09.02.2016
Maltseva Marina Arnoldovna
Head of the consultation department - neurologist, specialist in the field of extrapyramidal pathologies, doctor of the highest category
Women suffer from migraines more often than men. This is probably why this disease is considered truly female. The reasons why migraines occur in women vary. So:
- Pain due to tension
Such pain most often overtakes those women who work at a computer for a long period of time or do written work. An uncomfortable posture, in which the head drops very low, causes the muscles to tense, and this becomes the cause of female migraines. You need to watch your back while sitting in front of the computer. It is very important to take a break for an hour and a half, at least for 10-12 minutes.
- Poor nutrition
Migraines can also be caused by substances found in food. Those who are prone to severe headaches should exclude all sorts of “junk” foods from their diet. This is sausage, frankfurters, ham. Sometimes even coffee causes sharp and unbearable pain.
- Migraine due to medications
This migraine occurs due to the reverse action of analgesics. Such pain can also be caused by an overdose of aspirin (3-5 tablets per day).
- Migraine before menstruation
Migraine occurs before the onset of menstruation, in order to prevent its onset, you must try not to overwork on such days, devote more time to walks on the street and proper sleep.
- Hidden depression
There is no need to keep all negative emotions inside yourself, this will not lead to anything good. Take more positive emotions from life, smile more often and relax.
Causes of migraine in women
Migraine is a chronic neurological disease. Refers to angiocephalgia (headache of vascular origin). It manifests itself as periodic or regular attacks of severe throbbing headaches, usually in one half of the head.
According to clinical studies of the World Health Organization, women are susceptible to the disease 4 times more often than men. This is due to the peculiarities of the functioning of the reproductive system and hormonal fluctuations.
Migraine often occurs in adolescence; 20-30% of patients aged 20-25 years suffer from pronounced manifestations of the disease.
The causes of the disease are not fully understood. Failures in the regulation of vascular wall tone can occur at any period of life against the background of changes in brain activity, autonomic vascular disorders, and hormonal imbalance. Lack of physical activity, obesity, chronic stress, unbalanced diet, smoking and alcohol abuse, hormonal changes - a number of factors can cause migraines and provoke an attack. The disease can be hereditary, with maternal transmission.
At risk are residents of megacities, patients with diabetes mellitus and endocrine disorders.
The following factors can trigger a migraine attack:
- stress;
- weather dependence;
- hormonal changes associated with the menstrual cycle (ovulation, PMS, menopause);
- overwork, mental and physical;
- taking certain medications, incl. oral contraceptives;
- pregnancy and lactation;
- excess/lack of sleep.
Triggering factors include:
- substances with a pungent odor;
- tight hairstyles and hats;
- excessive consumption of carbonated drinks and caffeine-containing products;
- certain food products (chocolate, citrus fruits, legumes, fast food, cheeses, fatty and smoked foods);
- alcohol;
- change of time zones.
Decapitated migraine - symptoms
Pain is the main symptom of most types of migraines. A decapitated migraine does not cause pain, but it does have other typical symptoms of a regular migraine. These symptoms depend on the phase of the migraine.
Prodromal phase
Occurs before the onset of a migraine and may begin several days or several hours before it occurs. Symptoms may include:
- difficulty concentrating;
- difficulties with speech and reading;
- fatigue and yawning;
- food cravings;
- irritability;
- muscle stiffness;
- nausea;
- sensitivity to light and sound;
- sleep disorders;
- frequent urination.
Aura phase
Only 20-25% of people with migraines have an aura phase. People with headless migraine have aura symptoms without the headache. Aura symptoms include:
- numbness and tingling in parts of the body;
- temporary loss of vision;
- visual disturbances such as patterns, flashing lights, or spots in front of the eyes.
These symptoms develop gradually and may last for more than an hour.
Headache phase
During this phase, people usually experience pain that can last from 4 to 72 hours. This does not apply to people with headless migraine, who may experience symptoms such as:
- anxiety or depressed mood;
- dizziness;
- insomnia;
- nasal congestion;
- nausea;
- neck pain and stiffness;
- sensitivity to light, smell and sound;
- vomit.
Migraine symptoms and types
Manifestations of migraine in women can occur episodically, with a frequency of 1-2 times a month. In some cases, there is a clear connection with periods of menstruation.
The disease has characteristic symptoms:
- severe headache lasting from several hours to several days;
- nausea;
- vomit;
- tactile touch intolerance;
- increased pain during mental and physical activity.
The headache is unilateral, less often bilateral. Sometimes it is localized in the eye or temporal region, spreading to the neck area. At the beginning of the attack, the pain is dull, with gradual intensification and pulsation. External irritants (bright lights, loud sounds, strong odors) contribute to increased pain.
In about a third of patients, characteristic warning signs are observed before the onset of an attack:
- anxiety;
- panic attacks;
- depressed mood, its sudden changes;
- decreased performance;
- chills;
- yawn;
- drowsiness and apathy;
- dizziness.
About an hour before the onset of an attack, visual disturbances may occur: flashes of light, double outlines of objects, luminous zigzags, spots or dots. Less commonly, there is a feeling of numbness in the limbs or transient speech disturbances (the so-called migraine aura).
The attack ends with a long, heavy sleep.
The symptoms and causes of migraine in women are individual, appear in various combinations and can differ significantly in patients of different ages.
The most common types of migraines are:
Classic or migraine with aura
The attack is preceded by auditory hallucinations, disturbances of smell and vision.
No aura
The attack occurs without warning, with a painful headache in one part of the head.
With an aura without a headache
There is only an aura and additional symptoms, no headache.
Aphasic
At the peak of the attack, temporary speech disorders are noted.
Ophthalmic
Pregnant women are mainly susceptible due to stress, overexertion, and disruption of their daily routine. A distinctive feature is temporary visual disturbances (flashes, sparks, spots, distortion of the size of objects).
Basilar
Manifests itself in the form of a pronounced aura with hearing loss, dizziness, and fainting. May provoke the development of ischemic stroke.
Cervical migraine
Dysfunction of the arteries located in the cervical spine leads to oxygen starvation of the brain. A characteristic symptom is a dull throbbing pain in the back of the head.
Menstrual
Associated with hormonal fluctuations that occur in the female body during the menstrual cycle. Pain and accompanying symptoms develop 2 days before the onset of menstrual bleeding or within three days after its completion.
What is migraine?
“When I have a migraine attack, I am completely overwhelmed and completely taken out of my daily life for a day or more. Once it starts, the attack keeps growing and I feel so terrible that I have to go to bed. The pain gets stronger and stronger, nausea appears, sometimes I can vomit; Finally, the pain begins to subside. The next day my head is heavy, I feel empty, but still much better than the day before.”
Migraine is a neurological disease. It manifests itself in attacks that can occur with varying frequencies - from 1-2 times a year to several times a month.
The main manifestation of a migraine attack is a headache, which can be very severe. Other common symptoms include nausea and vomiting, and intolerance to light and sound.
If during a headache you feel nauseous, are irritated by light or sound, and the headache interferes with your usual activities, then most likely it is a migraine.
Why does migraine occur?
The cause of migraine lies in the brain. Migraine pain is associated with disturbances in the structures that are responsible for transmitting pain and other sensations. There is a hereditary predisposition to developing migraines: that is, you can inherit it from one of your parents.
Who gets migraines?
Every seventh adult suffers from migraine, so the disease is quite common. Women experience migraines three times more often than men. The disease usually begins in childhood or adolescence. In girls, migraines usually begin during puberty. Since there is a hereditary predisposition to the development of migraine, this disease is passed on from generation to generation.
What are the types of migraines?
The most common type of migraine is migraine without aura (aura will be discussed below). This type of migraine occurs in three quarters of migraine patients; migraine with aura occurs exclusively in only every tenth person; the rest may have attacks of both migraine with aura and migraine without aura. Much less often (more often in older people) attacks of only aura without headache are observed. There are other types of migraines, but they are extremely rare.
How does migraine manifest?
All migraine symptoms occur during an attack, which has four stages of development, although not all of them can be fully represented. Most people with migraines feel well between attacks.
The precursor phase of migraine (prodrome) occurs before all other symptoms of an attack and in no more than half of patients. If you have a prodrome, you may feel irritable, depressed, or tired several hours or even a couple of days before the headache develops. Some, on the contrary, may notice an unusual increase in activity. Some people may have an increased appetite, some people “just know” that they will have an attack.
The aura, if present, is the next phase. Only a third of migraine patients ever report an aura, and it may not occur in every attack. An aura is a reflection of a certain process (transient and harmless to health) occurring in the brain and associated with the mechanism of a migraine attack. It lasts 10-30 minutes, but can be longer. Most often there is a visual aura. You may "see" blind spots, flashes of light, or a multi-colored zigzag line extending from the center of your visual field to the periphery. Less common are sensory symptoms - a tingling sensation or numbness that begins in the fingertips on one side, extends up to the shoulder, and sometimes spreads to the cheek or tongue on the same side. Sensory symptoms are almost always accompanied by visual disturbances. In addition, during the aura there may be difficulty speaking or difficulty finding words.
The headache phase is the most severe for most people, lasting from several hours to 2-3 days. Migraine headaches are usually very severe, most often occurring in one half of the head, but can affect the entire head. Most often, pain occurs in the frontal or temporal region, although it can be localized in any part of the head. This is usually a throbbing or bursting pain that intensifies with movement and physical activity. Nausea and even vomiting often occur, which subjectively relieves the headache. During an attack, light and sounds may be unpleasant; most patients prefer to remain alone in a quiet and darkened room.
The headache phase is followed by a resolution phase. During this period, you may again feel tired, irritable or depressed, and find it difficult to concentrate. These symptoms may persist for up to 24 hours before you feel completely well.
What is the “threshold for the development of a migraine attack”?
A migraine attack is unpredictable and can start at any time. However, some people are more prone to having seizures. The higher your threshold for migraine development, the lower the likelihood of developing an attack; the lower the threshold, the greater this likelihood.
Precipitating factors (triggers) of migraine play a significant role. The trigger can trigger a migraine attack (although it is not known how this occurs). This happens especially quickly if the migraine threshold is low. If your threshold is high, then in order for an attack to develop, two or three triggers must act simultaneously.
Triggers must be distinguished from predisposing factors, which lower the threshold for the development of an attack, while triggers initiate an attack. Predisposing factors include chronic fatigue, anxiety and stress; in women this may include menstruation, pregnancy and menopause.
What are migraine triggers?
Every migraine patient would like to know what can trigger an attack. This is usually difficult or impossible because each patient has different triggers; Even within the same patient, different attacks can be caused by different triggers. Many patients are unable to identify their triggers because they vary widely.
Diet : some foods (and alcohol), but only in some patients; More often, an attack can be caused by skipping meals, inadequate nutrition, caffeine withdrawal, and insufficient water intake.
Sleep: changes in sleep patterns, both sleep deprivation and excess sleep
Other life factors : intense physical activity, long journeys, especially with time zone changes.
External : bright or flickering light, strong odors, changes in weather
Psychological : emotional tension or, oddly enough, relaxation after stress.
Hormonal factors in women : menstruation, hormonal contraceptives and hormone replacement therapy.
One common trigger is hunger or not eating enough. This is especially true for young patients - children suffering from migraines should not skip breakfast! In women, a significant potential trigger is hormonal fluctuations associated with the menstrual cycle.
These and most other triggers represent some kind of stress, which supports the idea that people with migraines generally do not respond well to any changes.
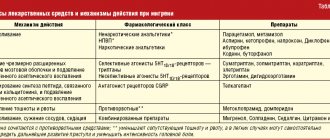
What treatment can be used?
Medicines that are used to relieve an existing migraine attack are called migraine relievers. The right medications can be very effective if taken correctly and in small quantities. These include over-the-counter analgesics, most of which contain aspirin, ibuprofen, or paracetamol; Among them, paracetamol is the least effective. Soluble forms of these drugs, such as effervescent tablets, work faster and better.
If you are very bothered by nausea or vomiting, you can use antiemetics. Some of them actually enhance the effect of analgesics by increasing their absorption in the gastrointestinal tract. If you experience severe nausea or vomiting, you can use these medications in the form of rectal suppositories.
When purchasing the drug, your pharmacist can advise you on which over-the-counter analgesic is best to take. If none of the drugs in this class help you, or you require a dose of the drug that exceeds the recommended dose, you should consult a doctor.
Your doctor may prescribe you one of the specific anti-migraine medications. These medications should be used if analgesics and antiemetics do not relieve your symptoms and quickly return you to daily activities. According to the principle of action, anti-migraine drugs differ from conventional painkillers. They do not affect pain, but the pathological processes occurring in the brain during a migraine attack. These drugs include ergotamine, which is widely used in some countries but not commercially available in others, and a group of newer drugs called triptans. If your doctor has prescribed these drugs to you, then, if necessary, you can combine them with analgesics and antiemetics.
There are several techniques to increase the effectiveness of drug treatment for a migraine attack.
1. Take the drug at the very beginning of the attack...
Always carry at least one dose of the drug recommended by your doctor. Take the drug as soon as you feel the onset of an attack. The sooner you take the medicine, the more effective it will be. During a migraine attack, the gastrointestinal tract slows down, so medications taken in tablet form are absorbed into the bloodstream more slowly than usual. If your condition allows, eat or drink something sweet.
2. ... but not very often
Always strictly follow the instructions for use of the drug. In particular, do not use headache relievers too often, as this may cause you to develop painkiller headaches. This is the so-called headache associated with excessive use of drugs (overuse headache), and there is a separate leaflet dedicated to it, which you can look at if necessary. To prevent you from developing such a headache, under no circumstances use migraine relief products on a regular basis, that is, more than 2-3 times a week.
What to do if this treatment does not help?
If migraine attacks are very frequent or severe and do not respond well to relief medications, then preventative treatment is available. Unlike anti-migraine medications, prophylactic treatment requires medications to be taken every day, as this treatment is aimed at preventing the development of migraine attacks. In other words, preventive treatment can increase the threshold for the occurrence of a migraine attack.
Your doctor will advise you on preventative medications and warn you about possible side effects. Most of them were originally developed to treat other diseases, so you should not be surprised if you are prescribed a drug from the group of antidepressants, antiepileptics, or used to lower blood pressure. You were not prescribed treatment for these indications; these drugs simply also have an anti-migraine effect.
When you are prescribed one or more medications, carefully follow the instructions for use. Studies have shown that the most common reason for the lack of effectiveness of preventive treatment is non-compliance with therapy.
What else can you do to help yourself?
Regular exercise and keeping fit will significantly improve your well-being. It is advisable to avoid predisposing factors and triggers, so it makes sense to know all possible triggers. Try to eliminate at least some of them, even if other triggers are difficult to identify or cannot be avoided.
Keeping a headache diary
Keeping a diary will help you collect important information about your headaches: how often the headache occurs, when it occurs, how long the headache lasts, and what symptoms accompany it. This information is very valuable for making a correct diagnosis, identifying factors that provoke headaches and assessing the effectiveness of treatment.
What to do if you suspect you are pregnant?
You should consult your doctor as some anti-migraine medications are contraindicated during pregnancy.
Do you need additional examinations?
In most cases, diagnosing migraine is not difficult. There are no examination methods to confirm the diagnosis of migraine. Diagnosis is based on your description of the characteristics of the headache and accompanying symptoms, and it is imperative that there are no abnormalities on medical examination. Try to describe your headache to the doctor in as much detail as possible. It is very important to tell your doctor how often and in what quantities you take painkillers or other medications for your headaches.
Brain scans are usually non-diagnostic. If your doctor is not sure of the correct diagnosis, he may prescribe additional examinations to rule out other causes of headaches. As a rule, this is not often necessary. If your doctor has not prescribed additional tests, this means that he is confident in the diagnosis and conducting examinations will not in any way make it easier to prescribe treatment.
Can migraines be cured?
There is no cure for migraines completely. However, for most people with migraines, attacks become less frequent as they age.
The tips and advice contained in this leaflet will help you manage your migraines effectively.
To learn more about the problem of headaches,
visit sites:
www.wha.org , www.headache-society.ru , www.migreni.net
Migraine during pregnancy
Predisposition to the development of migraines during pregnancy is associated with hormonal changes. It occurs both with an aura and without previous signals. Attacks are accompanied by nausea, less often vomiting, sensitivity to external stimuli (light, loud sounds, noises, smells).
Seizures without aura tend to decrease in frequency and duration as labor approaches.
Migraine with aura is characterized by a stable course. Against the background of the disease, blood circulation in the placenta may deteriorate. In rare cases, headaches provoke the development of fetal brain hypoxia. Attacks deplete the expectant mother’s body, which necessitates treatment. When contacting certified medical centers with experienced specialists, treatment is successful.
By the second trimester, positive dynamics are observed - the intensity and duration of paroxysms decreases. By the third trimester, there is an improvement in well-being in 50-80% of cases.
Features of treatment of elderly people with migraine
Somatic and mental illnesses in old age limit the use of some drugs prescribed for migraine. Ergotamine, dihydroergotamine and triptans are contraindicated in the presence of myocardial infarction, stroke, arterial hypertension, note German scientists from the University of Münster. Beta blockers and calcium channel blockers should not be used in patients with cardiac pathology, prostate adenoma, or glaucoma.
Taking medications for migraines should be taken as responsibly as possible.
Diagnosis of migraine
Diagnosis of migraine is based on characteristic symptoms, in the absence of signs of organic damage to the central nervous system. Russian recommendations for migraine in adults do not recommend the use of laboratory and instrumental studies if the disease has a typical course.
Diagnosis of migraine. Photo: US Navy/DVIDS
To exclude physical pathology, a series of tests and studies are performed using all available methods. If you have migraines, testing may be needed to help make a differential diagnosis. Magnetic resonance imaging (MRI) can help rule out inflammatory diseases, tumors, and other organic lesions. For migraine, this study shows no change. Experts recommend keeping a special diary describing each attack of headaches, the reasons that provoke them, the time and duration of the attack. This data can help a specialist systematize symptoms and determine the form of migraine.
Causes of migraine
Currently, there are three theories of the occurrence of attacks. Among them are:
- Disturbances in the functioning of the vascular system.
- Neurological and neurovascular abnormalities.
- Serotonergic theory.
However, none of these theories can fully explain the mechanism of migraine, since each organism is individual and migraine attacks can occur under the influence of certain factors - neurogenic, vascular, biochemical.
Migraine: disease prognosis
What is the prognosis if the diagnosis is migraine? It has been proven that headaches seriously reduce the quality of life and work ability of a person suffering from this common disease. According to statistics, 19% of women and 11% of men complain of characteristic symptoms. The long-term prognosis depends on the individual characteristics of the person. However, there is evidence that the prognosis worsens and the risk of developing chronic migraine increases after each attack. Modern migraine treatments help most people cope with the disease. For most women, symptoms become milder or go away after menopause. In addition, new migraine treatments are constantly being developed. The most promising direction in this area is the use of botulinum toxin preparations for the chronic form of the disease.
Types of Migraine
- Migraine without aura
(people do not have an aura phase). Most forms of migraine occur without an aura. - Migraine with aura
. In this type of migraine, people experience aura symptoms before the headache phase begins. - Basilar migraine
. This form of migraine is rare and can be frightening. Symptoms include double vision or blurred vision, loss of balance, loss of consciousness and difficulty speaking. - Hemiplegic migraine
. During a hemiplegic migraine, a person experiences temporary numbness, weakness, or paralysis on one side of the body. - Retinal migraine
. This rare type of migraine causes weakness in one or more of the muscles that move the eye. This occurs most often in young people. - Vestibular migraine
. People who have vestibular migraine will experience dizziness that lasts from a few minutes to several hours.
Headless migraine - causes
The exact cause of migraines is unknown, but genetic and environmental factors likely play a role. Migraines can develop due to problems with brain activity that affect nerves and blood vessels. Changes in brain chemicals such as serotonin may also be a contributing factor. Several factors can trigger a migraine attack:
- certain products;
- alcohol and caffeine;
- changes in sleep habits;
- changes in weather or atmospheric pressure;
- fluctuations in estrogen in women;
- intense physical activity;
- sensory stimuli such as bright lights, loud sounds, and strong smells;
- use of certain medications such as oral contraceptives and vasodilators.
Treatment and prevention
To eliminate migraines, drug treatment is used, including taking analgesics, anti-inflammatory drugs, as well as drugs that cause a strong vasoconstrictor effect.
Clinical Brain Institute Rating: 2/5 — 10 votes
Share article on social networks
Prevention
Certain lifestyle changes can prevent migraine symptoms. People can try:
- identify triggers (causes) and, if possible, avoid them;
- practice stress-relieving techniques such as meditation, creative therapy, yoga;
- exercise regularly, avoiding intense exercise, which can trigger migraines;
- go to bed and get up at the same time every day;
- regular meals;
- avoid caffeine and limit alcohol consumption;
- maintaining a healthy body weight.
People who suffer from migraines associated with hormonal fluctuations should talk to a doctor who can help reduce the effects of estrogen.
Decapitated migraine - treatment
Treatment can reduce the frequency and severity of migraines. Treatment methods include medications:
Painkillers
: They can stop symptoms as soon as they start.
Preventive drugs
: People can take these medications regularly to reduce their risk of developing migraines. Doctors usually prescribe them for people who have recurrent, persistent, or severe migraines or whose symptoms do not respond to pain medications.
Some people find relief using home remedies that include:
- practicing relaxation techniques such as muscle relaxation, meditation and yoga;
- rash every night;
- resting in a dark, quiet room when symptoms first begin;
- applying an ice pack to the back of the neck;
- light massage of painful areas of the scalp.
Some people, especially those with chronic migraines, may benefit from alternative treatments that include:
Acupuncture
: Acupuncture may reduce the number of migraine attacks, according to a review of scientific papers.
Biofeedback
: An evaluation of biofeedback for migraine found that treatment may improve symptoms such as psychological stress, anxiety, depression, and irritation associated with headache. It may also reduce the duration of migraines.
Massage
: Regular massage can reduce stress and muscle tension, as well as reduce the frequency of migraines.
Primary sources of migraine
Medical studies have not revealed the exact prerequisites for the occurrence of the disease in representatives of both sexes. Genetic predisposition plays a major role in its formation, and individual associated factors play a secondary role.
The occurrence of wave-like attacks of cephalalgia is caused by weather conditions and concomitant pathologies, represented by:
- depressive syndrome, apathy;
- bipolar disorder;
- unreasonable anxiety, worry;
- severe stress or post-traumatic stress conditions.
Exacerbation of the disease is associated with one or more factors:
- stress, tension;
- fasting, improperly selected dietary nutrition;
- excessive fatigue, insufficient sleep;
- strong odors or tobacco smoke;
- changes in weather conditions, including sudden increases in temperature and humidity;
- quality characteristics of indoor air;
- too bright and dim lighting, etc.
The strength and significance of these triggers is not fully understood.