Causes
The causes of migraines are not fully understood. It is believed that the attack itself is a regional dystonic vasospasm, which leads to ischemia and changes in the metabolism of nerve cells. There is also a dysregulation of the system of one of the neurotransmitters - serotonin. However, it is much easier to trace the factors that provoke a migraine attack. These factors include:
- Alcohol consumption.
- Drinking coffee and caffeine-containing products.
- Stress and psycho-emotional tension.
- Changes in weather conditions.
- Changing your sleep schedule (either decreasing or increasing sleep time).
- Taking certain medications (primarily hormonal oral contraceptives).
Symptoms
The clinical picture of the disease is very variable, the symptoms of migraine can differ significantly from person to person, despite the fact that the main one is headache.
In this case, we should highlight the most common signs of migraine, the presence of which allows us to make a diagnosis:
- Paroxysmal development of headache with a certain time of its occurrence (from several hours to 2-3 days).
- Localization is predominantly in the fronto-orbital region.
- The monotony of the course of all attacks.
- Presence of nausea, vomiting, photophobia, sound fear.
- High intensity of pain, up to the need to take a lying position.
- Having a family history.
- With concomitant diseases (for example, the consequences of a traumatic brain injury), the patient can clearly distinguish between two different types of headaches.
Note:
“Classical” signs, such as unilateral, throbbing pain, cannot be considered mandatory.
Migraine with aura is also characterized by the development of visual (flickering spots, sparks before the eyes, flashes of light), sensory (impaired sensitivity), speech, and less often motor disturbances, developing within half an hour and completely disappearing in a short period of time. As a rule, the aura develops immediately before the attack, which allows the person to take the medicine in a timely manner.
Migraine
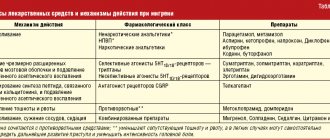
In accordance with the criteria of the International Classification of Headache Disorders, 2nd revision (ICHD II), migraine is defined as paroxysmal conditions manifested by attacks of intense headache of a pulsating nature, periodically recurring, localized mainly in one half of the head, mainly in the orbital-frontotemporal region, accompanied in most cases by nausea, vomiting, poor tolerance of bright light, loud sounds (photo- and phonophobia), drowsiness, lethargy after an attack. Migraine affects women more often: the ratio is 3:1, 4:2 “in favor” of women. Migraines typically occur between the ages of 18 and 33. Almost all people (according to world statistics, 75–80%) have suffered at least one migraine attack in their lives. The onset of the disease in childhood is less common, although cases of migraine in 5-year-old children are known. After 50 years, migraine as an independent disease is quite rare, but in the literature there are descriptions of cases of typical migraine occurring in patients over 60 years of age. It has been noted that migraine in older people occurs in almost equal numbers of cases - both in men and women. Hereditary factors play an important role in the occurrence of migraine: in relatives of patients, migraine occurs much more often than in the population; in the presence of migraine in both parents, the risk of the disease in offspring reaches 60–90% (while in the control group - 11%), while the leading role belongs to the mother: the risk of disease in children is 72%. The mechanism of inheritance is not entirely clear: some authors point to a recessive type, others to a dominant type. Perhaps the inheritance of a certain neurochemical defect (in particular, insufficiency in the metabolism of brain amino acids, especially serotonin) plays a significant role. There is an opinion about the inheritance not of the disease itself, but of a predisposition to a certain type of response of the vascular system to various stimuli. In the modern International Classification of Diseases (ICD - X) of 1988, the following forms of migraine are identified: - migraine without aura (formerly simple migraine), which occurs in 70% of cases; – migraine with aura (associated), i.e. a form in which an attack of pain is preceded by a complex of focal neurological symptoms (visual, sensory, motor disturbances). This is a rarer form, observed in 30% of cases. Within the latter, forms are distinguished depending on the type of aura: typical (formerly classic ophthalmic migraine), with a prolonged aura, with an acute onset of aura, migraine with aura without subsequent headache, while the aura is often represented by visual disturbances and alternates with typical migraine attacks. Further, depending on the vascular basin included in the pathological process, the following forms of migraine are distinguished: ophthalmoplegic, retinal, basilar, etc. The classification presents childhood periodic syndromes that can be precursors of migraine or combined with it, for example, benign paroxysmal vertigo in children (as the equivalent of migraine if there is a history of migraine). The classification also identifies complications of migraine: status migraine (a series of severe, successive attacks or one unusually severe and prolonged, usually with vomiting, rare - 1-2% of cases) and migraine stroke (development against the background of migraine with aura cerebral vascular accident). A column has been left to describe new types of migraine disorders. Based on a number of studies of autonomic changes in migraine patients O.A. Kolosov and V.V. Osipova (1998) distinguish vegetative or panic migraine. This form is characterized by the appearance of symptoms of a panic attack against the background of a typical migraine attack (according to the classification in DSM-IV): tachycardia, feelings of fear, anxiety, respiratory disorders (feeling of lack of air, suffocation), chill-like hyperkinesis, polyuria. These attacks are more severe and prolonged and require a special therapeutic approach. Diagnostic signs of migraine without aura are: • as a rule, hemicranial localization of headache; • pulsating nature of this pain; • pronounced intensity of pain, aggravated by physical work and walking; • the presence of all or one or two accompanying symptoms (nausea, vomiting, sensitivity to light and sound); • attack duration from 4 to 72 hours; • at least five attacks in history that meet the above criteria. For migraine with aura, in addition to the mentioned signs, the following provisions are mandatory: • not a single aura symptom should last more than 60 minutes; • complete reversibility of one or more aura symptoms indicating focal cerebral dysfunction; • the duration of the “light” interval between the aura and the onset of headache should not exceed 60 minutes. The course of attacks during migraine without aura consists of three phases. The first phase of prodromal phenomena in the form of mood changes (anxiety, anxiety, depression, less often euphoria), irritability, tearfulness, decreased performance, drowsiness, yawning, changes in appetite, thirst, and the appearance of local edema. The duration of this phase is several hours; it is often absent in migraines without aura. The second phase is the onset of pain. An attack can begin at any time of the day, while, according to our observations, night attacks (i.e. attacks that occur during sleep) have a more severe course, are more often accompanied by edema, and are less easily controlled. At the beginning of an attack, pain is usually localized in the frontotemporal region, the eyeball, mainly on one side (according to our data, more often on the right - up to 50%, on the left - up to 30%), bilateral - 20%. The nature of the pain is pulsating, less often aching, bursting; The pain intensity increases over 2–5 hours. Pain is accompanied by a decrease in the threshold of excitability of the sensory organs, which manifests itself in increased pain from bright light, loud sounds, and strong odors. Any touch to the body can become unbearable. Each beat of the pulse, as patients put it, “feels in the head like a hammer blow.” The behavior of a migraine sufferer during an attack is very typical: the patient tries to retire, go to bed, darken the room, cover his ears with a pillow, wrap himself in a blanket. In some patients, a swollen temporal artery is detected, and its pulsation is sometimes visible. Patients often apply strong pressure to the artery, as stopping the blood flow can reduce the throbbing pain. On the side of pain, the vessels of the conjunctiva are injected, the eye is watery, the periorbital tissues and the temporal region are swollen. As a result of swelling of the soft tissues of the face, the capillary network is compressed, the face turns pale, and the skin around the eye is cyanotic. During an attack, the headache can spread to the entire half of the head or, less often, to the entire head, then the throbbing pain is replaced by a feeling of fullness, “splitting,” squeezing, nausea occurs, and in some cases repeated vomiting, which sometimes weakens further manifestations of the attack, coldness of the distal extremities , chills The average duration is from 8 to 20 hours. The third phase is a gradual decrease, “attenuation” of pain, lethargy, drowsiness, weakness (from several hours to a day). The frequency of attacks is different, their frequency is individual. With migraine with aura, there may also be a prodrome phase, but more often the first phase is an aura, the clinical picture of which depends on the localization of the pathological process, then the pain phase and the post-attack phase. In the group of migraines with aura, the most common (up to 28%) is the ophthalmic (or classical, typical) form, which is characterized by various visual disorders, which in most cases manifest themselves in a flickering scotoma: the patient sees sparkling zigzags, dots, balls, fiery figures, lightning-like flashes, broken lines reminiscent of the battlements of a fortress wall, etc., after which an attack of headache develops (described for the first time in 1887 by the outstanding French neurologist J.M. Charcot). Brilliant photopsia may be replaced by the loss of certain parts of the visual field or the loss of half of the visual field (hemionopsia). If visual disturbances occur in the right half of the visual field, then the headache is localized on the left, and vice versa, although in 10–15% of patients the pain occurs on the same side. Auras, as a rule, are stereotypical for each patient. Some people experience visual illusions before an attack of headache: all people, things, objects seem elongated (“Alice syndrome,” which received its name from the description of a similar phenomenon in L. Carroll’s book “Alice in Wonderland”) or reduced in size, sometimes with a change coloring. Such visual disturbances are more common with migraine in childhood. In the neurological status of patients with migraine without aura and migraine with aura in the interictal period, as a rule, no deviations are observed. According to O.A. Kolosova, in 14–16% of cases there were neuroendocrine manifestations of hypothalamic origin (cerebral obesity, menstrual irregularities, hirsutism, etc.), most represented in the group of patients with panic migraine. In the somatic status, in 11–20% of cases, pathology of the gastrointestinal tract was identified, which was more pronounced in men. They also showed a tendency to arterial hypertension. Many works are devoted to the personality characteristics and mental state of migraine patients. The literature contains the names of many prominent people who suffered from migraines: Guy Julius Caesar, E. Poe, G. Heine, G. Maupassant, R. Wagner, F. Chopin, P. Tchaikovsky, C. Darwin, Z. Freud. It is believed that there is a special migraine personality, characterized by increased excitability, touchiness, conscientiousness, behavioral activity, a high level of aspirations, and intolerance to the mistakes of other people. “Perfectionist” is a common description of migraine sufferers. However, many authors do not recognize the existence of a special personality type for a migraine patient. We can say with confidence that people suffering from migraine are characterized by a special sensitivity to distress: high stress availability and low stress resistance, a tendency to anxiety and depressive reactions, behavioral and emotional lability, which, in combination with severe autonomic dysfunction in these patients, allows us to consider them as patients with psychovegetative syndrome. “Danger signals” in the diagnosis of migraine cephalgia are: changes in the nature and/or intensity of attacks with a long history of migraine, late “onset” (50 years or more), the appearance of neurological symptoms and previously absent accompanying symptoms such as vomiting, etc. d. They are and require a thorough examination of patients using neuroimaging methods to exclude the symptomatic form of migraine, which is a mask of a growing process, vascular pathology (aneurysm). Treatment of migraine Treatment of migraine includes two approaches: stopping a cephalgic attack and carrying out preventive therapy. During an attack, due to the short duration of the vasoconstrictor phase, it is advisable to use analgesics at the very beginning, before severe pain appears. But, as a rule, they are taken at the peak of pain, which, naturally, is ineffective. Basic drugs that directly affect the mechanism of development of a pain attack are listed in Table 1. Non-steroidal anti-inflammatory drugs are also used to relieve an attack. In case of severe attacks (status migraine), the patient should be hospitalized. Intravenous drip administration of dihydroergotamine is carried out, however, a history of long-term use of ergotamine is a contraindication to its use for relief of the status. The attack can be stopped with sedatives, dehydration agents, and antidepressants. You can use the following combination: seduxen intravenously slowly 0.5% solution from 2 to 4 ml per 20 ml of 40% glucose solution and melipramine 0.025 g orally or 1.25% solution 2 ml intramuscularly, as well as furosemide - 2 ml of 1% solution. In case of indomitable vomiting, in addition to antihistamines, you can use a 0.5% solution of haloperidol (1–2 ml), or a 0.25% solution of trifluperidol, or a 0.2% solution of triftazine intramuscularly. Treatment during the interictal period Medications that can be used for a long time (i.e., not only to stop an attack, but also to prevent it) include serotonin antagonists - methysergide, sandomigran, cyproheptadine. All these drugs in large doses stop the attack, then courses of maintenance therapy are carried out for several months. The next group is b-adrenergic blockers: anaprilin, etc. In recent years, reports have appeared on the effectiveness of migraine treatment with calcium blockers (nimodipine, verapamil, etc.). Antidepressants - thyricyclic and selective serotonin reuptake inhibitors - are often used with good effect. Currently, the high preventive effectiveness of some anticonvulsants, such as valproic acid derivatives, gabapentin, and topiramate, has been shown. It is important to emphasize that preventive drug measures are carried out only when the frequency of attacks is more than 2 times a month. In all other cases, it makes sense to carry out only anti-attack measures. It is necessary to take into account the frequency of attacks and the form of migraine. For frequent attacks of moderate severity and especially for panic (vegetative) form of migraine, complex therapy is recommended. For migraine with aura, it is advisable to include in complex therapy vasoactive drugs that improve microcirculation: nootropics, pentoxifylline, sermion, etc. For nocturnal forms of migraine, it is preferable to take drugs in the afternoon. In addition to drug therapy, rational psychotherapy can be used for all forms of migraine, as well as such means as auto-training, acupuncture, transcutaneous electrical neurostimulation, and biofeedback. Considering the frequent “inclusion in the process” of the muscles of the pericranial and cervical corset - massage, isometric relaxation, certain exercises, local physiotherapeutic effects - muscle relaxants can be added. Behavioral therapy is essential, the purpose of which is to teach the patient to stop his attacks and be able to prevent them. Diet, regular meals, and exclusion of foods containing tyramine (chocolate, cocoa, nuts, citrus fruits, beans, tomatoes, celery, cheeses), as well as drinks (dry, especially red wines, champagne, beer) are important. The duration of courses of preventive therapy should be at least 3 months, and often reaches 4–6 months.
Literature 1. Headache. In the book: Neurology for general practitioners. Edited by A. M. Vane. 2nd edition. Publishing house "Eidos Media", 2002, p. 18 – 48 2. Kolosova O.A. Headache. In the book: Pain syndromes in neurological practice. Edited by A. M. Vane. 2nd edition. Publishing house "Medpress", 2001, p. 106 –166 3. Levin Ya.I. Sleep and headache. Medicine for everyone. 1998, No. 4, pp. 27–29 4. Osipova V.V. International classification of headaches. J. Treatment of nervous diseases, 2003, No. 4, pp. 3 – 10
Diagnostics
Diagnosis of migraine includes a thorough collection of complaints and medical history. Often, characteristic complaints, as well as the absence of objective neurological disorders, allow a diagnosis to be made.
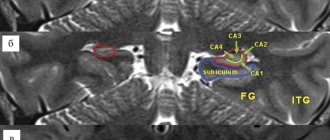
However, occasionally it is necessary to clarify the diagnosis and exclude focal brain lesions, hydrocephalus and other pathological conditions. In such cases, they resort to neuroimaging research methods (MRI, MSCT, etc.), neurophysiological research (EEG, REG, polysomnography), and the general clinical minimum.
Symptoms that should alert you
The following symptoms require contacting a neurologist to clarify the diagnosis and exclude various serious pathologies:
- headache occurred for the first time over the age of 50 years or in a child under 10 years of age
- pain occurred for the first time in a patient with cancer or HIV infection
- headaches get worse from attack to attack or attacks become more frequent
- sudden onset of headaches (like a “clap of thunder”) - this condition requires immediate attention to a neurologist
- headaches began to be accompanied by neurological or physical disorders that were unusual for the patient - for example, with a migraine without an aura, its sudden appearance, the duration of the aura for more than an hour (normally it should pass within an hour), the appearance of weakness during movements
- headaches clearly intensify when bending over, moving - i.e. in situations of increased intracranial pressure
- headache accompanied by an unreasonable increase in temperature
What can migraine pain be confused with?
It is necessary to differentiate migraine pain from the following:
- Toothache. A throbbing pain appears in the right or left half of the face, then it spreads to the temporal and occipital regions. There is no aura or harbingers.
- Cervical osteochondrosis. In addition to headaches and dizziness, it is accompanied by crunching and pain when moving the head, pain in the neck, chest, and shoulders.
- Cluster headache. Accompanied by ear congestion, acute pain behind the eye, redness, lacrimation, nasal congestion, sweating and facial flushing. The seasonality of the disease is noted.
- Temporal arteritis. It is accompanied by a headache on one side of the head, pain in the scalp of the affected area upon palpation, redness and swelling of the skin of the temple, fever, pain in the neck and upper extremities.
- Headaches caused by tumors in the brain.
Treatment and prevention
Unfortunately, treating migraine is a rather long and expensive process. It should be said that the indication for hospitalization in a neurological hospital is only diagnosed complicated migraine and the presence of migraine status (duration of severe pain more than 72 hours); other cases are treated on an outpatient basis. In an outpatient setting, you can use the complex effects of drug and non-drug therapy, normalization of the daily routine and lifestyle modification. Among the drugs used for migraine are vascular drugs, drugs that affect the serotonin system, non-steroidal anti-inflammatory drugs, and antiepileptic drugs.
Non-drug methods of therapy include massage of the collar area and scalp, as well as some physiotherapy. Electrosleep is very effective, as it significantly reduces the frequency of attacks.
Normalizing the daily routine consists, first of all, of maintaining a strict sleep schedule, excluding lack of sleep, as well as excessively long periods of sleep. Among the general recommendations, it should be noted the need to exclude a number of foods from the diet (primarily alcohol), as well as regular exercise therapy.
More detailed information about migraine medications, dosages, treatment regimens, and general recommendations can be found in the following article (read the article!).