Among the huge number of neurological diseases, stroke is the most important problem. Hemorrhage in the brain leads to disruption of intracranial circulation, neuronal necrosis and disruption of vital body functions. Only 10% of patients return to a normal, full life; the rest adapt to life with lost abilities. Some patients have to relearn how to speak, walk and perform basic everyday activities.
The vast experience and high professionalism of neurologists, physiotherapists, neurosurgeons, psychologists, and speech therapists at the Yusupov Hospital allow us to achieve the highest results. Patients who were abandoned by doctors in other medical institutions successfully undergo rehabilitation at the Yusupov Hospital and begin an active life.
A stroke is a brain pathology that develops as a result of destruction or blockage of the blood vessels that supply the brain. Blood stops flowing to the neurons and they die.
Stroke is divided into two types – ischemic and hemorrhagic. The first type is also called cerebral infarction. It develops due to poor blood flow to brain cells when neurons begin to die.
Hemorrhagic stroke develops due to hemorrhage in the brain when a vessel ruptures. In this case, even capillary bleeding is enough for the development of severe disorders.
In any case, be it an ischemic or hemorrhagic stroke, they develop in a matter of minutes and the patient requires immediate hospitalization. Timely medical assistance often saves the lives of patients at the Yusupov Hospital.
Periods of the disease
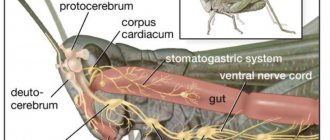
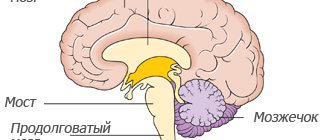
In ischemic stroke, a number of processes are observed that together lead to the death of neurons. Cell destruction occurs against the background of cerebral edema. At the same time, the brain increases in volume and intracranial pressure increases.
Due to cell swelling, displacement of the temporal lobe is observed, as well as infringement of the midbrain.
Compression of the medulla oblongata may also occur due to wedging of the cerebellar tonsils into the foramen magnum. This process quite often leads to death. Therefore, early hospitalization of the patient is extremely important.
When the first signs of an ischemic stroke appear, medical assistance should be provided within the first three hours, otherwise the prognosis is disappointing.
There are several periods of ischemic stroke:
- acute;
- spicy;
- early recovery period of stroke;
- late recovery;
- stage of residual effects.
Rehabilitation after injuries and operations on the musculoskeletal system
Home page › Medical rehabilitation › Rehabilitation after injuries and operations on the musculoskeletal system
Relevance
Traumatic injuries to the musculoskeletal system and surgical interventions on the spine and joints, unfortunately, are not uncommon, and no one is immune from them. As a rule, the injured part is immobilized for a long time, which leads to loss of mobility, swelling, circulatory disorders and muscle atrophy. As a result, a general weakening of the body occurs, immunity decreases and there is a danger of new diseases. Therefore, it is very important to carry out the correct rehabilitation course in a specialized medical institution under the supervision of qualified specialists.
Our experience and advantages
“Sanatorium named after Vorovsky” offers a full range of rehabilitation activities to patients after surgical interventions and injuries to the musculoskeletal system. Experienced doctors - orthopedic traumatologists, neurologists, chiropractors, physical therapy doctors, based on the latest techniques and long-term traditions of rehabilitation medicine, will assist you in restoring your functional state and returning to a normal active life.
It is important to note that the cost of our rehabilitation courses is much lower than similar programs in other specialized rehabilitation centers.
Indications for the rehabilitation course:
- Spinal injuries resulting from falls, bruises, compression and other impacts.
- Traumatic brain injuries.
- Limb injuries - fractures, cracks, joint injuries, dislocations, muscle and tendon ruptures, sprains.
- Conditions after endoprosthetics of large joints.
- Conditions after surgical interventions on the spine.
Course duration: 14-21 days.
Main components of the course:
- Reception and consultations with specialist doctors: traumatologist-orthopedist, therapist, physiotherapist, exercise therapy doctor, kinesthetic instructor.
- Diagnostics: blood tests, urine tests, ECG.
- Physiotherapy: magnetotherapy, laser therapy.
- Mechanotherapy.
- Gas baths.
- Therapeutic massage course.
- Drinking treatment with mineral water.
- Physiotherapy.
- Diet therapy.
- Climatotherapy.
Expected effect:
- Reduction or complete disappearance of pain.
- Elimination of edema and vascular disorders.
- Increased elasticity and muscle tone, formation of the muscle frame.
- Restoration of motor functions.
- Increasing tolerance to physical activity.
- General physical strengthening of the body and improvement of the psychological background.
Early recovery period after
injuries and endoprosthetics of large joints from 14 days to 6 weeks after surgery. The program is designed for 14, 18 and 21 days.*
Early recovery period ↓
| Diagnostics | |||
| Type of examination | Number of examinations | ||
| 14 days | 18 days | 21 day | |
| Appointment with an orthopedic traumatologist | 6 | 8 | 9 |
| Consultation with a physical therapy doctor | 1-2 | 2 | 3 |
| Consultation with a kinesthetic instructor | 3 | 3 | 4 |
| Consultation with a general practitioner | 1 | 1 | 1 |
| Consultation with a physiotherapist | 2 | 2 | 2 |
| General blood test | 2 | 2 | 2 |
| General urine analysis | 1 | 1 | 1 |
| Blood biochemistry (CRP) | 1 | 1 | 1 |
| ECG | 1 | 1 | 1 |
| Medical complex | |||
| Diet therapy for ARVD | 14 | 18 | 21 |
| Climatotherapy (gentle regimen, tonic) | 14 | 18 | 21 |
| Drinking treatment with mineral water | 14 | 18 | 21 |
| Physiotherapy | 8-9 | 11-12 | 14-15 |
| Massotherapy | 6 | 9 | 10 |
| Mechanotherapy "Artromot" | 10 | 12 | 15 |
| Physiotherapy or Bioptron on the postoperative suture area | 8 | 9 | 10 |
| Physiotherapy (laser therapy, Rikta magnetotherapy) | 8 | 9 | 10 |
| Gas baths (SUV or VRV) | 7 | 9 | 10 |
Collapse
Late recovery period
after injuries and endoprosthetics of large joints from 6-8 weeks to 10-12 weeks after surgery. The program is designed for 14, 18 and 21 days.*
Treatment program for patients with musculoskeletal diseases
| Diagnostics | |||
| Type of examination | Number of examinations | ||
| 14 days | 18 days | 21 day | |
| Appointment with an orthopedic traumatologist | 6 | 8 | 9 |
| Consultation with a physical therapy doctor | 1-2 | 2 | 3 |
| Consultation with a kinesthetic instructor | 3 | 3 | 4 |
| Consultation with a general practitioner | 1 | 1 | 1 |
| Consultation with a physiotherapist | 2 | 2 | 2 |
| Consultation with a dermatologist | 1 | 1 | 1 |
| General blood test | 2 | 2 | 2 |
| General urine analysis | 1 | 1 | 1 |
| Blood biochemistry (CRP) | 1 | 1 | 1 |
| ECG | 1 | 1 | 1 |
| Medical complex | |||
| Diet therapy for ARVD | 14 | 18 | 21 |
| Climatotherapy (gentle regimen, tonic) | 14 | 18 | 21 |
| Drinking treatment with mineral water | 14 | 18 | 21 |
| Physiotherapy | 8-9 | 11-12 | 14-15 |
| Massotherapy | 6 | 8 | 10 |
| Mechanotherapy "Artomot" | 9 | 13 | 16 |
| Physiotherapy or Bioptron on the postoperative suture area | 8 | 9 | 10 |
| Physiotherapy (laser therapy, Rikta magnetotherapy) | 8 | 9 | 10 |
| Pool with mineral water (physical therapy) or baths (mineral or radon or pearl or turpentine) | 7 | 9 | 10 |
| Underwater shower massage | 7 | 9 | 10 |
| Gas baths (SUV or VRV) | 7 | 9 | 10 |
| Heat treatment (peloid therapy or ozokerite or impregnation) | 7 | 9 | 10 |
Collapse
* The attending physician of the aftercare department makes the choice of the type of treatment from this program individually for each patient, depending on the individual condition and concomitant diseases.
The most acute period
In the first three hours, it is possible to restore blood flow and eliminate or reduce neuronal death through the use of thrombolytics. It is also possible to administer drugs into the stroke area itself, which helps prevent the development of complications.
Then doctors take measures to restore pressure, carry out rehydration, dehydration and oxygen therapy.
During the most acute period of a stroke (from 4 to 5 hours after the attack), the patient should be under the close supervision of a doctor in a hospital setting.
Early recovery period
The early recovery period is considered to be the period from 2 to 6 months after a stroke. At this stage, complex treatment is carried out:
- the patient takes medications according to an individual treatment regimen;
- in case of speech impairment, a speech therapist works with the patient;
- various manipulations are prescribed to restore sensitivity of the limbs and other parts of the body (massages, baths, acupuncture and others);
- physical therapy – the method helps strengthen ligaments and muscles.
Syndrome of movement disorders of the recovery period of perinatal lesions of the nervous system
About the article
11614
0
Regular issues of "RMZh" No. 1 dated January 10, 2006 p. 76
Category: General articles
Author: Zykov V.P. 1 1 Federal State Budgetary Educational Institution of Further Professional Education RMANPO of the Ministry of Health of Russia, Moscow
For quotation:
Zykov V.P. Syndrome of movement disorders during the recovery period of perinatal lesions of the nervous system. RMJ. 2006;1:76.
The recovery period of neonatal hypoxic-ischemic enphalopathy (NGIE) of moderate severity and periventricular hemorrhage (PVH) of II–III degree proceeds with the presence of persistent motor disorders in 46–50% of cases, in which disturbances of psychomotor development are detected in 70%, and in 30% of patients epilepsy develops [Akhtanina E.A., et al., 1997, Golenitskaya E.S. et al., 1997].
The evolution of motor disorders is associated with the stages of ontogenesis of the motor cortex: the peak of myelination of the corticospinal tract occurs at 4–6 months of postnatal development, which creates the conditions for the clinical manifestation of spastic syndrome by the first half of life. Currently, there are no standards for clinical and laboratory-instrumental diagnosis of movement disorders (MD) in infants, so in this article we tried to systematize our own and literature data concerning this problem. Clinical diagnosis A feature of DR in infants is hypotonic syndromes with central paresis. An early clinical symptom of DR in most patients is a delay in psychomotor development, and therefore the chronology of motor skills and reduction of innate reflexes, as well as a thorough analysis of anamnestic and somatic information play an important role in clinical diagnosis. First of all, a perinatal history related to hypoxia, infection, toxic-metabolic disorders is collected to resolve the issue of the etiology of DR, including information about the therapy and the effectiveness of rehabilitation. From the anamnestic information, special attention is paid to those that are characteristic of neonatal hypoxic encephalopathy, the consequences of which are DR: Apgar score less than 5 points, mechanical ventilation in the acute period for more than 2 days, pO2 less than 40 mm Hg, neonatal shock , convulsions in the acute period, including depression, coma. And also for some somatic symptoms - craniofacial anomalies (microcephaly, macrohydrocephaly), more than 3 stigmas, height and weight plateau, vomiting, lethargy, pigment abnormalities, angiomatoses, unusual odors. Lack of response to treatment allows one to suspect brain dysgynesia, gene or chromosomal syndrome; the progression of DR directs the diagnosis towards neurometabolic diseases. When examining a child, pay attention to the following neurological disorders: – limitation of range of motion of the limbs, disturbances in muscle tone, changes in the reflex sphere – primary neurological criteria; – disturbances of saccadic eye movements, gaze fixation, nystagmus; delay or absence of reduction of congenital cervical-tonic and labyrinthine-tonic reflexes by 2-3 months in full-term infants; delay in the verticalization program, chain reflexes to the head, trunk and limbs are secondary neurological criteria. Motor disorders can be represented by the following syndromes: • hypotonic – more common in premature infants, with multi-infarction brain damage. Transforms into spastic by 3–6 months. Another transformation option is into atonic-astatic syndrome (significant symmetrical limitation of range of motion in all extremities, low muscle tone, low reflexes, minimal motor skills, combination with a severe form of psychomotor development disorder); • spastic – decreased range of motion, muscle strength, increased muscle tone, hyperreflexia, foot clonus, contractures, synkinesis, often combined with dystonia; • dystonic – an increase in tone is associated with a change in body position, mainly a change from horizontal to vertical, which is associated with the pattern of cervical and labyrinthine tonic reflexes; combined with the manifestation of spastic syndrome; • hyperkinetic – athetosis and dystonia, which debut at 3–5 months, which is probably associated with myelination of the striatal system by the first half of life. In patients with “double athetosis” syndrome, hyperkinesis debuts in the first month of life; • waxy rigidity – muscle tone is increased according to the plastic type, active movements are slowed down, with passive movements the resistance is uniform, the return to the flexor position is slow, freezing in an unnatural position is observed. Occurs in patients with severe degrees of NGIE, decortication; • opisthotonus – increased muscle tone of a spastic type, manifested in a sharp extension of the back and neck; • cervical radicular syndrome – a characteristic symptom of cervical birth injury, manifested by stiffness of the neck muscles, sometimes with elevation of the shoulder girdle; • syndrome of “flexible child”, “flaccid child” – observed in patients with spinal amyotrophy, birth trauma, organic aciduria, cerebellar aplasia. The legs are completely spread, the arms are extended, there is no flexor reaction to traction by the arms, when suspended vertically and horizontally, the child’s head and limbs hang down; • benign motor phenomena – dystonic reaction of the feet to support during verticalization lasting up to 1–3 minutes with subsequent extension of the foot, flexor hypertonicity in the flexors of the elbow and knee joints for up to 3–4 months in full-term infants, benign paroxysmal dystonia (torticolis of the head or trunk). It is proposed to assess psychomotor development according to the calendar of critical periods (corresponds to the score of psychomotor development (PMR) by L.T. Zhurba, E.A. Mastyukova, 1985) in the 1st, 3rd, 6th, 9th and 12th months. The calendar method consists of determining the correspondence of the child’s chronological age (age at the time of examination) to the age standard of psychomotor skills. If the chronological age deviates from the calendar age by no more than 3 months, a mild degree of VMR impairment or VMR delay, or “tempo” delay is diagnosed (occurs in premature infants, with rickets; the outcome, as a rule, is a complete restoration of motor and mental functions, if there are no signs of brain damage according to neuroimaging data). A delay from calendar age of 3 to 6 months is recognized as a moderate violation of VUR, which determines the tactics of a detailed examination to find the cause of the disease. The average degree of PMR occurs in patients with NGIE with leukomalacia, stage II PVC, who have had meningitis, with epilepsy, gene syndromes, and brain dysgenesis. Severe degree of violation of PMR - developmental delay from the calendar for more than 6 months due to malformations of the brain (aplasia of the frontal lobes, cerebellum), HIE and PVC of the III degree, metabolic disorders of amino and organic acids, necrotizing encephalopathy, leukodystrophy, tuberous sclerosis, chromosomal and gene abnormalities, intrauterine encephalitis, congenital hypothyroidism. The given calendar (Table 1) presents the chronology of the reduction of cervical and labyrinthine tonic reflexes, on the one hand, and the program for the verticalization of chain righting reflexes to the head and torso, on the other. The calendar is built with an emphasis on important stages of motor and mental development. On the left side of the table are the standards for the head circumference and weight of the child, which allows the doctor not to miss information and timely screen small children with microcephaly for chromosomal and genetic syndromes, and in case of vomiting, exclude neurometabolic diseases: aminacidopathy, organic aciduria, mitochondrial and peroxicommic diseases. Instrumental and laboratory diagnostics 1. Neurophysiological methods: – electroencephalography with topographic mapping (EEGTC) allows you to trace the formation of age-related EEG rhythms. From 2 months, sleep spindles should appear and delta activity should disappear; – auditory evoked potentials (AEPs) are necessary to determine a child’s hearing based on an analysis of the conduction of the sound signal from the periphery to the temporal lobe cortex; – visual evoked potentials (VEPs) help assess the state of the visual analyzer from the optic nerve to the cortex; – electromyography and electroneuromyography (EMG) can detect a decrease in the speed of conduction along the nerves of the upper extremities (normally, up to 6 months of age, the speed in the arms is higher than in the legs), a decrease in the amplitude of oscillations in patients with atonic-astatic syndrome and severe spasticity [I.A. . Skvortsov, 2000]. 2. Neuroimaging - neurosonography (NSG) determines periventricular leukomalacia (PVL), subcortical necrosis, spina bifida. Computed tomography and magnetic resonance imaging are necessary to diagnose developmental anomalies of the frontal, temporal lobes, cerebellum, corpus callosum, and cerebrospinal fluid system. 3. Laboratory diagnostics are carried out for patients with impaired psychomotor development (lag behind the calendar by 3 or more months): - uremic amino acid test: for hyperalaninemia, histidinemia, phenylketonnuria, homocystinuria, glycinemia, organic acids, lactate-pyruvate, etc.; – tests for intrauterine infections, thyroid hormones, tests for leukodystrophies, mucopolysaccharidoses; – cytogenetic study, the indications for which are dysmorphia (3–5), mental retardation of unknown etiology, microcephaly in the absence of perinatal lesions, repeated stillbirths or deaths of newborns. Therapy of movement disorders and psychomotor development disorders Physiotherapeutic and drug treatment methods are most often used. Among physiotherapeutic methods, kinesitherapy has proven itself well. According to the Voight method, in patients with hemiparesis, movements in paretic limbs are reproduced daily for 6 hours for 21 days (the method was developed at the University of Alabama, Taub E., Ramey SL, DeLuca S., Echols K., 2004). Massage, therapeutic exercises, laser therapy (puncture technique for plexopathies), and a “dry” pool may also be recommended. Medications used include pyritinol (from the 3rd day of life, the dose is increased weekly by 1 ml or 20 mg to 5 ml or 100 mg for 2–3 months), Cerebrolysin 1.0–2.0 ml IM from the 4th week N 20, Actovegin 0.5–1.0 ml IM N 20. Combination of levodopa + carbidopa 0.05–0.1 mg/kg twice daily for 2–3 months, tolperisone 5 mg/kg twice daily, tizanidine in children over 6 months 1–2 mg/day. 2-fold dose, thermal procedures are used in the presence of rigidity and spasticity. Taking calcium hopantenate at a dose of 125–500 mg/day. 15 minutes after meals for 1–4 months with a repeat course after 3–6 months, including in the presence of athetoid movements. The drug penetrates well through the blood-brain barrier within an hour and has a positive effect on metabolic processes and blood circulation in the brain. Combines stimulating activity against various manifestations of cerebral insufficiency of exogenous organic origin with anticonvulsant properties. The drug leads to a decrease in motor excitability and has an activating effect on performance and mental activity. Calcium hopanthenate is also used in the treatment of speech development disorders, clonic stuttering, and urinary disorders. The drug has low toxicity and is usually well tolerated, is not metabolized and is excreted unchanged. The simultaneous use of other nootropic drugs is not recommended. Three-fold doses of clonazepam at a dose of up to 0.005–0.01 mg/kg are recommended in cases of athetosis and dystonia. For the treatment of opisthotonus, diphenine is prescribed up to 5 mg/kg per day. Therapy for organic aciduria also involves constant adherence to a low-protein diet, taking carnitine 100 mg per kg daily. Conclusion Movement disorders observed during the recovery period of more than 2–3 months should be considered persistent. Modern research methods make it possible to reduce the time of clinical observation before making a diagnosis of cerebral palsy. To do this, it is advisable to introduce psychomotor development scales at the level of regulatory documents of the Ministry of Health of the Russian Federation and organize modern diagnostic centers for movement disorders in infancy and early childhood on the basis of clinics at the rate of 1 center per 1 million population. Literature 1. Bondarenko E.S., Zykov V.P. Breast cancer, Perinatal hypoxic encephalopathy, 1999, No. 4 2. Zykov V.P., Shiretorova, D.Ch., Shadrin V.N., et al. Treatment of diseases of the nervous system in children. M.2003. 286 pp. 3. Zykov V.P., Shiretorova, D.Ch., Shadrin V.N., et al. Research methods in child neurology. M. 2004, 127 pp. 4. Palchik A.B. Evolutionary neurology. St. Petersburg., 2002, .383 p. 5. Register of medicines in Russia. M. 2005, 1440 pp. 6. Skvortsov I.A. Development of the nervous system in children. M. 2000, 200 pp. 7. Taskaeva T.V., Mikhnovich V.I., Dutova N.Ya. Treatment of cerebral palsy with L-dopa drugs. Issues of modern pediatrics. Appendix No. 3, 2004, p. 90 8. Pediatria. Taub E, Ramey SL, DeLuca S, Echols K 2004 ; 113(2):305–12. 9. L.–W. Wang, K.–M. Xu", H. Cai", C. Qian, J.–X. Wu", C.–H. Zhang, I. Matsumoto. Diagnoses and treatment of methylmalonic aciduria (MMA) J. Br & Dev, 2003.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues