Definition of frontal lobe epilepsy
Frontal epilepsy is one of the forms of epilepsy, accompanied by seizures, the focus of which is located in the frontal regions of the brain. Frontal lobe epilepsy is the second most common and accounts for approximately 30% of other forms.
Frontal lobe epilepsy can develop at any age. The likelihood of developing this form of epilepsy is the same in men and women.
Features of a frontal epileptic seizure:
- A motor phenomenon that is accompanied by gestural automatisms at the beginning of an attack. There are tonic, clonic and postural;
- The attack lasts several seconds;
- Rapid secondary generalization, observed more often during temporal lobe seizures;
- Minimal or complete absence of postictal confusion;
- Attacks occur frequently, mostly occurring at night. Consciousness may be preserved or partially impaired. The clinical pattern of a seizure depends on the location of the lesion.
Causes of development of temporal lobe epilepsy
There are two groups of causes of temporal lobe epilepsy (TE):
1. Perinatal (intrauterine development and childbirth):
- intrauterine infection and polyhydramnios,
- fetal hypoxia,
- premature birth,
- cortical dysplasia
- suffocation during childbirth,
- birth injury.
2. Postnatal (from the moment of birth and throughout life):
- various brain diseases (infections, inflammations, cysts, tumors),
- traumatic brain injuries (specifically, the temporal lobe),
- alcohol addiction (there is even a concept of alcoholic epilepsy),
- vitamin deficiency, hypoglycemia, circulatory disorders, intoxication, etc.
In almost all cases of temporal lobe epilepsy, a disorder in the structure of the hippocampus is found - hippocampal sclerosis. There is an opinion that epilepsy is inherited, but this does not correspond to reality. The disease itself is not hereditary, however, the specific reaction of neurons to stimuli is inherited, which can trigger the onset of the disease.
Diagnosis of frontal lobe epilepsy
Diagnosis of this type of epilepsy is carried out using MRI. Magnetic resonance imaging reveals the focus of pathology in 60% of cases. Functional neuroimaging methods are also used to help achieve focus localization. Interictal and ictal EEG results will usually be normal.
In most cases, the prognosis for the frequency of attacks during treatment is not encouraging.
The probability of erroneous differential diagnosis is very high - hypermotor seizures are regarded as psychogenic seizures, familial paroxysmal dystonic choreoathetosis, paroxysmal kinesiogenic choreoathetosis, episodic ataxia. Due to similar clinical manifestations and EEG characteristics, symptomatic frontal absence seizures are mistakenly classified as typical absence seizures.
Causes of epilepsy at night
Why the symptoms of the disease appear during the dark period of the day still remains an open question. But based on practical observations, psychiatrists at our mental health center have identified a number of factors that provoke exacerbation.
These include:
- Insufficient duration of rest, chronic lack of sleep.
- A state of prolonged stress.
- Abuse of drinks containing alcohol, smoking.
- Taking psychoactive substances, including medications.
- Head injuries, previous surgical interventions.
- The presence of epilepsy in close relatives.
In a child, an attack can be triggered by:
- Overexcitement before falling asleep.
- Loud noise at night.
- Lack of fresh air.
- High or low temperature in the sleeping area.
- Violent awakening.
Similar causes leading to a seizure are also identified in adolescents. To these is added watching a movie in the evening that causes a mental reaction and excitement.
Causes and symptoms of frontal lobe epilepsy
The clinical symptoms of frontal lobe epilepsy are determined by the zone of irritation, on the basis of which the following forms are distinguished:
- Motor form, which is accompanied by convulsions in the half of the body that is opposite to the lesion;
- Dorsolateral paroxysms, which are expressed by a sharp unnatural turn of the head and eyes in the direction that is also opposite to the focus of the pathology;
- Orbitofrontal paroxysms, manifesting as cardiovascular, respiratory and epigastric attacks. In this case, it is possible to record pharyngeal-oral automatisms, which are accompanied by copious secretion of saliva;
- Frontopolar seizures associated with mental dysfunction;
- Cingular seizures that disrupt a person’s behavior and expression of emotions;
- Seizures arising from the supplementary motor area of the brain. Paroxysms from different parts of the frontal lobe of the brain can spread to the supplementary motor area. In this case, the patient suffers from nocturnal simple partial seizures. Seizures alternate with archaic movements and hemiconvulsions. Often an epileptic seizure is accompanied by aphasia. Aphasia is a disorder of the speech apparatus, and occurs due to damage to certain areas of the cerebral cortex. Accompanied by strange sensations in the torso, arms and legs. In addition, tonic convulsions appear alternately in one half or throughout the entire body.
- “Inhibitory” seizures and paroxysmal hemiparesis are rare phenomena accompanied by paroxysms of archaic movements, which often occur at night. These seizures can happen up to 10 times a night and repeat every night.
Symptoms of temporal lobe epilepsy
The first signs of temporal lobe epilepsy usually appear from six months of age to 6-7 years. Sometimes the manifestations of the disease are so invisible that parents do not react to them, considering them to be a common ailment. This condition can persist throughout life, or it can progress and manifest itself rapidly during puberty.
Most often, seizures in VE are partial (local), but in severe cases, pathological activity can spread from one part of the body to surrounding parts, and ultimately completely take over the body, causing a so-called secondary generalized epileptic seizure.
The onset of a seizure in temporal lobe epilepsy is usually expressed by:
- from the motor side: involuntary movements (turning the palm, eyes, head in a certain direction), inappropriate actions (the patient begins to move things from place to place, change clothes, etc.);
- from the side of sensations: hallucinations (visual, auditory, olfactory, gustatory) are of the “seemed” nature, which is how they differ from true hallucinations;
- vestibular disorders: dizziness, loss of balance;
- mental manifestations: anxiety attacks, panic attacks, feelings of derealization and depersonalization;
- often the attack is accompanied by vague pain in the heart or gastrointestinal distress (stomach pain, intestinal weakness).
These symptoms can be considered an aura before a complex partial attack, which is accompanied by unconscious compulsive actions: uncontrolled swallowing, sucking reflex, chewing movements of the jaw, grimacing, blinking, looking around, rubbing hands, stamping. Sometimes an epileptic attack, on the contrary, can be expressed in the patient freezing in an unnatural position. In some cases, loss of consciousness occurs without convulsions. During an attack, the patient usually does not react to surrounding stimuli, and after the attack does not remember what he did during it.
Preventing seizures
Epileptic seizures that occur at night are easier for patients to tolerate. The effectiveness of drug therapy also gives more significant results. After treatment is completed at our mental health center, we offer patients recommendations to reduce the likelihood of symptoms returning.
Clients should adhere to the following rules:
Normalize sleep and rest patterns. Sleep at least 8 hours a day, go to bed and get up at a certain time.- Provide the opportunity to rest for at least 1 hour during the day.
- In the evening, do not watch TV for a long time, especially with programs and films that carry negative information.
- Do not play computer games or talk on the phone for a long time.
- Before going to bed, calm down and think about something pleasant.
- Sleep in a ventilated room with the curtains closed.
- Avoid drinking alcohol and smoking completely.
- Do moderate intensity physical activity. Strictly avoid overloading.
- If you have the slightest suspicion of resumption of epileptic seizures, consult a doctor immediately.
Classification of focal epilepsy
So, focal epilepsy and what is it in adults and children, how is it classified? There are many parameters for defining a term in medicine. From a neurological perspective, there are three main forms of PE:
- Symptomatic. It is diagnosed if the cause of damage to a specific sector of the medulla can be clearly identified. As a rule, instrumental diagnostics are used for this.
- Cryptogenic. It is characterized by the inability to make an accurate diagnosis depending on the location of the lesion. The likelihood that the disease is a secondary manifestation, and the frontal lobe and other parts are not damaged, is high.
- Ideopathic. Regardless of any cause, the symptoms are idiopathic in nature.
TREATMENT OF IDIOPATHIC GENERALIZED EPILEPSY
Treatment of idiopathic generalized epilepsies is complex and often requires lifelong treatment.
Sodium valproate is one of the most effective drugs in the treatment of all types of IGE attacks. The effectiveness of monotherapy reaches 75%. Sodium valproate prevents the development of absence seizures and is effective in myoclonic absence seizures, and also eliminates photosensitivity. However, its pharmacokinetic properties and spectrum of side effects may limit its use. Clonazepam is also effective against all types of attacks in IGE, but its use is limited by side effects and relatively rapid development of addiction. Lamotrigine is effective in controlling absence seizures and GTCS, but its effect on myoclonus is unpredictable. Ethosuximide is effective for typical absence seizures but cannot prevent generalized tonic-clonic seizures or myoclonus. Therefore, ethosuximide may be the first choice drug for DAE, but not for JAE, where the risk of generalized tonic-clonic seizures is high. Of the new generation drugs, topiramate and levetiracetam have demonstrated their effectiveness in treating IGE. High-quality clinical studies regarding treatment options for IGE syndromes in children and adolescents are still lacking. Based on the data available today, the sequence of anticonvulsants for IGE appears as follows (Table 4.)
Table 4
Drugs of choice for the treatment of idiopathic generalized epilepsies in children and adolescents
Absence seizures:
- Valproate and/or ethosuximide or lamotrigine
- Topiramate or clonazepam or levetiracetam
- Polytherapy
Myoclonus:
- Valproate or levetiracetam
- Topiramate or clonazepam
- Piracetam or polytherapy
GTKP:
- Valproate or topiramate or lamotrigine
- Barbiturates or clonazepam or carbamazepine
- Polytherapy
The use of carbamazepine, phenytoin, vigabatrin, tiagabine, gabapentin and pregabalin, which can increase the frequency of absence seizures and myoclonus, contribute to the development of absence seizure status, is contraindicated.
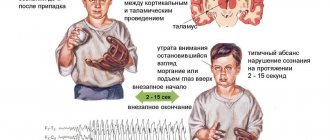
Rice. 1. The characteristic EEG pattern of a typical absence seizure is generalized bilaterally synchronous rhythmic peak-wave complexes with a frequency of 3 Hz.
Rice. 2. EEG pattern of atypical absence - generalized bilateral synchronous arrhythmic peak-wave complexes with a frequency of less than 3 Hz.
Rice. 3. Bioccipital delta activity in a patient with childhood absence epilepsy.
Treatment
After consultation and examination, psychiatrists at the Leto clinic will offer you the most suitable treatment option. In uncomplicated cases, you can get by with an outpatient selection of the necessary medications to take at home. In more complex situations, hospitalization cannot be avoided.
We offer you comfortable conditions in our hospital rooms. 24-hour supervision allows you to use all treatment procedures with maximum efficiency.
The treatment plan is selected individually and includes:
Prescribing drugs to relieve pain from attacks in the presence of pain using anticonvulsants or painkillers, as well as taking prunes, which contain a lot of calcium. This element is able to reduce the number of convulsive episodes and has the ability to relieve pain.- Prevention and reduction of the frequency of new paroxysms. The goal is achieved by consuming foods that are part of the ketogenic diet.
- Reducing the duration of residual seizures.
- Gradually reduce the dose of medication after the seizures disappear.
Pharmaceutical drugs are selected in such a way as to minimize the possible side effects of anticonvulsants.
Nocturnal sleep epilepsy must be eliminated by prescribing special anticonvulsants. The selection of anticonvulsants begins with the selection of one name. If necessary, two or more pharmaceuticals are introduced into the treatment regimen.
Most often used:
- Carbamazepine.
- Clonazepam.
- Phenytoin.
- Lamotrigine.
If the selection and combination of pharmacotherapy does not give the expected result, then electrical stimulation of the vagus nerve is prescribed.
As an additional treatment option, the Vojta physiotherapeutic method is used, based on the normalization of nerve connections. This technique can be taught to the patient’s relatives, and they will be able to use it at home independently after discharge from the hospital.
Diagnostics
If your loved ones, children, or acquaintances have suspicious symptoms, we suggest undergoing a diagnostic examination at our Leto clinic. Experienced specialists will assess the patient’s condition and accurately establish a diagnosis so that the subsequent selection of treatment will lead to a positive result.
To make an appointment with a doctor, make a preliminary call at the phone number listed on the website. The receptionist on duty will register the client at a suitable time.
The initial consultation includes:
- Survey and find out the essence of the problem that has arisen.
- Examination with assessment of all data on the condition, including neurological status, identifying signs characteristic of epilepsy.
- Clarification of all the details of existing epileptic attacks: frequency of occurrence, duration, other features.
After the medical examination you will need to undergo:
Magnetic resonance imaging (MRI). It will allow us to identify oncological processes, structural features of the brain, the presence of consequences of hemorrhages, vascular anomalies, and other changes that lead to problems.- Electroencephalography (EEG). Removal of biopotentials makes it possible to accurately identify the paroxysmal predisposition of the nervous system and establish the variant of the disease.
- Positron emission tomography (PET). The technique is prescribed to patients with metabolic and metabolic disorders in the body to assess metabolic processes in brain tissue, to confirm the found formations in controversial cases.
If the patient has concomitant ailments, the clinic can provide consultations with other specialists.
All procedures are necessary to clarify and confirm the diagnosis.
Treatment of epilepsy in children
The first step to overcoming the disease is diagnosis in the office of a neurologist. If one of the presented signs begins to appear, you should immediately go to a good clinic. An experienced doctor will identify the problem (probably requiring tests to make an accurate diagnosis), and select a strategy to solve it.
Effective medications are used to treat epilepsy. Every third child recovers as a result of drug treatment alone. The use of hardware technologies makes it possible to permanently cure more than 75% of babies.
SELECTED FORMS OF IDIOPATHIC GENERALIZED EPILEPSY
Absence forms
Among absence-dominated epilepsies, the most common form is childhood absence epilepsy (CAE) .
The onset of the disease is from 2 to 8 years of age. The frequency of childhood absence epilepsy among children from 1 to 15 years of age is 6.3-8 per 100,000. Girls are more often affected - they make up 76% of patients.
The main clinical manifestation is typical absence seizures (simple and complex), which are accompanied by a sudden and profound disturbance of consciousness, cessation of gaze and interruption of vigorous activity. 35% of patients with childhood absence epilepsy have simple absence seizures, 43% have complex absence seizures, and 22% of cases have both.
Absence seizures in this form of epilepsy are characterized by a profound impairment of consciousness and complete amnesia of the attack; freezing of the gaze, interruption of speech and other activities. The duration of the attack is on average 6-15 seconds. The frequency of attacks is usually high - up to several dozen attacks per day. Absence seizures occur mainly during the daytime.
In most patients with childhood absence epilepsy, typical absence seizures are the first symptom. In 2/3 of cases, various automatisms occur.
40% of patients with childhood absence epilepsy have generalized tonic-clonic seizures.
In childhood absence epilepsy, generalized tonic-clonic seizures usually occur at the age of 10-13 years, more often upon awakening.
The presence of incomplete loss of consciousness, severe and rhythmic myoclonus, or generalized seizures or myoclonus before the onset of absence seizures makes the diagnosis of childhood absence epilepsy unlikely.
There are so-called “strict” criteria for DAE (Table 4), if met, we can talk about a 100% probability of recovery.
Table 4
Strict criteria for childhood absence epilepsy (Loiseau and Panayiotopoulos, 2005)
Inclusion criteria:
- The age of debut is from 4 to 10 years with a peak at 5-7 years.
- Normal neurological status and mental development.
- Short (4-20 seconds) and frequent (dozens per day) absence seizures with sudden and profound loss of consciousness.
- Ictal discharges are represented by peak- or beep-wave complexes (single complexes may contain 3 peaks in a row). These discharges are rhythmic, their frequency is 3 Hz and gradually slows down towards the end of the attack.
Exclusion criteria:
- Other types of seizures (GTC, myoclonus) before the onset of absence seizures
- Myoclonus of the eyelids, perioral myoclonus, rhythmic shaking of the hands and single or arrhythmic shaking of the head, torso, and limbs
- Incomplete loss or retention of consciousness during EEG discharges
- Short (less than 4 sec.), fragmented ictal discharges, polyps (more than 3 in one complex)
- Photosensitivity and other clinically obvious types of sensitivity.
The main provoking factors are emotional, intellectual and metabolic factors (hypoglycemia, hypocapnia). The absence of absence seizures during hyperventilation in patients who have not received anticonvulsants should raise doubts about the diagnosis of childhood absence epilepsy. Photosensitivity occurs in 10% of cases.
Bioelectrical activity of the brain during the interictal period can be completely normal, but discharges of generalized bilateral synchronous peak-wave complexes with a frequency of 3 Hz are usually recorded of varying durations against a background of normal basic rhythms. The ictal pattern is characterized by longer discharges of peak-wave complexes. Typically, clinical manifestations appear when the discharge lasts more than 5 seconds.
In 15-20% of patients with DAE, after closing the eyes, rhythmic delta activity of 2.5-3.5 Hz can be recorded in the occipital regions of the brain, which appears in the form of periods lasting from several seconds to a minute (Fig. 3.). Bioccipital delta activity is most common in children aged 5 to 8 years. Transient asymmetry of this activity occurs in approximately a quarter of cases. This delta activity can be interspersed with individual synchronous peaks and spread to adjacent areas of the cortex.
The prognosis for DAE is favorable - recovery occurs in almost 100% of cases. The prognosis is worsened by pharmacoresistance of seizures, photosensitivity and the presence of more than 10 generalized convulsive seizures.
The adolescent variant of IGE with absence seizure dominance is represented by juvenile absence epilepsy (JAE ). The disease debuts between the ages of 7 and 12 years. The proportion of juvenile absence epilepsy (JAE) is about 10% among all age-dependent absence epilepsies.
The main clinical manifestations of juvenile absence epilepsy are typical absence seizures. Simple absence seizures predominate - 66%. The frequency of absence seizures in JAE is low - several attacks per day or less. In comparison with DAE, absence seizures in JAE are characterized by a lesser depth of disturbance of consciousness, a longer duration and a more frequent myoclonic component in the structure of the attack. A third of patients experience automatisms that occur 6-10 seconds after the onset of an attack. Up to 20% of patients experience absence status episodes.
80% of patients with JAE have generalized tonic-clonic seizures. The most typical occurrence of GTCS is upon awakening. This type of attack usually joins absence seizures at the age of 14-15 years.
The most important precipitating factors in juvenile absence epilepsy are hyperventilation and sleep deprivation. Photosensitivity is relatively rare.
Neurological and mental status, as well as neuroimaging data, are normal in most patients.
Interictal EEG contains short discharges of generalized bilaterally synchronous peak-wave complexes with a frequency of 3.5-4.5 Hz. In some patients, these complexes may be localized only over the posterior parts of the brain. Ictal patterns differ little from those in childhood absence epilepsy.
Factors that worsen the prognosis are the clonic component of absence seizures, absence seizure status, nocturnal GTCS, and asymmetry of epileptic discharges on the EEG.
In young children, epilepsy with typical absence seizures is rare, but nevertheless, there is a separate IGE syndrome - early age absence epilepsy (AERE) . The age of manifestation of the disease is the first 4 years of life, boys are more often affected. The prevalence is not known due to the lack of registration as an independent nosological unit. The main clinical symptom is typical absence seizures (simple and complex), which are characterized by a short duration and low frequency of occurrence.
In 2/3 of patients, absence seizures are combined with generalized tonic-clonic seizures, which are often the first symptom of the disease.
In 40% of cases, these attacks may be accompanied by myoclonic or myoclonic-astatic paroxysms. A moderate delay in neuropsychic development is often observed.
Basic bioelectrical activity is usually within normal limits or there is a slight slowdown in the background rhythm. The most typical interictal and ictal EEG pattern is generalized bilaterally synchronous peak-wave complexes with a frequency of 2-3 Hz. There may be polypeak-wave complexes and focal peaks. The presence of myoclonic-astatic seizures and the low frequency of discharges on the EEG bring AERV closer to epileptic encephalopathies of early age.
Among the IGE syndromes, the most “noticeable” seizures are characterized by the so-called epilepsy with generalized convulsive seizures of awakening or epilepsy with isolated generalized convulsive seizures.
The main clinical manifestation of this form of epilepsy is generalized tonic-clonic seizures, which in most cases (about 90%) occur in the first 2 hours after waking up.
The age of onset of this form of IGE is more variable, in comparison with the rather narrow age limits of onset in age-dependent epilepsies with absences. In 66% of cases, epilepsy with grandmal seizures manifests itself between the ages of 9 and 24 years.
In some patients, GTCS are not the only type of seizure - myoclonic attacks and absence seizures are also possible.
Seizures in this form of epilepsy occur suddenly, without an aura. They are often accompanied by traumatic falls. The attacks may be precipitated by episodes of relaxation and rest. In some cases, HCTP begins with a series of myoclonus, which usually involves the arms and face.
Up to a quarter of cases are accompanied by a focal component, which is usually expressed in a turning of the head and eyes to the side, which occurs during the attack.
Attacks are triggered by sleep deprivation, alcohol, and stress. These factors often occur together. In women, attacks can be associated with the menstrual cycle and usually occur in the premenstrual period. Photosensitivity occurs in 18% of patients.
Neurological status and neuroimaging data are usually within normal limits or there are minor nonspecific changes.
Electrographic changes in the interictal period are variable and are represented by generalized synchronous peak-wave complexes or, less commonly, polypeak-wave complexes. Often, in the interictal period, routine EEG does not reveal pathology.
The prognosis for epilepsy with isolated GTCS is relatively favorable - in most cases, good seizure control is possible with the help of regimen measures and monotherapy with anticonvulsants. However, this condition can be lifelong and relapses occur in more than 80% of patients when therapy is discontinued.
Among IGE syndromes, juvenile myoclonic epilepsy (JME) , since it is one of the most common forms of epilepsy in young people and adults. The incidence of JME is 3% among childhood epilepsies and 11% among adults with epilepsy.
Females get sick 2-3 times more often than males. Family history of epilepsy - 17-49%.
Onset most often occurs between the ages of 12 and 18 years, but onset is also possible in the first decade of life.
The clinical picture is represented by a combination of myoclonus, absences and generalized tonic-clonic seizures: myoclonus - 100%, GTCS -80% and absences - in 25%. As the only symptom of the disease, myoclonus is rare - 5-17% of cases.
Myoclonus, as a rule, has a jerk-like character, is localized mainly in the proximal muscle groups of the upper extremities (in the area of the shoulders, arm extensors), usually symmetrical, bilateral, and has varying degrees of severity. In some patients they are so weakly expressed that they are felt only by the patient in the form of a sensation reminiscent of a weak electric shock.
In other cases, myoclonus is so amplitude that it leads to throwing objects and even falls. Falls may also occur if myoclonus is localized in the legs.
Involvement of only the arms in myoclonic seizures is the most common variant of JME and accounts for about half of cases. Combined myoclonus of the arms and legs occurs in 40% of patients, and the muscles of the neck and face – in 10%.
The frequency of myoclonus varies from single to multiple.
The distribution of myoclonus throughout the day usually tends to occur most often in the morning, shortly after waking up.
Consciousness during myoclonic attacks is usually not impaired, although in some cases it may be slightly suppressed during long-term series.
Absence seizures in JME are observed in a relatively small number of patients - from 10% to 30% of cases. Absence seizures can precede myoclonus and occur long before their onset, develop approximately simultaneously with myoclonus, or several years after the development of myoclonus. They usually appear before myoclonus, which occurs between 1 and 9 years of age. 3-8% of children with absence seizures are subsequently diagnosed with JME.
Generalized tonic-clonic seizures may precede myoclonus, occur simultaneously with it, or appear some time after myoclonus. Often the first GTCS occurs several months after the onset of the first myoclonus and seems to be a debut symptom. Like myoclonus, GTCS dominate in the morning, immediately after waking up. GTCS often develops from a long series of myoclonus.
Provoking factors may include sleep deprivation, photostimulation, alcohol, physical activity, and menstruation. Sleep deprivation and forced awakening are of greatest importance.
Myoclonus in JME in most cases demonstrates praxis sensitivity and therefore quite often in such patients throwing away objects with which they manipulate (cutlery, toothbrushes, combs, etc.) occurs.
Intelligence in patients with juvenile myoclonic epilepsy is normal. Significant pathology of the central nervous system is usually not detected.
Interictal EEG may be normal in 7-10% of patients. The most typical EEG patterns in juvenile myoclonic epilepsy are generalized bilateral “peak-wave” or “polypeak-wave” complexes with a frequency of 3-5 Hz lasting from 1 to 20 seconds. The ictal pattern is represented by discharges of polyps with a frequency of 10-16 Hz. Each digit can have from 5 to 20 individual peaks.
The frequency of photosensitivity in JME is the highest among all idiopathic generalized epilepsies - about half of the patients.
Treatment for JME is most often lifelong. Relapses occur in 85-90% of cases.