Liquor is the cerebrospinal fluid that fills and washes the anatomical spaces of the brain and spinal cord. It carries the most important functions of protecting these organs from damage and shock, helps maintain the constancy of liquid media, and maintains intracranial pressure. In addition, it is involved in the release of brain metabolites and the transport of nutrients. Analysis of cerebrospinal fluid helps to identify pathologies of the central nervous system, their degree and development, since cerebrospinal fluid immediately reacts by changing parameters to any changes in the brain.
Indications for use
A study of cerebrospinal fluid is carried out when:
- the appearance of a risk of hemorrhage in the brain cavity;
- infections that affect the central nervous system and lead to inflammation of the membranes (meningitis, encephalitis, meningoencephalitis);
- malignant formations in the meninges;
- there is a suspicion of liquorrhea (loss of cerebrospinal fluid), the main cause of which is a violation of the integrity of the hard membranes of the brain.
The above indications are absolute, i.e. requiring mandatory analysis of the cerebrospinal fluid. The study can also be chosen as a diagnostic tool in other situations. Such relative indications may include:
- diseases caused by demyelination, i.e. destruction of the myelin sheath of neurons, in which the conductivity of nerve impulses deteriorates and various abnormalities occur (for example, multiple sclerosis);
- autoimmune diseases;
- blockage of blood vessels by pathogenic organisms (septic embolism);
- the child has a fever of unknown origin;
- systemic lesions of peripheral nerves (polyneuropathy) caused by inflammatory reactions.
In some cases, cerebrospinal fluid analysis is contraindicated, for example, in case of a large tumor, greatly increased cranial pressure, or edema.
The procedure is prescribed with caution in cases of bleeding disorders (due to the risk of bleeding) or thrombocytopenia (a decrease in the number of platelets, accompanied by bleeding).
Multiple Sclerosis Research
Multiple sclerosis is a neurological disease that affects women more often. Multiple sclerosis does not always manifest itself with pronounced symptoms; it is often characterized by nonspecific symptoms - numbness and tingling in the limbs, weakness, and fatigue. With multiple sclerosis, in almost 90% of cases, IgG immunoglobulins are found in the cerebrospinal fluid, which are synthesized in the area of damage to the myelin sheath of the brain. Oligoclonal IgG is found in many other diseases of the nervous system; for the diagnosis of multiple sclerosis, cerebrospinal fluid analysis is performed as an additional test when an MRI study has shown ambiguous results. In multiple sclerosis, serum protein electrophoresis is normal, but oligoclonal antibodies are detected in the cerebrospinal fluid. To differentiate multiple sclerosis from other diseases, certain parameters of the cerebrospinal fluid are studied - the number and composition of cells, protein levels. In multiple sclerosis, the level of protein increase will be moderate. A cerebrospinal fluid analysis for diagnosing multiple sclerosis is prescribed when symptoms of the disease appear:
- increased frequency of urination.
- numbness and tingling in the limbs.
- double vision.
- weakness, fatigue.
- lack of coordination when moving.
Methods for studying cerebrospinal fluid
Cerebrospinal fluid is collected in several test tubes, since the technique for studying cerebrospinal fluid involves conducting tests:
- clinical (external and internal);
- biochemical;
- bacteriological.
External analysis involves studying the type of cerebrospinal fluid, its color, transparency, and the presence of a fibrinous film, which is formed at a high concentration of the fibrinogen protein, which is responsible for blood clotting.
During microscopic (internal) examination, the cellular composition is analyzed. Normally, only monocytes and lymphocytes are present in the cerebrospinal fluid; in pathologies, other cells appear. Their number per unit volume is determined and differentiation is carried out.
Biochemical analysis evaluates the acidity of the cerebrospinal fluid, its relative density, the presence of protein, and the PH level. The concentration of glucose, the amount and proportions of lactate (lactic acid) and pyruvate (pyruvic acid) are also determined. This helps in the diagnosis of CNS infections - viral and bacterial, and may also indicate a cerebrovascular accident.
The bacteriological method of studying cerebrospinal fluid helps to identify pathogens such as pneumococcus, meningococcus, Haemophilus influenzae, and tuberculosis bacilli. It involves taking a smear, isolating and identifying the harmful agent with the determination of antigens.
Decoding the results
A transcript of the cerebrospinal fluid analysis can be viewed online. The interpretation of the cerebrospinal fluid analysis is as follows:
- Change in liquor color:
- the red color of the cerebrospinal fluid is observed when blood enters the cerebrospinal fluid and with subarachnoid hemorrhage;
- xanthochrome color of the cerebrospinal fluid will be with an intraspinal tumor, chronic subdural hematoma, meningeal carcinomatosis;
- a greenish tint of the liquid or yellow is observed with purulent meningitis, a ruptured brain abscess;
- opalescent color of the cerebrospinal fluid is observed with carcinomatosis of the meninges, bacterial meningitis;
- colorless liquid is normal;
- turbidity of the cerebrospinal fluid - the presence of a large number of microorganisms, an increase in the level of leukocytes, erythrocytes, epithelium;
- clear cerebrospinal fluid is normal;
Deciphering the cerebrospinal fluid analysis helps differentiate the disease; additional studies are prescribed for a more accurate diagnosis. Certain changes in some cerebrospinal fluid indicators with normal levels of other indicators may indicate the development of severe damage to the nervous system - multiple sclerosis, Guillain-Barré syndrome and other diseases. Examination of the patient by a neurologist, MRI examination and analysis of cerebrospinal fluid make it possible to begin treatment of multiple sclerosis at an early stage of development.
CSF analysis: explanation (Table 1)
Preparing for the examination
Preparation for cerebrospinal fluid analysis is as follows:
- Blood tests are taken (general, clotting tests).
- At the preliminary consultation, an anamnesis is collected. The patient needs to inform the doctor about past illnesses, the presence of chronic illnesses, and negative reactions to medications.
- It is necessary to donate cerebrospinal fluid on an empty stomach - eating is prohibited 12 hours before the procedure.
Before the examination, taking medications that thin the blood, as well as analgesics and non-steroidal anti-inflammatory drugs is not allowed.
Violation of cerebrospinal fluid. Causes and symptoms
The main disease states associated with CSF include liquorrhea, liquorodynamic imbalance, cerebral hydrocele, and increased intracranial pressure. Their development mechanism differs, as does the symptom complex.
Liquororrhea
It is the most pathogenetically simple disease, because its mechanism is clear: the integrity of the bones of the base of the skull or meninges is disrupted, which provokes the release of the spinal substance.
Depending on the symptoms and visual manifestations, liquorrhea is called:
- Hidden - liquor flows through the nasal passages, which is not visually noticeable due to aspiration or accidental ingestion.
- Obvious - a clear liquid or mixed with ichor is intensely released from the ears, fracture sites, which is noticeable by the leakage of the bandage headband.
Also distinguished:
- The primary nature of the disease - the discharge manifests itself immediately after injury, after surgery.
- Secondary, or cerebrospinal fluid fistulas - leakage is observed in the later stages of severe complications of infectious diseases.
If the primary pathology is not treated for a long period of time, and then inflammation (meningitis or encephalitis) develops, then this is fraught with the development of a fistula.
Common causes of CSF leak:
- severe bruises with traumatic brain injury;
- injuries and serious injuries of the spine;
- complicated hydrocephalus;
- hernial neoplasms and tumors in dangerous proximity or directly in the brain tissue;
- inaccuracy of medical procedures - washing or draining the ENT profile;
- weakness of the sutures of the dura mater after neurosurgical operations;
- Spontaneous liquorrhea is very rare.
Liquorodynamic disorders
CSF dynamics are disrupted if there is difficulty or improper circulation of cerebrospinal fluid. The course of the disease can be hypertensive (associated with high blood pressure) or hypotensive (on the contrary, with low blood pressure).
The hypertensive form occurs when:
- excessive secretion - due to the strong excitability of the choroid plexuses, which are responsible for the production of CSF;
- insufficient absorption and excretion.
Liquor is produced in large quantities or is simply not absorbed, which provokes the following symptoms:
- severe headaches, especially intense in the morning;
- nausea, frequent gagging, periodic vomiting;
- dizzy;
- slow heartbeat – bradycardia;
- sometimes nystagmus - frequent involuntary eye movements, “trembling” of the pupils;
- symptoms characteristic of meningitis.
The hypotensive form occurs less frequently, with hypofunction or weak activity of the choroid plexuses, the consequence is reduced production of the cerebrospinal fluid substance. Symptoms:
- severe headache in the occipital and parietal regions;
- discomfort, increased pain during sudden movements, excessive physical activity;
- hypotension.
In addition to the listed reasons for the appearance of an imbalance in liquor dynamics, experts also identify inflammatory diseases of the central nervous system, parasitic invasion of the central nervous system, spinal injuries/wounds, as well as congenital genetic characteristics.
Impaired cerebrospinal fluid outflow and resorption
from the brain may be disrupted - due to this, deviations develop that manifest themselves differently in adults and children.
An adult will respond to a deviation by increasing intracranial pressure due to a strong, “overgrown” cranium. The bones of the child’s skull are immature and have not yet fused together, so excessive accumulation of spinal substance provokes hydrocephalus (dropsy) and other unpleasant manifestations.
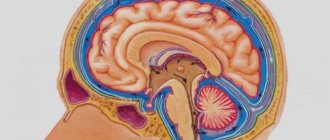
CSF accumulation in the brain – increased ICP in adults
The cranium contains not only brain tissue and a great many neurons - a significant part of the volume is occupied by CSF. Its larger share is located in the ventricles, and the smaller one washes the GM and moves between its arachnoid and soft membranes.
Intracranial pressure directly depends on the volume of the skull and the amount of fluid circulating in it. Whether the production of a substance increases or its resorption decreases, the body immediately responds to this by increasing ICP.
This indicator reflects how much the pressure inside the skull exceeds atmospheric pressure - the norm is a value from 3 to 15 mm of mercury. Minor fluctuations lead to a deterioration in well-being, but an increase in ICP to 30 mm Hg. Art. already threatens to be fatal.
Manifestations of increased ICP:
- constantly sleepy, low performance;
- severe headaches;
- deterioration of visual acuity;
- forgetfulness, absent-mindedness, low concentration;
- “jumps” in pressure are noticeable - hypertension is regularly replaced by hypotension;
- poor appetite, nausea, vomiting;
- emotional instability: mood swings, depression, apathy, severe irritability;
- spinal pain;
- chills;
- increased sweating;
- failures of respiratory activity, shortness of breath;
- skin is more sensitive;
- muscle paresis.
The presence of 2-3 symptoms is not a reason to suspect increased ICP, but an almost complete complex is a good reason to consult a specialist.
The clearest sign of the disease is a girdling headache that is not expressed in any particular area. Coughing, sneezing and sudden movements only provoke increased pain, which is not relieved even by analgesics.
The second important sign of increased ICP is vision problems. The patient suffers from double vision (diplopia), notices deterioration of vision in the dark and in bright light, sees as if in a fog and suffers from attacks of blindness.
Pressure can increase in a healthy body, but it immediately returns to normal - for example, during physical and emotional stress, stress, coughing or sneezing.
Accumulation of cerebrospinal fluid in the brain - pediatric hydrops GM
Young children cannot report how they are feeling, so parents must be able to identify a violation of the cerebrospinal fluid outflow by the external signs and behavior of the baby. These include:
- noticeable vascular network on the skin of the forehead and back of the head;
- restlessness at night, poor sleep;
- frequent crying;
- vomit;
- protrusion of the fontanel, its pulsation;
- convulsions;
- increase in head size;
- uneven muscle tone - some are tense and some are relaxed.
The most serious sign of increased ICP in a child is hydrocephalus, which occurs with a frequency of up to one case in a couple of thousand newborns. Male babies suffer from hydrocele more often, and the defect itself is usually diagnosed by doctors during the first 3 months of life.
“Cerebral hydrocephalus”, as an independent disease, should not be confused with the diagnosis of “hypertensive-hydrocephalic syndrome”. It reflects that the newborn has a slightly increased ICP, but this does not require therapy or surgery, since it resolves itself.
The childhood form of the disease can be congenital or acquired, depending on the cause of development, of which, according to medical experts, there can be up to 170. The congenital disease is provoked by:
- injury to the child during childbirth;
- hypoxia during childbirth (insufficient oxygen supply);
- genetic failures;
- infectious diseases transmitted by the fetus while in the womb (cytomegalopathy, acute respiratory viral infections, mycoplasma and toxoplasma infections, syphilis, rubella, mumps and herpesvirus).
Genetic abnormalities causing the congenital form:
- underdeveloped cerebrospinal fluid ducts;
- Chiari syndrome - the child’s skull is larger in volume than his brain;
- narrowed liquor duct;
- other chromosomal pathologies.
The acquired form occurs as a result of toxic poisoning, the development of tumors, cerebral hemorrhages, and infectious diseases outside the mother's womb - these include otitis media, meningitis and encephalitis.
Speaking about hydrocephalus in newborns, it is worth considering that normally the head circumference of babies increases quite quickly (one and a half centimeters per month), but if the growth exceeds the indicators, then this is a good reason to examine the child.
The baby’s skull is soft, not yet ossified, and excess cerebrospinal fluid slows down the overgrowth of the fontanel, “pushes” the bones apart and prevents the normal development of the skull - because of this, the head grows disproportionately. Accumulating in the subarachnoid space , which separates the meninges, the cerebrospinal fluid compresses some parts of the brain. Despite the pliability of children's cranial bones, this manifestation of the disease is dangerous and requires immediate treatment. An increase in head size is not the only sign of obstructed liquor outflow in children. Characteristic is:
- the specific sound of a “broken pot”, heard when lightly tapping the skull;
- difficulty raising and holding the head in one position;
- trembling of the chin, hands.
It is important to pay attention to the baby’s eyes, because some signs are indicative:
- involuntary, chaotic eye movements;
- occasional eye rolling;
- eyes “squint”;
- “setting sun” syndrome - when blinking, a thin white stripe is noticeable between the pupil and the upper eyelid.
Hydrocephalus up to 2 years of age is manifested by this symptom complex, and later it is combined with vomiting, nausea, problems with coordination, irritability, diplopia or even blindness.
Sometimes hydrocephalic syndrome develops in adults as a consequence of previous infections, but this is a rare occurrence.
How to improve the outflow of cerebrospinal fluid
The pathology of liquor outflow in a baby is usually learned from a neurologist, whose examination takes place in the first month after birth. An initial examination and identification of signs requires medical correction, since this disease will interfere with the normal development of the child.
If the condition of a small patient is complex, then specialists use surgical intervention to create “bypass paths” for the CSF and eliminate the poor outflow artificially. If the situation does not threaten the baby’s life, treatment can also take place at home with drug therapy. In order to prescribe the optimal medications for a child, it is necessary to understand what can interfere with the outflow of cerebrospinal fluid in hydrocephalus . The cause, origin and complications will all play a role in the selection of treatment.
Pharmacological correction of outflow disorders in children includes:
- drugs that improve and stimulate blood flow (Actovegin, Pantogam, Cinnarizine);
- medications that help remove excess fluid (Triampur or Diakarb);
- neuroprotective drugs (Ceraxon).
Analysis process
Typically, cerebrospinal fluid is obtained using a lumbar puncture to obtain a sample. Sometimes it is necessary to do a ventricular (ventricular) or suboccipital (occipital) puncture, but this is not common. The price of the procedure varies depending on the type of fluid taken; the cost also varies depending on the location and complexity of the study.
A sequential description of the procedure, which lasts on average 40-50 minutes, is as follows:
- The patient takes a horizontal position and pulls his legs to his stomach and his head to his chest (during lumbar puncture). In other types - lying or sitting.
- The desired area is treated with iodine and alcohol.
- For pain relief, novocaine is injected into the puncture area.
- The needle passes between the 3rd and 4th or 5th and 6th vertebrae (for lumbar puncture), between the temporal, parietal and frontal bones (for ventricular puncture), between the second cervical vertebra and the occipital bone (for occipital puncture).
- CSF is collected. By the way the liquid flows out, deviations can be judged. Normally, it is released in drops, but with an increase in intracranial pressure it runs rapidly. A pressure gauge is used to determine pressure.
- The needle is removed and the puncture area is covered with a sterile napkin.
- The patient is prescribed bed rest for a day.
The resulting liquor must be immediately delivered to the laboratory.
Research for meningitis
If cerebrospinal fluid examination does not reveal inflammatory changes, the diagnosis of meningitis is excluded. An important component of the analysis is pleocytosis. Turbid cerebrospinal fluid with a discolored liquid (from milky to greenish) indicates the development of purulent meningitis. Neutrophils predominate in the fluid, which suggests the severity of the inflammatory process. Increased protein, decreased glucose levels. With a decrease in the number of neutrophils and an increase in lymphocytes, and an increase in glucose levels, we can talk about a favorable outcome of the disease.
When testing for tuberculous meningitis, a bacterioscopy test may be negative. This form of meningitis is indicated by the formation of sediment in the cerebrospinal fluid when it settles. In most cases, Mycobacterium tuberculosis is found in sediment, which is a cobweb-like delicate mesh. The cerebrospinal fluid in tuberculous meningitis has no color, is transparent, there is a high level of lymphocytes in pleocytosis, in some cases the level of neutrophils and lymphocytes increases. Poor prognosis with an increase in the number of macrophages and monocytes. With tuberculous meningitis, the protein level is increased, the glucose level is decreased, and in some patients the chloride level decreases.
Meningococcal meningitis is characterized by increased intracranial pressure; when examining the cerebrospinal fluid, mild neutrophilic cytosis is detected, then changes occur as in purulent meningitis.
Serous meningitis is characterized by clear cerebrospinal fluid, slight pleocytosis with an increase in the level of lymphocytes. The protein level is within normal limits or slightly increases; in some patients, the protein level may fall due to overproduction of cerebrospinal fluid. If in the initial stage of the disease there is pleocytosis with the growth of neutrophils, then the prognosis of the disease is considered unfavorable and the course of the disease is severe.
Treatment of spinal fluid disorders
Children's diseases of cerebrospinal fluid dynamics are most often corrected by pharmacotherapy, but adults need to be prescribed physiological procedures:
- A course of electrophoresis with aminophylline (ten visits) - drug “recharge” will activate the delivery of oxygen to brain tissue suffering from hypoxia with increased ICP. The condition of the vessels returns to normal, which will ensure normal resorption.
- 15 sessions of massage of the collar area - the procedure is simple, so over time the patient can carry out a similar manipulation himself. With its help, muscle hypertonicity is reduced, spasm is relieved and outflow is improved.
- Magnetic effect on the collar area - reduction of swelling and vascular spasm, improvement of innervation.
- Therapeutic swimming or supportive exercise. charger.