Epilepsy is a serious chronic disease characterized by uncontrolled spontaneous seizures of various types. The disease may be congenital or acquired.
The first epileptic seizures can occur at any age; their development is due to many reasons: from genetic predisposition to previous neuroinfections and traumatic brain injuries.
Epilepsy that appears in adults threatens a significant deterioration in the quality of life and even disability. Due to the spontaneity of attacks and the inability to control them, a person loses working capacity. Epileptic seizures negatively affect not only the physical health of the patient, but also his psychological state, which is expressed in the development of psychosis and depression.
There are certain provoking factors, the presence of which can increase the likelihood of epileptic seizures. If they are present, the patient needs to regularly visit a neurologist to prevent attacks and receive timely medical support.
The Yusupov Hospital provides high-quality diagnosis and treatment of epilepsy. Modern medical equipment at the diagnostic center of the Yusupov Hospital provides the most accurate results - identifying pathology in the early stages and establishing the root cause of the disease, which in turn makes it possible to select the most effective treatment regimen. Therapeutic tactics are drawn up taking into account the individual characteristics of the patient and the severity of the pathology.
Thanks to the use of innovative methods, treatment significantly improves the condition of patients with epilepsy and allows them to achieve stable remission.
Causes of the disease
Epilepsy can be idiopathic or symptomatic in nature. The reasons for the development of idiopathic epilepsy remain unclear. The pathology can be diagnosed in people both at an early and mature age, but is most often found in children. Scientists believe that one of the most likely causes of idiopathic epilepsy is hereditary predisposition. In addition, it can occur as a result of genetic abnormalities formed in the child during the prenatal period.
The occurrence of symptomatic epilepsy is associated with one or another negative circumstance that has a negative impact on the structures of the brain. Thus, an epileptic attack is provoked by the following factors:
- repeated flashes of light and color;
- repetitive sounds;
- bright changing pictures, video effects;
- poisoning of various kinds;
- consumption of alcoholic beverages, drugs;
- taking certain medications;
- oxygen starvation;
- hypoglycemic attack - when there is a sharp drop in blood sugar levels.
You need to know that an epileptic seizure in a healthy person can be caused by one of the last three reasons.
Make an appointment
Provoking factors in children
Epilepsy is not considered a childhood disease, but is more often diagnosed at an early age. Depending on the form of the disease, it can manifest itself in different ways. Epilepsy is accompanied by convulsions and loss of consciousness. Early diagnosis in a child contributes to partial or complete recovery. By adolescence, all symptoms may disappear, and children will lead an active, full life.
The most common causes of epilepsy in children are:
- neck and head injuries during birth;
- hypoxia (oxygen starvation) of the fetus;
- infectious diseases suffered by the mother during pregnancy;
- maternal abuse of alcohol and drugs during pregnancy.
The disease can appear in a child immediately after birth or several years later. Minor convulsive movements in children under three months of age may be a consequence of an immature nervous system. However, if they are present, you should consult a neurologist to exclude pathology. If seizures continue to appear after three months of life, intensify and occur spontaneously, it is necessary to show the child to a pediatric neurologist.
Epileptic seizures in childhood can also be caused by high fever, so-called febrile seizures. Some attacks are accompanied by sudden freezing and short-term loss of consciousness. There is also absence epilepsy, which occurs without seizures. The symptoms of epilepsy are quite multifaceted. If there is even the slightest suspicion of epilepsy, then it is necessary to immediately do an electroencephalogram.
Parents need to pay attention to the following symptoms in their child:
- fading;
- loss of concentration;
- no reaction to stimuli;
- high temperature;
- fainting;
- lethargy;
- headache;
- nausea;
- stomach ache;
- dizziness.
If these symptoms occur, call a doctor immediately or take your child to the hospital.
Provoking factors in adults
Hereditary forms of epilepsy do not always appear at an early age. There are cases where patients of older age groups experienced their first epileptic attack, and upon examination it turned out that there was a genetic predisposition. Epilepsy is inherited, but depending on the form, it is not always accompanied by seizures.
The occurrence of epileptic seizures in adulthood is provoked by other factors:
- suffered a stroke;
- brain tumors;
- multiple sclerosis;
- metabolic disorders;
- infectious diseases with brain damage (meningitis, encephalitis, etc.);
- alcohol, drugs and other intoxications.
Traumatic brain injuries can cause epilepsy in people of any age. Damage to the bones of the skull, hemorrhage in the brain and disruption of the integrity of soft tissues may be accompanied by the development of pathological processes with secondary epilepsy.
Symptoms of epilepsy in adults are varied. Sometimes attacks are not accompanied by convulsions and loss of consciousness. From the outside, the patient looks normal, but slightly inhibited. He has a vacant look, he may lose touch with reality and not respond to stimuli. Such symptoms are observed in mild forms of the disease.
Classic manifestations of epilepsy are much worse. The person may fall sharply and begin to convulse. In this condition, his jaws are strongly compressed, so the patient may bite his tongue. Foam appears on his lips. During an epileptic seizure, the patient may harm himself. Often the attack is accompanied by dislocations and fractures. Seizures can also be vegetative - without loss of consciousness or convulsions. They are characterized by the following types of symptoms:
- increased heart rate;
- excessive sweating;
- flatulence and cramping abdominal pain.
Nonconvulsive epilepsy can be caused by factors such as predisposition and exogenous influences. Epilepsy in adults is treatable. Only an accurate diagnosis in the early stages can guarantee success.
Expert opinion
Author: Olga Vladimirovna Boyko
Neurologist, Doctor of Medical SciencesRecently, doctors have noted an increase in cases of newly diagnosed epilepsy. The exact causes of this dangerous neurological disease have not been established. According to statistics, 4-10 people per 1000 population suffer from epilepsy. In Russia, the incidence rate accounts for 2.5% of cases. Numerous clinical studies have led to the following conclusion: 80% of patients with epilepsy live in countries with low and medium levels of development, where there is a high level of injuries and the prevalence of infectious diseases.
To diagnose epilepsy, doctors at the Yusupov Hospital use modern medical equipment. The clinic is equipped with European MRI, CT, and EEG equipment. Blood tests are carried out in a specially equipped laboratory. Experienced neurologists and epileptologists find out the possible causes of the disease. This is necessary to develop the correct treatment. Therapy is selected based on the individual characteristics of each patient. The drugs included in the treatment regimen meet European safety and quality requirements. To minimize the risk of relapse of the disease, patients are provided with preventive recommendations.
Neurocardiogenic or vasovagal syncope
This type of fainting is characterized by a young age of onset of the disease, multiple repetitions of episodes of loss of consciousness over many years. The patient mentions a tendency to motion sickness and lightheadedness at the sight of blood. Most often, such fainting occurs in warmth, at rest, after physical exertion. It begins in a standing or sitting position, never lying on your back. The prodromal period usually lasts from 30 seconds to several minutes and includes symptoms such as nausea, possibly vomiting, abdominal discomfort, a feeling of heat, cold sweats, a feeling of flushing, dizziness, an increasing feeling of lightheadedness leading to loss of consciousness. Such fainting usually does not lead to bodily harm or injury. Changing to a horizontal position can interrupt the loss of consciousness. Witnesses note marked lethargy and describe how the patient “slipped” to the floor during the attack. There is no disorientation or paralysis upon awakening. There may often be a feeling of extreme fatigue that lasts for several hours.
The first signs of an epileptic seizure
Often, the patient and his family are not aware of the presence of epilepsy until the first attack. It can be quite difficult to determine the reasons for its development and the specific irritant for the first time, however, the fact that an epilepsy attack is approaching can be suspected if the patient has certain signs:
- headache a few days before an epileptic seizure;
- sleep disorders;
- severe stress;
- nervousness and irritability;
- decreased appetite;
- loss of appetite.
During a convulsive attack, muscle tension and lack of response to any irritants are noted - patients do not hear sounds, do not respond to touch, pain, their pupils do not narrow or dilate. After an epileptic seizure, people become lethargic and drowsy; to restore strength and normalize their condition, they need rest and good sleep.
If convulsions last for a long time and symptoms worsen, patients need qualified medical care, for which they must immediately call an ambulance and, before their arrival, make efforts to prevent injury to the patient during convulsions. Without medical attention, status epilepticus can be fatal.
Manifestations of epileptic seizures
Epilepsy is characterized by uncontrolled spontaneous seizures, the occurrence and intensity of which cannot be predicted in advance. The disease can be suspected after the first attack occurs. If the attack recurs, you should immediately consult a neurologist, since in the absence of proper treatment, the frequency of epileptic seizures only increases over time.
One of the frequent precursors of an epileptic attack is the so-called aura. It is a subjective sensation of a hallucinogenic nature that occurs in a patient with epilepsy shortly before the onset of an attack.
The aura can be manifested by the following sensations:
- certain sounds (ringing or tinnitus, melody, other sounds);
- some odors;
- visual visions;
- a feeling of deja vu;
- headaches;
- increased anxiety, etc.
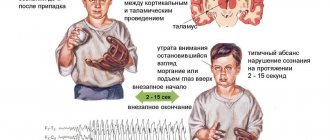
Certain types of seizures, such as absence seizures, are not accompanied by an aura. During absence seizures, patients lose consciousness. The patient freezes in place and does not respond to actions or words. In this case, fainting does not happen, the person simply seems to freeze. In cases of complex absence seizures, patients experience repetitive motor acts: during an attack, the eyeballs, lips, and tongue may move.
In reflex epilepsy, the appearance of seizures is provoked by a certain irritant. An epileptic seizure in such cases can begin as a result of exposure to bright light, a flash of light, light music in a nightclub, or a fast video sequence with a frequently changing picture. In some patients, the onset of an attack is preceded by emotional overstrain and listening to certain sounds. Therefore, people suffering from reflex epilepsy need to exclude situations with provoking factors.
In addition, epilepsy may be characterized by the following symptoms:
- convulsions: during an attack, tonic or clonic convulsions appear in the muscles of the upper and lower extremities;
- disorder of consciousness: some simple epileptic seizures are accompanied by the preservation of consciousness, others by turning it off or the patient falling into a coma. In addition, during an epileptic seizure, an epileptic may see hallucinations and mentally move to another place;
- autonomic disorders: during an attack, patients experience changes in pulse, blood pressure, and vascular tone;
- memory impairment: after the end of an epileptic attack, the patient most often cannot remember what happened to him. As the disease progresses and the frequency of attacks increases, epileptics experience impaired speech and thinking, which leads to dementia.
In the early stages of the disease, as a rule, simple epileptic seizures occur, characterized by a short duration and the absence of loss of consciousness. As the disease progresses, the condition worsens and attacks become more frequent with more noticeable consequences.
Make an appointment
A patient with syncope should be asked the following questions:
- At what age did you first faint, and how often do you faint?
- How long did it take from the moment you realized that “something was wrong” with you until you lost consciousness? This is a key question that will allow us to assess the course of the prodromal period.
- What were you doing when the symptoms appeared? What position were you in: lying, sitting, standing, in motion?
- What sensations did you experience before losing consciousness - nausea, fullness in the stomach, increased salivation, sweating, flushing, feeling hot or cold, sudden yawning, tingling or numbness in the arms and legs, flashing “floaters” before the eyes or distorted perception, spots before the eyes ?
- Did you feel any smells, sounds, or visual distortions before you lost consciousness? Were you injured during the fall?
- Did you feel dizzy, nauseous during injections or taking blood for analysis?
- Do you get motion sickness in transport?
- Did you understand what happened to you when you woke up?
- During fainting, did you bite your tongue or cheek, did you feel weakness in half of your body after waking up, did you experience urinary or fecal incontinence during the attack?
It is also important to ask questions to the witness of the syncope, especially when seeing an elderly patient with retrograde amnesia, such as:
- What did the patient complain about before he lost consciousness?
- How long was the patient unconscious?
- Did you have any convulsions while you were unconscious?
- did the patient make involuntary sounds during loss of consciousness?
- did the patient wet himself or lose stool?
- Was the patient tense or, conversely, lethargic at the time of loss of consciousness?
- did the patient look deathly pale, with a gray or sallow complexion?
- Did you quickly realize what happened after waking up, or was you disoriented and paralyzed?
These features of the anamnesis, obtained from the patient and from the witness, make it possible to most accurately identify the cause of fainting.
Types of disease
The following types of epilepsy are observed in patients of different age groups.
- Juvenile myoclonic epilepsy. Mostly occurs in teenagers. The attacks occur after waking up and are sometimes not accompanied by convulsions.
- Progressive myoclonic epilepsy. It is difficult to treat and can develop into a more complex and dangerous form of the disease throughout life.
- Symptomatic epilepsy. Older people suffer. The first signs of the disease may appear up to 30 years of age. The causes are head injuries and diseases of the nervous system. Due to the varied manifestations of the disease, it is difficult to diagnose as the symptoms can be misleading and the patient may be misdiagnosed even after a thorough examination.
- Temporal lobe epilepsy. Affects the temporal lobes of the brain. A common symptom is a state of “déjà vu.” This form of epilepsy also causes anxiety disorders, uncontrollable outbursts of anger and other emotional states.
- Frontal epilepsy. Symptoms vary and depend on which parts of the brain are affected. Affects the motor functions of the human body. The manifestations of this disease often do not cause concern. The patient may move his eyes and tongue rapidly, and stagnate. From the outside it may seem that a person is simply experiencing nervous excitement. At the same time, a person cannot organize his thoughts, experiences many emotions at the same time and cannot calm down or concentrate on one thing.
- Parietal epilepsy. It is quite rare. The symptom is visual disturbances or eye sensitivity to flashes of light. The eyes may move uncontrollably or jerk from side to side, and the eyelids may tremble. Severe headaches often occur during or after an attack.
- Absence epilepsy. Symptoms of this disease are characterized by short-term fainting or loss of consciousness. With rare exceptions, absence epilepsy is manifested by a loss of concentration; a person cannot focus, breaks off a sentence mid-sentence and cannot build a logical chain to convey his idea. His movements are unclear, his hands can move uncontrollably, inexplicable sensations arise in his fingers, so the patient wants to stretch his hands.
- Myoclonic epilepsy. Manifests itself with sudden spontaneous movements of the arms and legs. The symptoms of this disease are often ignored and confused with the completely normal hypnogogic myoclonus that everyone experiences when falling asleep.
In addition to the classification of epilepsy, individual forms of epileptic seizures are also distinguished.
Causes of fainting
Cardiovascular diseases
Syncope associated with cardiac output obstruction
- aortic stenosis
- mitral stenosis
- hypertrophic cardiomyopathy
Syncope associated with cardiac arrhythmia
Dysregulation of vascular tone and blood volume
- reflex syncope - neurocardiogenic (vasovagal) syncope
- carotid sinus hypersensitivity
- situational syncope (coughing, sneezing, swallowing, urination, defecation, orthostatic instability syndromes)
Primary causes of autonomic failure:
- True autonomic failure
- Multiple system atrophy
- Postural otostatic tachycardia syndrome
- Acute autonomic failure
Secondary causes of autonomic dysfunction
- additional causes of orthostatic instability
Other causes of fainting
- Hypoglycemia
- hyperventilation
Subclavian steal syndrome
- decrease in circulating blood volume
- Carcinoid
- medications
Multifactorial syncope (more common in older patients)
The basis of the clinical diagnosis of syncope is a carefully collected history, which is sometimes absent due to the presence of retrograde amnesia in the patient, especially in elderly patients.
Diagnosis of the disease at the Yusupov Hospital
No doctor can determine a reliable diagnosis after one single attack, since an epileptic seizure can occur once and in completely healthy people.
In order to establish the cause that provokes the development of an epileptic seizure, neurologists and epileptologists at the neurology clinic of the Yusupov Hospital collect information about the nature of the patient’s complaints, the presence of episodes of epilepsy and other neurological pathologies in the family, the presence of factors that negatively affect the state of the nervous system (regular stress, chronic fatigue and etc.).
After the examination, the neurologist prescribes laboratory and instrumental examinations using the latest equipment from the world's leading manufacturers of medical equipment. The clinic’s specialists interpret the results of laboratory tests and instrumental studies as accurately as possible.
Based on the data obtained, the diagnosis can be confirmed or excluded.
The following modern methods are used to carry out diagnostics at the Yusupov Hospital:
- computed and magnetic resonance imaging;
- angiography;
- electroencephalography;
- neuroradiological diagnostics;
- examination by an ophthalmologist of the fundus;
- biochemical blood test.
In some cases, a lumbar puncture is prescribed - a test that allows you to identify an infection that has affected the brain.
Make an appointment
Arrhythmic syncope
As a rule, these are patients over 60 years of age with a history of heart disease. Loss of consciousness occurs suddenly, with a minimal prodromal period (“I found myself lying on the floor”) and is often accompanied by physical injuries (fractures, cuts) and even an accident if the attack occurs while driving a car. The duration of the attack does not exceed 30-40 seconds.
Fainting due to congenital arrhythmic syndromes - the so-called channelopathies - is characterized by young age, a family history of sudden death in other family members, spontaneous miscarriages, sudden infant death. Loss of consciousness associated with fright, swimming (drowning), surprise. Fainting in males during physical activity, after eating a high-carbohydrate meal or poor sleep should raise suspicion of Brugada syndrome.
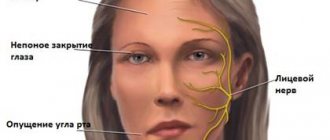
During epileptic seizures, from which it is very important to differentiate syncope, a typical aura occurs in the form of visual, olfactory, auditory sensations, often the same before each attack. Deja vu or jamevu. Personal injury is very common. Accompanied by fecal and urinary incontinence. Those around describe prolonged tonic-clonic convulsions, starting with stiffness, turning into lethargy, and note a turn of the head to the side during loss of consciousness. There is a bite of the tongue and cheeks. After the attack, there is confusion, disorientation, inability to remember events, and neurological deficits or paralysis of one side (Todd's palsy) often persist.
After collecting anamnesis, we perform a medical examination, during which we note the presence of injuries and physical injuries, which often indicate the presence of either cardiac pathology or the epileptic nature of the attack. Blood pressure is measured while lying on your back, sitting and standing for 30 seconds and after 2 minutes in a standing position, which helps to identify postural changes in pressure - orthostatic collapse. Pressure measurements must be taken on both sides to avoid missing aortic dissection. Heart examination - assessment of pulse, cardiac impulse, systolic ejection murmur at the base of the heart - to identify cardiogenic pathology. Also an important diagnostic technique is carotid sinus massage, which is carried out by applying pressure to the carotid artery high in the neck at the angle of the lower jaw for 5 seconds while continuously recording an ECG. After 30 seconds, similar events are carried out on the other side. A result is considered positive when provoking a pause of 3 seconds leads to the reproduction of clinical symptoms.
Along with a thorough medical examination, a 12-lead ECG is necessary. This completes the triplet, allowing a reliable diagnosis of fainting to be made. Additionally, the ECG allows you to predict the further development of events and the patient’s management tactics. Based on the data obtained, the doctor must determine whether the fainting event is an interrupted episode of sudden death or this condition is not life-threatening for the patient. This prediction is more important, even than making a diagnosis.
You can get advice from highly qualified specialists on the treatment of fainting in Samara at the specialized neurological clinic First Neurology, which is staffed by a neurologist, cardiologist, epileptologist and functional diagnostics doctor.
The diagnostic examination includes a study of biochemical blood tests, ECG, ultrasound of the heart, and, if necessary, Holter, EEG to exclude epilepsy.
We are waiting for you at one of the three clinic addresses.
Treatment at the Yusupov Hospital
To alleviate the condition of patients suffering from epilepsy, the specialists at the neurology clinic at the Yusupov Hospital have several methods at their disposal. Properly selected treatment and strict adherence by the epileptic to medical recommendations can achieve stable remission for a long time.
Drug treatment helps to reduce electrical activity in the lobe of the brain where the disease, previously identified through EEG (electroencephalography), is localized. Treatment of patients at the Yusupov Hospital is carried out using the most modern medications that have a pronounced therapeutic effect and have minimal side effects.
Specialists at the Neurology Clinic of the Yusupov Hospital develop an individual treatment regimen for each patient, taking into account the form of epilepsy, duration and frequency of epileptic seizures, thereby achieving a significant improvement in the condition of patients after seizures.
During drug treatment at the Yusupov Hospital, patients are constantly monitored by doctors who monitor the course of the disease.
In what cases is hospitalization required?
The patient must be taken to the hospital:
- if epilepsy was detected for the first time - to conduct research and select effective treatment;
- with status epilepticus;
- in case of planning surgical intervention (in particular, removal of a brain tumor accompanied by epileptic seizures);
- in order to routinely assess the dynamics of the disease.
For patients at the Yusupov Hospital suffering from epilepsy, additional accompanying methods are used: physical therapy, psychological personality correction, bioacoustic correction of the brain, etc.
Physical therapy exercises, supervised by an experienced physical therapy doctor, can normalize the processes of excitation and inhibition in the brain, which are most often disturbed in epileptics. Special rhythmic movements and breathing exercises have a positive effect on neurons, harmonize the mental state of patients, and prevent stress and other diseases.
Read also
Restless legs syndrome
Restless legs syndrome - manifests itself as unpleasant sensations in the lower extremities, mainly in the evening and at night, forcing you to make relief movements with your legs, which leads to impaired…
Read more
Gliomas
What is a glioma? Glioma is a neuroepithelial tumor, a type of tumor of the central nervous system, the source of growth of which is glial tissue. In turn, glial tissue (glia) ...
More details
Brain concussion
A concussion is a mild traumatic brain injury without damage to the bones of the vault and base of the skull. In this condition, there are no pronounced disturbances in the functioning of the brain and there are no changes...
More details
Sudden memory loss/transient global ischemia
Transient, that is, temporary memory loss occurs in elderly patients and people suffering from migraines. At the same time, memory for past and present events disappears. But the person is conscious, accessible...
More details
Clubfoot
Clubfoot should not be understood as just one foot disorder. This is a group of deformities of the foot and ankle joint with their pathological setting. Clubfoot is a deformity in which...
More details