Epilepsy drugs
Epileptic seizures occur when potassium leaves nerve cells at the same time calcium and sodium enter it. An impulse failure occurs, which provokes the release of neurotransmitters. Some activate the attack (glutamate), others inhibit it (GABA). Antiepileptic drugs are necessary in order to properly influence neurotransmitters and normalize the functioning of neurons.
AEDs are classified into different groups based on their mechanism of action:
- sodium and calcium blockers;
- glutamate blockers;
- GABA receptor stimulants;
- multiple action drugs.
There are also the following groups of drugs against epileptic seizures:
- anticonvulsants (anticonvulsants);
- sedatives (calming);
- vitamin complexes.
All medicines are produced in the form of tablets (capsules, granules), syrup (drops), powders for solution, injections. Each form of drugs has different bioavailability (rate of absorption into the blood):
- Solid (tablets, capsules). They can be slow or immediate. The former are used more often due to the absence of a sharp increase in the concentration of the active substance, which leads to its rapid decrease and reduction of the effect - this is how immediate-release tablets work. The delayed type is preferable due to the long-lasting effect, which allows you to minimize the number of medications taken.
- Soluble. The granules can be dissolved in water or yogurt - this method of consumption is well suited for small children or people with swallowing disorders.
- Liquid (drops, syrups). They are considered the most convenient for treating children and the elderly due to ease of use. Usually the packaging contains measuring devices (spoon, syringe).
- Injections. Indispensable in urgent situations due to its high bioavailability, when it is necessary to quickly relieve an acute attack. Most often used in hospitals or by emergency doctors.
Anticonvulsants
Anticonvulsants help prevent, reduce, or completely eliminate an epileptic seizure. Anticonvulsants block the excitation of nerve cells and activate GABA receptors, which inhibit excitation. Today doctors prescribe medications based on the following active ingredients:
- Sodium valproate. Increases the amount of GABA and stimulates its activity.
- Ethosuximide. Blocks calcium and sodium channels, weakens the effect of glutamate.
- Carbamazepine, phenytoin. Reduce the number of neurons in sodium channels, reduce the effects of amino acids and glutamate.
- Phenobarbital, primidone. Accelerate the activity of GABA receptors in calcium channels.
- Lamotrigine, oxcarbazepine, oxcarbazepine. They reduce the excitation of sodium neurons and inhibit glutamate activity.
- Levetiracetam, topiramate. They have multiple effects on nerve cells and neurotransmitters.
- Tiagabine. Blocks the attack of GABA by neurons, increases the concentration of beneficial neurotransmitters.
- Gabapentin. In addition to activating calming receptors, it relieves pain and tension.
Sedatives
Epileptics are often prescribed sedatives and sleeping pills - the active substances in tablets and injections help relieve stress, calm the nervous system and weaken the effect of impulses that provoke seizures. Usually prescribed:
- Valerian. Relaxes muscles, normalizes heart rate, suppresses attacks.
- Afobazol. It has a gentle effect on the nervous system and improves sleep.
- Relanium. Relieves anxiety, fears, overexcitement.
- Tenoten. Relieves psycho-emotional stress without atrophying muscles.
- Antidepressants. Prevents stress, panic and depression, which often cause seizures.
Other drugs
- Painkillers. An epileptic attack may be accompanied by pain in the head and muscles. Analgesics eliminate pain and additionally have an anti-inflammatory, vasodilating and calming effect.
- Hormonal. Most hormones in excess provoke an attack, but some of them (for example, dexamethasone) stop the transmission of impulses.
- Nootropic. They promote normal brain function while suppressing the activity of neurotransmitters.
Some doctors prescribe dietary supplements as a form of prevention and additional stimulation of the positive effect of drugs. It is not recommended to choose biological additives on your own - despite their plant origin, certain components can be harmful.
Vitamins and minerals for epilepsy
Vitamin and mineral complexes are especially necessary for young children or people following a ketogenic diet. With epilepsy, the patient has limited nutrition, which negatively affects physical and mental development. What vitamins and minerals restore the body’s functioning:
- B vitamins: For healthy metabolism and energy, the body needs folic acid, B6 and B12 - they eliminate drug resistance.
- Vitamin D. In epileptics, the liver actively produces enzymes that flush vitamin D from the body. Calcium deficiency threatens osteoporosis.
- Antioxidants. Taking medications reduces the amount of selenium, vitamins C and E, so the use of antioxidants is included in the medication course.
- Magnesium. Necessary for maintaining the balance of neurotransmitters, as well as for the inhibition of calcium channels.
- Melatonin. Inhibits excitatory receptors and glutamate, helps restore sleep and the biological rhythm of life, gives strength and energy.
- Omega-3. Fatty acids are essential for epilepsy due to their anticonvulsant effect. Large amounts of fat in the blood stimulate the production of ketones, which replace the stimulating glucose but are not harmful.
Types and stages of status epilepticus
The variability and diversity of types of epileptic seizures is the main basis for the formation and identification of forms of epileptic seizures, characterized by general signs of the clinical picture of the disease. They are divided into two groups: non-convulsive and convulsive. Classifying the types of ES, we can distinguish:
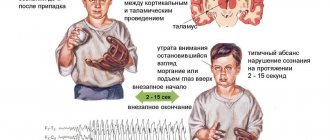
- Generalized non-convulsive seizure. In this case, a short-term loss of consciousness is observed. The patient seems to freeze with interrupted activities (eating, talking, writing...), or thinking about something. In this case, the eyes are focused on one point, the face becomes pale, and the connection with the outside world is interrupted. The absence seizure stops as suddenly as it started.
- Incompletely generalized status epilepticus is characterized by muscle cramps, the patient completely loses consciousness, cardiovascular activity is disrupted, and breathing becomes unstable.
- Tonic SE is typical for children of different ages with rare and severe forms of epilepsy.
- Clonic ES, accompanied by high fever and convulsions in children and infants.
- Myoclonic ES is expressed in episodic twitching of muscle tissue.
Epileptic seizures are characterized by short duration. Usually a seizure lasts several seconds, or several tens of seconds, less often - a minute. After status epilepticus, relief occurs spontaneously, without outside intervention. Therefore, they are called self-limited epileptic seizures. Serial attacks following one after another are often encountered.
In medicine, each stage of epistatus, which is a complication of epileptic syndrome, has its own name:
- The duration of the pre-status stage can last from 1 to 10 minutes;
- The initial stage is characterized by the duration of the attack from 10 to 30 minutes;
- Expanded - from 30 to 60 minutes;
- The stage, which lasts more than an hour, is called refractory.
Epistatus is a state of a person when he does not regain consciousness during alternating epileptic seizures. Before one attack has finished, the next one begins. The second variant of epistatus is no less dangerous, and is a seizure lasting more than 30 minutes.
Complications of status epilepticus
Epistatus is characterized by irreparable consequences. Statistics. With symptomatic ES, mortality is 30–50%. With ES in patients with epilepsy - 5%.
If ES lasts more than an hour, then patients will face serious consequences:
- Diffuse saturation of brain tissue with fluid, called cerebral edema and accompanied by oxygen starvation;
- Critically low blood pressure;
- Excessive levels of lactic acid, called lactic acidosis;
- Violation of water-salt balance;
- For children, characteristic signs are delays in the development and formation of the psyche, which can lead to mental retardation.
Non-convulsive epistatus is considered less dangerous compared to generalized epistatus. Nevertheless, complications of status epilepticus often find expression in disturbances of perception, attitude, thinking, memory, and understanding.
Symptoms of status epilepticus
Symptoms of epistatus are expressed in circulatory disorders, disturbances of consciousness (the person “switches off”), and disruption of the respiratory system. Symptoms of status epilepticus are a consequence of previous seizures from which the patient does not recover.
Epistatus can be characterized by a frequency of attacks up to 20 per hour. The patient does not regain consciousness at the onset of the subsequent seizure; his condition can be described as numbness bordering on coma.
The comatose state worsens in direct proportion to the duration. Tonic spasms affect the muscles of the back, arms and legs. High blood pressure suddenly drops. Increased reflexivity is also unexpectedly replaced by a complete lack of reaction.
Respiratory and circulatory disorders become obvious. When the seizures disappear, epileptic prostration occurs.
The duration of the epistatus is at least 30 minutes. Usually, as expected, we draw a line between this condition and episodic seizures with partial restoration of physiology and consciousness (full or partial).
There are two phases that characterize epileptic convulsive status with the following features:
- Compensatory changes in the circulatory and metabolic system, expressed in high blood pressure, vomiting and nausea, uncontrolled urination and defecation.
- Coming in about half an hour/hour, it is a maladaptation of compensatory changes, which is expressed in acute renal failure (and liver failure), a sharp decrease in pressure, disruption of the respiratory system, and arrhythmia.
Epistatus, the course of which is not accompanied by convulsions, is characterized by complete immobility of the patient and a feeling of detachment. Usually the patient lies with his mouth open, his blank gaze does not express anything.
Emergency care for status epilepticus
First aid for status epilepticus, before the arrival of doctors, is the need to protect the patient from receiving mechanical injuries. There is no need to crowd around the patient, blocking free access to clean air.
Our recommendations:
- Place the patient on a non-traumatic surface with something soft (jacket, sweater) under his head;
- To avoid choking on saliva, carefully turn your head to the side;
- Remove the tie, belt, unbutton the collar so that nothing interferes with the patient’s ability to breathe freely;
- Remove all sharp and traumatic objects located nearby;
- If your teeth are clenched, there is no need to unclench them;
- If your mouth is open, place any soft cloth between your teeth.
You should not place sharp, metal or other objects between your teeth that could cause injury to an unconscious person.
Emergency care for status epilepticus should be provided very carefully. You should not hold the patient too tightly so as not to damage his bones (in this condition the likelihood of fractures is very high).