans - hardly help the patient;
- Triptans and analgesics cannot be taken due to contraindications;
- The patient has hemiplegic migraine, a rare hereditary disease that leads to stroke.
Forecast
The prognosis for patients with visual migraine is relatively favorable. This is due to the fact that, despite the incurability of the disease, it can be quite effectively corrected with the help of medications. Often, with the right treatment, it is possible to completely normalize the patient’s condition and provide him with the opportunity to live a full life.
If for some reason therapy is not carried out, then the prognosis becomes unfavorable, and sometimes even bad, if ocular migraine attacks begin to occur constantly, which is why the patient is unable to continue a normal life, completely losing his ability to work. Also significantly worsens the condition and the appearance of complications that develop with frequent intense and prolonged attacks, which the patient does not relieve with medications.
Migraine classification ICD-10
Migraine is coded G43: Diseases of the nervous system => Episodic and paroxysmal disorders => Migraine.
| Code | Disease |
| G43.0 | Migraine without aura (simple) |
| G43.1 | Migraine with aura (classic) |
| G43.2 | Migrainous status |
| G43.3 | Complicated migraine |
| G43.8 | Other migraine |
| G43.9 | Migraine, unspecified |
Sources:
- Ashina M. Vascular changes have a primary role in migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430.
- Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692.
- Esin O.R. Migraine: Basic principles of treatment and prevention / O.R. Esin [et al.] // Clinician. - 2011. - No. 4. - P. 10-16.
- Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - pp. 92-96.
- Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138.
- Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41.