Causes
The exact cause of migraine in a particular person can be difficult to determine. The most common predisposing factors include the following:
- increased intracranial pressure,
- osteochondrosis,
- stress,
- overstrain of the muscles of the shoulder girdle and head,
- heredity,
- following strict diets with strict restrictions,
- insufficient intake of water into the body.
Previously, doctors believed that migraines were a consequence of dilation of blood vessels in the brain, but this theory is now recognized as erroneous. The attack is caused by a number of biochemical processes that are triggered by neurons located in the cerebral cortex. Neurons, for various reasons that are not yet precisely known to specialists, begin to activate. This automatically releases inflammatory substances near the blood vessels. The final stage is inflammation of the vessel itself and the surrounding tissue, which manifests itself as a headache.
Migraines often affect members of the same family. More than 80% of patients inherit the disease from their parents. However, changes in the genetic makeup that would be responsible for this pathology have not yet been found.
Up to contents
Diagnosis of migraine with aura
Consultations with people who suffer from migraines and other types of headaches are carried out by a neurologist. It is he who makes the diagnosis, the first stage of which should be interviewing the patient. It is necessary to obtain the most complete information about the sensations before, during and after a headache attack.
Migraine, both with and without aura, must be differentiated from other diseases. These are organic and vascular pathologies of the brain that cause symptoms similar to those of migraine aura: ischemic stroke, TIA, dyscirculatory encephalopathy, cyst, encephalitis, intracerebral tumor.
To exclude these diseases, the patient is sent for a neurological examination. In the process of studying the clinical picture, the following studies are carried out:
- Dopplerography;
- Magnetic resonance imaging;
- X-ray;
- Computer research of the brain.
Laboratory tests are also required, among which blood and urine tests are mandatory. In addition, neurological examinations and, if necessary, consultations with specialists from other fields of medicine are carried out. So, first of all, an ophthalmologist is involved in diagnosing migraines to determine the visual fields and examine the fundus.
An important point in diagnosing this disease is conducting electroencephalography, which allows one to obtain information about the functional activity of the patient’s brain and the characteristics of its bioelectric rhythm. The results of this study are used in the selection of medications to eliminate the symptoms and causes of the disease.
Types of migraine
An attack of pain can be either severe, when a person is unable to engage in usual household activities, or not so pronounced.
By manifestations
- With an aura. An aura is a specific condition that precedes a headache. Patients report a number of symptoms:
- visual – sparkling lines in the form of zigzags or fog before the eyes. Bright flashes are followed by dropouts in visual fields (blind spots). Objects may appear larger or smaller than their actual size, or their color may also appear different;
- sensory – tingling and numbness in the body, sensation of crawling on the skin;
- motor – difficulty coordinating movements, muscle weakness, hemiparesis;
- speech disorders - hesitation, stretching of words.
Dizziness, weakness, and a feeling of unreality of what is happening are also common. Each symptom can last from 5 minutes to an hour. After completing this phase, at least one of the listed manifestations goes away.
- No aura. More than half of migraine cases resolve without an aura. This course is called simple, since the attack passes much easier. However, patients still suffer from excruciating throbbing pain, nausea and sensitivity to light and sound.
By frequency of attacks
In this case, migraine may be:
- episodic. Occurs rarely and passes without obvious symptoms;
- chronic. We are talking about the chronicity of the process if the attacks occur for more than 15 days within one month, and this is observed for 3 months or more.
There are also other types of migraines:
- flickering. It is characterized by a visual scotoma - light glare or zigzags. The attack is rarely accompanied by a headache, limited only to visual discomfort;
- basilar. It often begins in adolescence and is predominantly found in girls. Sometimes it is called migraine epilepsy, since changes specific to epilepsy are noted on the EEG (electroencephalogram) during an attack;
- cervical In addition to all the standard symptoms, the involvement of the neck muscles in the process is added. The pain spreads to the lower back of the head, temples and eye sockets;
- abdominal. Usually characteristic of children and manifested by abdominal pain in the form of attacks. They can last up to 3 days, or they can end in an hour. No other symptoms characteristic of gastrointestinal pathology are observed. Between attacks of pain, the child feels well and behaves as usual.
A doctor must deal with each case and identify migraine, distinguishing it from many similar diseases. According to statistics, only half of people suffering from headaches turn to specialists. However, such an attitude towards one’s health can lead to the progression of the disease.
Up to contents
Types of migraine aura
The most common aura is visual. It is characterized by the illusory appearance before the eyes of a blurry flickering spot, white, golden or multi-colored. The patient sees it in each eye, but only one half of the field of vision is always covered by the spot. When the spot disappears and vision is restored, an attack of cephalgia occurs.
In children, the aura manifests itself as “Alice syndrome” - a condition in which the patient sees distorted shapes and sizes of surrounding objects and various visual hallucinations. The visual type of aura is also characterized by black spots before the eyes, sparkling dots, and blurred vision. Retinal aura is rarely observed, which is expressed by the appearance of a spot in the center of the visual field and subsequent temporary blindness.
Sensitive aura is the occurrence of transistor sensory disturbances that precede a headache: tingling, numbness in the fingers of one hand with a gradual transition to the entire hand and one half of the head. Sometimes this sensation spreads to the corresponding half of the entire body. Ringing in the ears and auditory or olfactory hallucinations are also observed.
The aura may cause temporary speech disturbances. This may be slow pronunciation, slurred reproduction of words or individual sounds, or difficulty finding words. Less often, an aura manifests itself as a violation of motor function. This phenomenon is described by patients as muscle weakness moving down one arm and leg on one side of the body.
What can trigger a migraine attack
Often, patients seek to prevent headaches by identifying and eliminating the factors that provoke them. The following conditions can cause migraines:
- eating foods containing tyramine - smoked or dried meat, bananas, chocolate, dried fruits, citrus fruits, hard cheese;
- salt abuse;
- forced or conscious hunger for a significant period of time;
- lack of sleep or too much sleep;
- violation of work and rest schedules;
- excessive consumption of alcohol, tea, coffee;
- too bright lighting and loud sounds;
- flickering light;
- obsessive unpleasant odors (paint thinner, cigarette smoke, perfume, etc.);
- increase or decrease in atmospheric pressure;
- sudden change in weather;
- the arrival of cold weather;
- taking oral contraceptives or estrogen replacement therapy;
- consumption of products containing aspartate or glutamate;
- staying on top.
In pregnant women, migraine attacks become less frequent, which is due to changes in hormonal levels. Often in the second and third trimester the headache goes away completely. However, 4% of women first encounter this disease during the period of expecting a child.
The menstrual cycle also affects the exacerbation of migraines. Some patients suffer from this disease strictly two days before menstruation or three days after. Doctors attribute this to the fact that the level of estradiol in the blood serum drops during the outlined period. With the onset of perimenopause, the situation with migraine worsens, but women in menopause note relief.
Up to contents
Forms and complications of migraine
There are several types of this headache, as well as two main complications that can result from untreated migraine:
- Migraine without aura
- Migraine with aura (classical migraine with aura, aura without migraine, basilar aura, hemiplegic migraine, retinal migraine)
- Chronic migraine
- Complications of migraine (migraine status, migraine cerebral infarction, migraine-associated seizures)
The exact type of migraine will be determined by the doctor, but it is very important to understand that a headache can be accompanied by a variety of symptoms, and the lack of treatment can lead to severe complications, including the development of a stroke.
Diagnostics
Migraine is diagnosed solely by symptoms. There are no instrumental methods to confirm it yet. However, to exclude other pathologies that are sometimes hidden under the mask of this disease, MRI and CT examinations may be prescribed. If the resulting images do not reveal any alarming changes, then most likely the patient suffers from migraine.
Up to contents
Causes of migraine
Why does a migraine develop, why does it hurt so much and only in one area of the head?
At one time it was believed that the aura was caused by a local narrowing of the blood vessels in the head, and the pain itself was caused by the subsequent dilation of the blood vessels. Also, one of the theories suggests a change in the bioelectrical activity of certain areas of the brain. Another theory is that pain is mediated by irritation of the branches of the trigeminal nerve, which is responsible for sensitivity and pain in the face, part of the head and the meninges. Some studies have shown that the balance of neurotransmitters in the nervous system is also important, and when it is disturbed, migraines also occur.
Obviously, each of the mechanisms described above makes its own contribution, which causes such severe pain and such a number of accompanying symptoms.
Treatment
Migraine brings many unpleasant moments to the patient. Treatment for this disease is usually symptomatic. Episodic migraines are treated with abortive therapy, which is designed to stop the attack. Analgesics such as NSAIDs, triptans, and dehydroergotamine have proven themselves to be effective in the fight against migraine. Be sure to take the recommended dose of the drug within the first hour from the onset of the headache. If more time passes, the effectiveness will be much lower.
It is impossible to use medications uncontrollably, otherwise a drug-dependent headache may gradually develop. Only a qualified specialist can take into account all the indications and contraindications for a particular patient. A short-term sleep, immersing the head in warm water, fresh air, bed rest, a darkened room and rest can remove an attack or ease its course.
Up to contents
Treatment of migraine with aura
It is believed that migraine cannot be cured with drugs of nonspecific action, since they are ineffective in this case. And yet, in modern pharmacology, there are drugs that can alleviate the main symptom of migraine - a headache attack. These are antispasmodics and anti-inflammatory drugs of nonspecific action: aspirin, citramon, ibuprofen, no-spa, nikoshman, nicotinamide and others.
It is necessary to take these medications at the first sign of an aura. This allows you to prevent an attack or at least alleviate and shorten its course. It should be taken into account that this measure serves only to temporarily alleviate the general condition and relieve unpleasant symptoms, and the systematic use of drugs without the supervision of a specialist and their independent prescription is unacceptable. Therefore, consulting a doctor in this case is mandatory. Drug treatment should be carried out only according to the recommendations of the attending physician. As a rule, he prescribes several drugs for a comprehensive effect:
- Ergot-based products for constricting blood vessels and arteries;
- Analgesics;
- Antidepressants;
- Anticonvulsants;
- Saline solutions in case of dehydration.
Triptans are considered the most effective medications for preventing migraines. Drugs in this group are also always included in the list of medications prescribed for this pathology.
When prescribing medications, the doctor takes into account the patient’s age, the characteristics of his body’s condition and possible concomitant pathologies. If side effects occur, he eliminates the medications that caused them or replaces them with drugs with a similar effect. The doctor also prescribes a dosage of medications, which should not be exceeded to avoid intoxication.
Migraine prevention
For migraines, preventive prescriptions are also made if the patient experiences attacks more than once a month. Taking medications according to the regimen specified by the doctor makes attacks of the disease more rare, their duration becomes shorter, and the manifestations are not so pronounced. As a result, the disease does not become chronic, and the response to abortive therapy becomes better. Antidepressants, beta blockers and some other medications are prescribed for prevention.
Experts advise patients with migraine symptoms to sleep at least 8 hours a day, going to bed at approximately the same time. They should drink up to two liters of water per day and salt their food in moderation. It is advisable to limit the consumption of alcohol and caffeinated drinks or completely avoid them. Patients are often recommended to keep a special diary, where they should write down the following every day before going to bed:
- time of onset and end of the attack, its duration;
- preceding unusual sensations from the eyes or other body systems;
- in what part of the head was the pain felt;
- type of pain (pulsating - intensifying in time with the beat of the heart, squeezing - reminiscent of the sensations of squeezing the head with a hoop, stabbing - similar to sharp pricks with a needle, etc.);
- whether the pain was aggravated by physical activities, such as climbing stairs;
- severity of pain throughout the day (o);
- whether this condition was accompanied by nausea and how severe it was;
- whether there was retching or belching;
- whether there were cases of vomiting during the attack;
- whether the patient was irritated by ordinary daylight, whether he wanted to shade the room;
- did he seek to retire to a quiet place, hiding from the sounds that were familiar to him;
- factors that could presumably influence the occurrence of an attack;
- all drugs with an analgesic effect that were taken during the headache period. You need to indicate the dose and time of administration.
It is necessary to keep a diary for three or more months so that the conclusions from the entries made are reliable. This data helps the doctor evaluate the effectiveness of prescriptions and adjust them in a timely manner. The patient, having analyzed the events preceding the migraine, can consciously change his lifestyle, eliminating the factors that provoke the attack.
Up to contents
Migraine symptoms
Migraines can go through several stages. The prodromal phase occurs in every fourth case. A few hours before this, a disturbance in well-being appears. The person becomes lethargic, irritable, sensitive to sounds and smells. Less commonly, unexplained euphoria develops and hyperactivity appears.
The aura phase (noted in 20% of cases) is expressed in the occurrence of additional symptoms:
- visual impairment;
- the appearance of blind or flickering areas in the field of view;
- tingling in fingertips;
- numbness of part of the face;
- confusion of speech.
Neurological disorders may be more pronounced and resemble an ischemic attack. In this case, sensitivity is impaired, a shaky gait appears, and coordination of movements suffers. Less commonly, confusion, stupor, or disruption of the coordination of movement of body parts appears, which indicates involvement of the brain stem in the process.
The headache itself is pulsating and concentrated on one side. The frontotemporal region is most often affected. But the second half of the head may also be involved. The pain increases gradually, intensifies with physical activity, and weakens at rest. It can last from several hours to three days.
Phono- and photophobia is often associated; loud sounds and bright lights intensify headaches. Therefore, they prefer to be in a dark room in complete silence during an attack. Painful sensations can spread to other parts of the body. Migraines may be accompanied by pain in the neck or scalp.
Cephalgia is often accompanied by nausea, frequent urination, and sweating. Children experience digestive disorders. In older people, the number of accompanying symptoms decreases sharply or disappears completely.
After the attack ends, additional time is required to improve well-being. Many people continue to feel tired, fatigued, and have trouble thinking for several days. Some patients who have suffered a severe attack describe their subsequent state as feeling like a hangover. Disturbances in the functioning of the digestive tract and emotional disorders may persist. Sometimes low mood resembles depression.
Less commonly, after a migraine there is a surge of strength and a feeling of euphoria. How you feel may change with each attack.
Motrin® for migraines
Motrin® is a modern pain reliever. The drug has a high safety profile and clinically proven effectiveness for pain3 such as migraine. Motrin ® can act for up to 12 hours1, which allows you to take the drug 2 times a day to alleviate the condition.
Before use, read the instructions.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Migraine aura: what is it and how to treat it?
Dizziness
Migraine is a disease with an “ancient” history. It was studied by Hippocrates, Celsus, Galen, Aretaeus of Cappadocia and other famous doctors.
In the 12th century, descriptions of visual disturbances that occur at the onset of an attack appeared. This condition later became known as “migraine with aura.” And in the 18th century, works were written on this disease that are still relevant today [3].
Modern medicine has learned to effectively alleviate the suffering of patients, but has not yet fully revealed the mechanisms of this disease.
What is migraine?
This is a neurological disease that occurs with episodic or regular attacks. They may occur several times a year or month.
A migraine attack is a critically painful condition with a whole range of painful symptoms - an aura, severe throbbing pain on one side of the head, nausea, vomiting, intolerance to light, sounds, and sometimes even touch.
Migraine is divided into simple, without aura (MSA), and with aura (MA). The aura precedes an attack or occurs at the peak of pain. It presents visual hallucinations, as well as other neurological symptoms - coordination disorders, decreased sensitivity of body parts, tingling, and occasionally temporary paralysis. MA is much less common than MBA—it accounts for 20% of cases, and women are affected three times more often than men [2].
Migraine with aura - symptoms of the disease
An attack of MA has several phases [2,3]:
- prodrome;
- aura;
- headache;
- stage of attack resolution;
- postdrome.
Prodrome (precursor) is a period that occurs the same for MA and MBA. Hours or even days before an attack, a person may begin to experience:
- anxiety;
- irritability;
- decline or, conversely, a surge of strength;
- changes in the sense of taste and smell [4].
Then comes the aura stage. It develops dynamically, with an increase in intensity over 5–20 minutes, and completely disappears in an hour [2,4]. Visual disturbances are varied - flashes, sparks, lightning, bright balls, partial or complete loss of areas of vision. Both eyes are typically involved. Hearing disturbances, such as tinnitus, may also occur.
Less commonly, sensitivity disorders develop - tingling, goosebumps, burning, loss of sensitivity in the hands, which then rises to the neck, mouth and tongue. Sometimes the legs are involved in the process, movement is difficult, up to temporary paralysis. Sensory disorders occur after visual ones, but can develop without them [3].
Most patients experience several different aura symptoms during one attack, and their combination may vary [2].
The aura is replaced by a severe throbbing headache, nausea, vomiting, and intolerance to light. This period lasts on average several hours, but can last up to a day.
An attack of migraine with aura does not always reach the stage of headache; there is a so-called “decapitated migraine”. In this case, everything ends with an aura or minor discomfort occurs in the forehead area. More often, this type of attack develops with age, in people with a long history of illness. In general, migraine occurs more often in youth, and over time its intensity weakens [1,4].
Any migraine attack is resolved by long, deep sleep.
The final phase is the postdrome state. It manifests itself as a feeling of weakness, exhaustion, or vice versa - euphoria.
Migraine with aura - causes of the disease
Despite the ancient history of studying the disease, its causes have not been fully established.
It is known that a combination of neurogenic (related to the nervous system) and vascular factors plays a role in the development of an attack. Malfunctions in the functioning of nerve impulses affect the permeability and expansion of brain vessels, causing their swelling and inflammation. First, spasm of the blood vessels occurs, and then their pulsating expansion [3].
The aura occurs during the contraction phase. Ischemia (oxygen starvation) of certain parts of the brain develops, which provokes hallucinations and sensitivity disorders, and the type of aura depends on which part of the brain is involved in the process [2].
The next stage of the attack is a pulsating unilateral headache, observed during the vasodilation phase [3].
An attack can be triggered by strong physical and psycho-emotional stress, especially their combination. Moreover, this is not always stress, it can also be joyful excitement. For example, both an exam and a vigorous vacation [2].
Irregular eating or a certain type of food often causes an exacerbation. In a quarter of patients, an attack develops after eating cocoa, chocolate, nuts, smoked meats, citrus fruits, and cheese [2]. Migraine is, to a certain extent, a disease of character and temperament. It is associated with such psychophysiological traits as touchiness, irritability, excitability, and perfectionism [1].
According to the observations of ancient and modern doctors, this disease most often affects people with a strong will and passion for excellence, active, stubborn, selfish, but at the same time conscientious and responsible [1]. “Famous patients”: Gaius Julius Caesar, Charles Darwin, Alfred Nobel, Sigmund Freud, Pyotr Tchaikovsky, Ludwig Beethoven, Heinrich Heine, Guy de Maupassant [3].
Migraine with aura - treatment
This disease is quite “capricious” with a difficult to predict effect from medications. Therefore, therapy is selected carefully and strictly individually. To be examined and receive treatment, you must make an appointment with a neurologist.
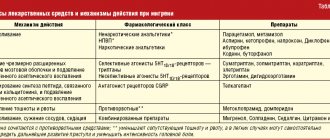
For migraines, regardless of their type, two types of drugs are used - specific and nonspecific. Specific ones are designed specifically for this disease, affect the mechanism of development of the attack and are aimed at stopping it. Nonspecific drugs are used for pain relief. These are analgesics and non-steroidal anti-inflammatory drugs [3].
If a person has more than two migraine episodes in a month, the doctor selects preventive medications for continuous use. For preventive purposes, antiepileptic drugs, beta-blockers, calcium channel blockers, antidepressants, vitamin B2, and magnesium are used. For vestibular migraines, which are associated with dizziness, drugs based on betahistine are used - it relieves an attack of dizziness, nausea and eliminates tinnitus, thereby alleviating the condition.
For prevention, it is important to maintain a sleep schedule and try to avoid stressful situations. If the attacks are related to diet, it needs to be adjusted. Considering the connection of migraine with stress and a person’s character, psychotherapy, autogenic training, and relaxation practices are indicated [3].
Bibliography:
1. Sanoeva M. Zh. Saidvaliev F. S. MIGRAINE - YESTERDAY, TODAY, TOMORROW. A MODERN VIEW AT THE PROBLEM. International Journal of Neurology. 2021.
2. A. N. Boyko, S. A. Sivertseva, N. F. Popova, P. R. Kamchatnov, O. V. Ryabukhina, etc. MIGRAINE WITH AURA. Journal of Neurology and Psychiatry. S.S. Korsakov. 2010, 11.
3. L. S. Manvelov. MILLENNIAL MIGRAINE. Lecture. Journal of Nervous Diseases. 2011, 1 (4).
4. Tabeeva G.R., Yakhno N.N. MIGRAINE. // GEOTAR-media. 2011.
Therapeutic exercise to improve the functioning of the cardiovascular system.
Co-author, editor and medical expert:
Volobueva Irina Vladimirovna
Born 09/17/1992.
Education:
2015 - Sumy State University, specializing in General Medicine.
2017 — Completed an internship in the specialty “Family Medicine” and also defended her master’s thesis on the topic “Peculiarities of the development of antibiotic-associated diarrhea in children of different age groups.”
Educational video “Headache and migraine”
1 - Frick et al. Efficacy and safety of naproxen sodium and ibuprofen for pain relief after oral surgery. Current Therapeutic Research. 1993;54(6):619-27. 2 — https://www.ncbi.nlm.nih.gov/pubmed 3 — Karateev AE. Naproxen: a versatile analgesic with minimal risk of cardiovascular complications. Modern rheumatology. 2016;10(2):70–77. 4 - in oral form. Based on these instructions for use and clinical studies of over-the-counter painkillers registered in the Russian Federation.
Forecast
If you are diagnosed with chronic migraine, you must be under medical supervision for 4–12 months (depending on the severity). Repeat visits to assess the effectiveness and correction of therapy should be carried out once every 2–3 months. For a good prognosis, the most important prerequisites are lifestyle changes, avoidance of attack provocateurs and migraine chronicity factors, control of painkillers, and adherence to the required duration of preventive therapy.