Impaired production, absorption or circulation of cerebrospinal fluid causes the development of hydrocephalus. The disease is characterized by the accumulation of excess amounts of cerebrospinal fluid in the cavities of the brain. At the Yusupov Hospital, all conditions have been created for the treatment of patients suffering from internal hydrocephalus of the brain:
- cozy rooms of different comfort classes;
- examination using modern diagnostic devices from leading companies in the world;
- the use of effective drugs for treatment that have a minimal range of side effects;
- an individual approach to the choice of management tactics for each patient;
- attentive attitude of the staff.
The Neurology Clinic employs candidates and doctors of medical sciences, who are leading neurologists. All complex cases of internal hydrocephalus are discussed at a meeting of the expert council. Doctors make a collective decision on the treatment tactics for a patient suffering from severe hydrocephalus.
Types and forms of internal hydrocephalus
Depending on the cause of the disease, two forms of hydrocephalus are distinguished - open, communicating and closed (occlusive). Open hydrocephalus occurs as a result of increased secretion or impaired absorption of cerebrospinal fluid. Closed hydrocephalus develops when the patency of the cerebrospinal fluid outflow tract is obstructed by a tumor, inflammatory infiltrate, or adhesions.
Internal non-occlusive hydrocephalus can be congenital or acquired. Congenital hydrocephalus occurs during intrauterine development of the fetus. Acquired hydrocephalus develops under the influence of various diseases and injuries after the birth of a child.
The acute form of hydrocephalus is characterized by the rapid onset of symptoms of the disease within 3 days. In the subacute course of the disease, the increase in signs of hydrocephalus continues up to 1 month from the onset of the disease. Chronic hydrocephalus can take anywhere from several weeks to six months to develop.
Depending on the rate of progression of the symptoms of the disease, 3 forms of internal hydrocephalus are distinguished:
- progressive or active – occurs with rapid accumulation of cerebrospinal fluid and severity of symptoms;
- stabilized or passive – signs of the disease do not increase;
- regressive - symptoms of the disease disappear without treatment.
Neurologists distinguish compensated, subcompensated and decompensated stages of hydrocephalus. Depending on the level of intracranial pressure, there are hypertensive (with increased cerebrospinal fluid pressure) and normotensive (with normal intracranial pressure) internal hydrocephalus. Internal asymmetric non-occlusive hydrocephalus is characterized by dilation of one ventricle; in the presence of symmetric hydrocephalus, both ventricles of the brain are dilated.
general information
In neurology, hydrocephalus refers to an increase in the volume of spinal fluid - cerebrospinal fluid - in the cranial cavity. Occlusive hydrocephalus is formed when the cerebrospinal fluid ducts are blocked. This type of disease is defined as closed hydrocephalus, because the occlusion closes the cerebrospinal fluid circulation ring and leads to the accumulation of cerebrospinal fluid in it.
The International Classification of Diseases defines hydrocephalus as obstructive. In children and adults, occlusive hydrocephalus is found equally often and may be congenital. In case of acute occlusion, emergency medical care must be provided.
Causes of congenital internal hydrocephalus
Internal non-occlusive hydrocephalus of the brain develops under the influence of the following factors:
- infectious diseases of a woman during pregnancy (respiratory viral infection, mumps, herpesvirus or cytomegalovirus infections, rubella, syphilis);
- abnormalities of intrauterine development that interfere with the circulation and absorption of cerebrospinal fluid;
- brain injuries;
- inflammation of the substance and membranes of the brain (meningitis, meningoencephalitis, arachnoiditis);
- hemorrhage as a result of injuries and diseases of the cerebral vessels;
- oxygen starvation or cerebral circulatory disorders.
- intoxication with chemicals or alcohol;
- genetic defects.
Internal hydrocephalus of the brain in adults can develop in the presence of oncological tumors of the brain, which are localized in the cerebellum or brain stem, acute cerebrovascular accident (stroke), arterial hypertension, and diabetes mellitus.
What is hydrocephalus?
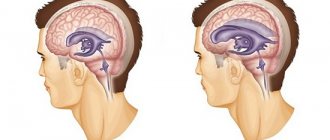
Nutrition of brain structures is carried out through a direct current of cerebrospinal fluid. Liquor circulates along a certain channel, ensuring continuous cerebral metabolism. Cerebrospinal fluid is needed for:
- protecting brain tissue from mechanical stress;
- ensuring a constant level of electrolytes;
- maintaining the balance of acids and alkalis;
- complete immunobiological protection.
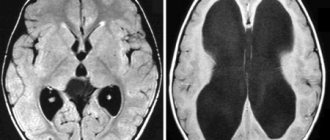
With hydrocephalus, there is a disturbance in the production, outflow and circulation of cerebrospinal fluid in the brain tissues. The disease is characterized by pathological accumulations of cerebrospinal fluid, which increases intracranial pressure. Clinically, hydrocephalus occurs in a severe form, with frequent attacks of the neurological type. A long-term pathological condition leads to the formation of secondary changes in brain tissue, which are usually irreversible. As a result of an uncontrolled course, hydrocephalus becomes the cause of death of the patient. Popularly, the disease has received a second name - dropsy of the brain.
Symptoms of internal non-occlusive hydrocephalus
The main symptom of hydrocephalus in children is an increase in the size of the head. In young children, the bones of the skull are thinned, soft, and the sutures between them diverge. A convex fontanelle stands out, which does not close for a long time. The skin on the skull is thin, shiny, and venous vessels are visible under it. Babies are lagging behind in physical and mental development, they are capricious, and cry constantly. The eyes are deep-set, looking down. Visual acuity decreases. With high intracranial pressure, nausea, vomiting occurs, and convulsions develop.
In older children, the signs of the disease worsen: irritability with attacks of aggression, lethargy, headaches, impaired memory, attention and consciousness. Coordination of movements and intelligence are impaired, learning problems appear, and mental retardation develops.
The characteristic signs of internal hydrocephalus in adults are:
- shaky, unsteady gait;
- loss of urinary control;
- memory impairment;
- headaches that are not always relieved by painkillers;
- blurred vision;
- vision deteriorates, pressure is felt on the eyes;
- nausea and vomiting.
Patients experience scattered attention and decreased concentration, and loss of thinking skills. Signs of mental disorders appear:
- emotional instability;
- attacks of aggression;
- neurasthenia;
- replacement of apathy with emotional upsurge.
Impaired motor functions appear. Impaired walking, contracture in the joints or paresis of the lower extremities develops. Patients often do not attach importance to these symptoms, mistaking them for signs of normal aging and do not consult a doctor.
What is Hypertension-hydrocephalic syndrome (HHS)?
Hypertensive-hydrocephalic syndrome (HHS) is caused by excessive accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain and under the meninges, resulting from obstruction of outflow, excessive formation and impaired reabsorption of cerebrospinal fluid. This is one of the most common syndromic diagnoses in pediatric neurology, especially in young children with perinatal encephalopathy (PEP). It should be noted that the term “hypertensive-hydrocephalic syndrome” is a concept used exclusively in Russia. The causes of HGS can be: unfavorable course of pregnancy and childbirth, hypoxic-ischemic brain damage, deep prematurity, intracranial hemorrhage and intrauterine infections, congenital malformations of the brain, neuroinfections. Research methods to judge the level of cerebrospinal fluid pressure are very limited. Currently, the only reliable and relatively accessible of them is to perform a lumbar puncture of cerebrospinal fluid (CSF) to measure CSF pressure, which is a diagnostic criterion for this pathology. HGS can be either one of the manifestations of hydrocephalus or many other neurological diseases. The diagnostic criteria for HGS include clinical symptoms that indirectly indicate an increase in cerebrospinal fluid pressure and dilation of the ventricles of the brain.
What is the prevalence of hydrocephalus? According to official statistics, up to 70% of newly born children suffer from an obvious (hydrocephalus) or latent form (hypertensive-hydrocephalic syndrome) of this disease.
What is the reason for the widespread incidence of hydrocephalus?
- Weakness of the nervous system of children born from parents who grew up in environmentally unfavorable conditions.
- A large number of “saved” premature babies.
- Frequent use of surgical delivery, which also contributes to the development of hydrocephalus.
- A busy schedule of vaccinations up to 1 year of age contributes to the exacerbation of latent hypertensive-hydrocephalic syndrome.
Early diagnosis (ultrasound, electropuncture) also helps to identify hidden forms of the disease hydrocephalus of the brain. There are many more reasons that can be found. But the fact remains: it is necessary to identify and treat hydrocephalus without waiting for exacerbations of the disease and complications.
What are the manifestations of hydrocephalus? In children under 1 year of age: increased excitability, “unreasonable” crying, sleep disturbance, frequent regurgitation, throwing the head back in sleep, increased muscle tone (hands held in fists, legs resting on toes and crossed), weak support with legs, lack of step reflex, delayed motor and mental development. In preschool children: hypermobility, aggressiveness, hysterical manifestations, stuttering, enuresis, strabismus, frequent colds, delayed psycho-speech development (poor vocabulary, impaired diction, difficulty constructing complex sentences). In schoolchildren: nosebleeds and headaches, memory and concentration are reduced, disinhibition and neuroticism are noted, learning school material is difficult: they complete tasks slowly, make a large number of mistakes, their hands get tired quickly, their handwriting is not even, they read slowly and poorly assimilate the material they read, find it difficult to write a competent story.
What are the worst complications of hydrocephalus? CONVISIONS, CEREBRAL PALSY, MORTONITY.
What factors cause exacerbation of hydrocephalus? Any stress on the body (viral infections, stress, mental and physical fatigue, concussion, vaccinations) can lead to an exacerbation of increased intracranial pressure - especially a combination of these. For example: studying at the gymnasium + flu + stress can lead to exacerbation of hydrocephalus, headaches and a decrease in academic performance and aggressiveness.
What to do if your child has any manifestations of hydrocephalus? Promptly seek advice from the children's department of neurology and reflexology at Reatsentr to clarify whether the child needs to be examined and treated.
Diagnosis of internal hydrocephalus
The clinical symptoms of internal hydrocephalus are usually so characteristic that they allow the neurologist at the Yusupov Hospital to suspect its presence during the first examination of the patient. To determine the type and degree of hydrocephalus, as well as to identify the pathological process that caused the disease, doctors conduct a comprehensive examination of the patient, which includes radiography of the skull, ultrasound, computed tomography or magnetic resonance imaging.
X-ray signs of hydrocephalus are thinning of the skull bones and divergence of the sutures between them; a symptom of “finger impressions” is observed on the inner surface of the cranial vault. With hydrocephalus caused by stenosis of the cerebral aqueduct, a decrease in the volume of the posterior cranial fossa is determined on radiographs of the skull. An increase in the volume of the posterior cranial fossa on craniograms is a sign of hydrocephalus in Dandy-Walker syndrome. If one of the interventricular communications is closed, the asymmetry of the skull is visible on the craniogram.
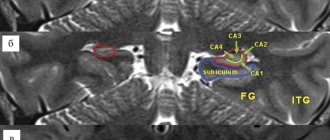
Echoencephalography (ultrasound) allows you to determine the degree of increase in intracranial pressure. In children of the first year of life, an ultrasound scan of the brain is performed through an open fontanel using ultrasonography. The most informative are tomographic diagnostic methods. They make it possible to determine the nature of hydrocephalus, identify the location of blockage of the cerebrospinal fluid tract or an existing congenital anomaly, and diagnose a neoplasm, cyst or hematoma. Monoventricular internal hydrocephalus is characterized by an increase in the volume of one ventricle of the brain.
If vascular disorders are suspected, magnetic resonance angiography is performed. For congenital hydrocephalus of infectious origin, PCR diagnostics are performed to determine the type of pathogen that caused it. Visual disturbances and the condition of the optic discs are assessed by an ophthalmologist at the Yusupov Hospital. Neurosurgeons at partner clinics decide on the need or advisability of surgical intervention.
Diagnosis and treatment methods for dropsy
Diagnosis of hydrocephalus is carried out in several ways. For example, using multislice computed tomography. As a result, the location of the pathology and its nature are determined - closed or open. The second common research method is MRI (magnetic resonance imaging), which provides accurate data on the condition of the brain vessels, the presence of structural changes and inflammatory processes.
In the early stages of identifying hydrocephalus, conservative treatment is prescribed - for example, medication. If the results are unfavorable, surgery is indicated:
- shunting for hydrocephalus involves draining excess fluid through a tube;
- external ventricular drainage - organization of a special drainage that is inserted into the cavity with cerebrospinal fluid;
- surgical removal of a septum, tumor, or blood clot that obstructs the movement of fluid.
Contraindications to surgery to eliminate symmetrical or asymmetrical hydrocephalus are severe cardiac pathologies, inflammatory processes in the nervous tissue, and serious problems with the blood vessels or respiratory system.
Neurosurgeons of the city clinical hospital named after. A.K. Eramishantsev will help cope with problems such as replacement, normotensive, triventricular, vicarious hydrocephalus. Sign up for a consultation to get more accurate answers to your questions. With timely intervention, the rehabilitation period after surgery occurs with minimal discomfort, and within a few days after surgery, adult patients can return to work, and children can return to school and a full-fledged active lifestyle.
Treatment of internal hydrocephalus of the brain
In the case of a compensated stage of the disease, neurologists at the Yusupov Hospital carry out dynamic monitoring of patients with hydrocephalus. Sometimes doctors prescribe diuretics, drugs aimed at improving cerebral circulation, and vitamin and mineral complexes. For severe internal hydrocephalus, drug treatment is prescribed in the initial stages of the disease. For patients, intracranial pressure is reduced and the condition is alleviated with diuretics, medications are used to treat the underlying disease that caused the dropsy, and the tumor is surgically removed.
The radical method of treating internal hydrocephalus is surgical intervention. During neurosurgery, a shunt is inserted into the brain and an output tube is inserted into the abdominal or pleural cavity, atrium, or bladder to create a new drainage path for cerebrospinal fluid. In the congenital form of the disease, it is left permanently. Bypass surgery is repeated several times during the patient's life. In case of damage to the veins, the development of infectious complications, epilepsy, or the formation of hematomas, the shunt is changed. In severe cases requiring urgent reduction of intracranial pressure and drainage of fluid, external drainage is performed.
At the partner clinics of the Yusupov Hospital, neurosurgeons use the neuroendoscopic method for treating hydrocephalus. Doctors are creating new pathways for fluid drainage using a neuroendoscope with a mini-camera. Endoscopic operations have a number of advantages: they are low-traumatic, do not require the installation of a foreign body - a shunt, complications rarely develop, and the patient’s quality of life increases.
If you have signs of internal hydrocephalus, call. You will be scheduled for an appointment with a neurologist. Doctors at the Yusupov Hospital use innovative methods for treating internal non-occlusive hydrocephalus of the brain.
Treatment of hydrocephalus
For this disease, medications are ineffective. Hydrocephalus is treated surgically. During the operation, the doctor installs a shunt system that allows cerebrospinal fluid to flow normally from the cavities of the brain into the abdominal cavity, and less often into the heart chamber or pleural cavity. The shunt system is equipped with a valve that prevents liquid backflow.
In some patients, ventriculostomy may be used. This is an endoscopic operation during which the surgeon makes a small hole in the wall of the 3rd ventricle of the brain. The normal outflow of cerebrospinal fluid then occurs through it.
Folk remedies for hydrocephalus have limited use. You can use tinctures of mint, lemon balm, cornflower, astragalus, calamus, and buckthorn berries.
Classification of hydrocephalus
Hydrocephalus can be congenital or acquired. It is generally accepted that the disease is diagnosed in children, but there is an increasing increase in cases of dropsy in adult patients.
According to the nature of the course, hydrocephalus can be:
- Acute - this form of the disease is characterized by a rapid course, the signs become obvious literally within three days.
- Subacute – symptoms increase and develop within one month.
- Chronic – the pathology develops for more than one month.
Diagnostics
The following diagnostic methods are used:
- The beginning of the examination is characterized by a detailed history taking. The onset of symptoms, the nature of their course, and the presence of primary pathology are determined.
- Neurological examination. The specialist determines intracranial hypertension and focal symptoms.
- Ophthalmological examination. The condition of the fundus and optic nerves is determined. Ophthalmoscopy, perimetry, and visometry are performed. Visual fields and visual acuity are examined.
- Echoencephalography. Determines intracranial hypertension, enlarged ventricles, and movement of brain tissue.
- Neuroimaging. In infants, it is performed using neurosonography through the fontanel. Adults are diagnosed using an MRI of the brain. In this way, developmental pathology and the location of the block of liquor vessels are determined.
Competent differential diagnosis excludes subarachnoid hemorrhages. In young children, it is important to exclude macrocrania, which is a hereditary feature.
Diagnostic methods
The optimal diagnostic method for hydrocephalus is an MRI scan of the brain. This study helps to clarify the type of hydrocephalus, determine the indications and choose the optimal treatment method for a particular patient. It should be noted that not every patient who consults a neurosurgeon with a diagnosis of Hydrocephalus requires neurosurgical intervention.
Remember that timely contact with a specialist allows in most cases to achieve control of hydrocephalus with a minimum amount of surgical intervention.
Causes
Cerebrospinal fluid moves through four ventricles - paired lateral ventricles, single - third and fourth. From the lateral ventricle, the cerebrospinal fluid passes through the interventricular window of Monroe and enters the third ventricle, then through the Sylvian canal into the fourth. Further, through the openings of Lyushko and Mozhandi, it flows into the cisterns of the cerebral and spinal subarachnoid subspace. If a barrier occurs along the path of cerebrospinal fluid circulation, occlusive hydrocephalus is formed.
The causes of occlusive hydrocephalus can be:
- Pathologies of brain formation. Native narrowing, immaturity of the aqueduct, Dandy-Walker syndrome, Arnold-Chiari pathology, are genetically determined or formed under conditions of prenatal infection, oxygen starvation of the fetus, or external influences. Hydrocephalus develops when the anatomical structure changes during fetal development or immediately after birth.
- Brain tumors. Tumors of the ventricles reduce their size, causing blockage of the associated lumens. Neoplasms of the cerebral cisterns block the passage of cerebrospinal fluid from the ventricles. The vessels through which the cerebrospinal fluid moves can be compressed by tumors of the brain stem. All pathological volumetric processes lead to accumulation of cerebrospinal fluid in the ventricles.
- Hematomas within the medulla. Formed as a result of traumatic brain injuries, after birth traumatic brain injuries, hemorrhagic hemorrhage in the brain. The cerebrospinal fluid ducts are blocked by the resulting hematoma, which forms occlusive hydrocephalus.
- Colloid cyst of the third ventricle is a benign neoplasm. The cyst closes the lumen of the Sylvian aqueduct and disrupts the cerebrospinal fluid flow, which gives rise to hydrocephalus.
- Hemorrhages in the cerebral ventricles. They are the result of injuries, disruption of the integrity of blood vessels, and arteriovenous pathologies. Blood coagulates in the cerebral ventricles, forming clots that block the physiological ducts in the brain structure.