When visiting a neurologist, more than 30% of patients present with somatic complaints that cannot be explained by any organic disease [1, 2].
Thus, the diagnosis of “tension headache” (TTH) ranks second in frequency among the 20 most common diagnoses established by a neurologist [3]
.
At a specialized otoneurological appointment, the diagnosis of “non-vestibular vertigo” takes second place after “benign paroxysmal positional vertigo” (BPPV) [4].
Suffice it to say that the prevalence of irritable bowel syndrome (IBS), according to various sources, reaches 10-20% in the population [5], the number of patients with functional disorders of the gastrointestinal tract (GIT) in a specialized gastroenterology hospital is about 45% [6] , and IBS - 23% [7] .
Similar data can be provided for other clinical functional syndromes, in particular chronic fatigue syndrome (CFS), hyperventilation syndrome, non-cardiac chest pain, intersitial cystitis, non-bacterial prostatitis, etc.
Below are the functional symptoms encountered at appointments with doctors of different specialties: gastroenterology - IBS, non-ulcer dyspepsia; rheumatology - fibromyalgia; cardiology - non-cardiac chest pain; pulmonology - hyperventilation syndrome; infectious diseases - CFS; neurology - tension-type headache, back pain, functional dizziness, psychogenic seizures, paresis, dysbasia, etc.; dentistry - atypical facial pain; ENT diseases - feeling of a “lump in the throat”; allergology - multiple chemical sensitivity (pseudoallergies); uro-gynecology - intersitial cystitis, non-bacterial prostatitis, chronic pelvic pain, premenstrual syndrome.
The clinical picture of the above diseases is dominated by chronic pain syndromes and various subjective sensations (dizziness, lack of air, fatigue, “lump in the throat”). Along with subjective symptoms, objectively recorded disorders are also detected (changes in the frequency and nature of stool, tachycardia, increases in blood pressure, changes in breathing patterns, swelling, signs of nonspecific immunity disorders, etc.). The predominance of functional symptoms is detected at the population level, at the general practitioner’s appointment and among patients referred for consultation to a specialist [8]. These patients are often prescribed various consultations, expensive studies and treatments, which, as a rule, do not lead to a positive result, causing dissatisfaction for both the patient and the doctor [9].
Terminology and classification
In domestic medicine, such disorders are most often referred to as “vegetative dystonia syndrome” (G-90.9, ICD-10) or “astheno-neurotic reactions” (F-48.0, R-53, ICD-10); in therapeutic practice the term “ neurocirculatory dystonia" (NCD) (F-45.3, ICD-10), in gastroenterology there is IBS (K-58, ICD-10). Some authors use the term “psychovegetative syndrome”, proposed in the 60s of the last century by German internists [10] .
In the practice of foreign colleagues, the terms SVD and NDC are practically not used today. As a rule, doctors prefer to use terms that denote specific clinical syndromes, for example, tension-type headache, “non-coronary pain”, “non-ulcer dyspepsia”, IBS, “hyperventilation syndrome”, CFS. Various terms have been used to denote this entire category of diseases: “somatoform”, “somatized” [11-13], “medically unexplained symptoms” ( eng.
.: medically unexplained symptoms) [14], “subjective health complaints” (
English
: subjective health complaints) [15].
However, these terms are not satisfactory, since most of them are based not on positive, but on negative criteria. Currently, terms with more positive content are proposed: “bodily distress syndrome” [
16, 17] and “dysfunctional syndromes” [18, 19].
Term «
functional diseases” was proposed back in the 80s of the last century [20].
The latest American Classification of Mental Illnesses, released in 2013, made significant changes to the Somatoform Disorders category, which was renamed Somatic Symptoms and Related Disorders. Officially to
refer to somatic and neurological symptoms. without an organic cause, the terms “functional somatic symptoms” (FSS) and “functional neurological symptoms” (FNS) were proposed. These changes are proposed to be used in preparing the next 11th version of the International Classification of Diseases (ICD-11). The advantage of the latter terms is their positive meaning. Firstly, the presence of any violations is emphasized, i.e. the validity of the patient’s complaints; secondly, the term is acceptable for the patient, since the term “unexplained” does not sound disturbing to the patient; thirdly, the role of the psychogenic factor, the existence of which is beyond doubt, is not emphasized, but is not recognized by the patient, and its mention usually causes internal resistance from the patient.
Not only changes in terminology are discussed, but also the movement of this category of diseases from the class of mental diseases to neurological ones. Very important are the DSM-5 comments for this class of diseases, which “recommend diagnosis in the presence of stressful somatic symptoms in response to which inappropriate thoughts, feelings and behavior arise” [21].
Thus, when diagnosing functional disorders, it is proposed not only to exclude an organic disease, but also to identify positive criteria, i.e., the patient’s erroneous ideas about the disease and its consequences, emotional reactions and changes in behavior in response to these stressful symptoms.
These patients are united into a single category of functional disorders by the presence of symptoms common to different functional disorders (comorbidity). Clinicians often observe suppression of symptoms characteristic of different functional diseases, sometimes simultaneously, sometimes sequentially [22]. Thus, patients with IBS or non-ulcer dyspepsia present complaints not only of a gastroenterological nature. Upon detailed questioning, they reveal symptoms characteristic of CFS, complaints of chest pain of non-cardiac origin, and allergies of unknown etiology. CFS can be combined with manifestations of fibromyalgia [23], premenstrual tension and headache of unknown etiology. Of the 12 patients with functional syndromes, 8 complained of bloating, 8 of constant headache, 6 of abdominal pain, 6 of chronic fatigue [24]. From 2 to 25 non-gastroenterological symptoms occur per patient in 84% of patients with IBS, while associated symptoms most often manifest themselves as pain in different parts of the body [25, 26]. In almost 80%, IBS symptoms are combined with functional disorders in the urological area [27 ], and in 35-44% - with pelvic pain [25, 28]. These facts show that the specificity of these syndromes is blurred by many repetitions of common symptoms [24]. All these data support the assumption that patients with one functional syndrome meet criteria for other functional diseases. It is no coincidence that questions arise about the uniqueness of each individual syndrome and about the possibility of forming a clinical picture of the disease from a group of syndromes [24].
According to a number of studies, in ¾ of patients with IBS, symptoms persisted for 10 years or more after their identification, which led to significant costs for repeated examinations and treatment [29]. Similar data were obtained for functional neurological disorders. Thus, after 12 years, FNS persisted in 83% of patients, and other FNS and FSS also appeared; the majority of these patients continued to remain in distress, were disabled and in need of medical care [30].
Clinical analysis of large samples of patients with CFS [31],
fibromyalgia [32], IBS [33, 34], and non-ulcer dyspepsia [35] showed that these syndromes are significantly more common in women. Thus, the ratio of women to men with IBS is 2-2.5:1 [36], and among patients visiting specialized medical institutions, it reaches 5:1 [37]. The ratio of women to men observed in a specialized gastroenterological institution with IBS is 2.5:1 [38]. These data allow us to discuss the role of sex hormones in the pathogenesis of functional disorders in different systems.
In the vast majority of patients with functional disorders, evidence of abuse in childhood, mental, physical or sexual violence in the family can be identified. These situations are considered as extreme stress, leading to the development of post-traumatic stress syndrome (PTSD) with irreversible changes in the central nervous system, neuroendocrine and immune regulation [39-41]. It is believed that it is these disorders that subsequently play a significant, if not leading role in the formation and chronicization of functional disorders.
It has been shown that not only violence, but also a number of factors that disrupt the quality of interaction between people providing primary care for a child during the first 18 years of life (including serious maternal illness, marital discord, divorce) can have an equally detrimental effect on predisposition of an adult to diseases [42]. Data on the role of psychosocial factors in the onset, chronicity and exacerbation of IBS symptoms are extensive [43]. Childhood sexual abuse was more often detected in the anamnesis of patients with CFS, as well as in patients with functional gastrointestinal diseases in comparison with organic ones [44, 45]. In women with chronic pelvic pain, a history of abuse led to hypocortisolemia and disturbances in its fluctuations in the concentration of cortisol in the blood, which was not observed in healthy women [46]. Patients with FNS reported a higher frequency of physical and sexual abuse compared to patients suffering from affective disorders. [47].
The important role of personality traits and emotional disorders in the genesis of functional diseases, their course and response to therapy has been revealed. A number of studies using standard personality questionnaires have shown a significant predominance compared to controls of such personality traits as neuroticism, introversion, isolation, anxiety, depression, as well as personality disorders of obsessive-compulsive, paranoid, schizoid and avoidant types in patients with CFS, psychogenic dizziness , IBS [48-50]. These patients are more often diagnosed with chronic anxiety, depressive and somatoform disorders.
Traditionally, this category of patients is prescribed standard therapy, which is symptomatic in nature: patients with tension-type headaches receive painkillers; for functional gastrointestinal diseases, proton pump inhibitors, H2 receptor blockers, antidiarrheals or laxatives are prescribed; for chronic non-vestibular vertigo - betahistines, etc. Standard symptomatic therapy or so-called on-demand therapy is generally ineffective in the long term. Its results are short-term and often minimal. Thus, patients with IBS follow a diet for years, take antispasmodics, prokinetics, antidiarrheal drugs or laxatives, but their effectiveness is short-lived and concerns only individual symptoms. Patients with tension-type headache take analgesics for a long time (often in large doses) and at the same time note that they do not relieve the headache. Moreover, long-term use of analgesics leads to the development of abuse, which in turn contributes to the chronicity of headaches.
The effectiveness of multimodal therapy
Numerous multicenter placebo-controlled studies have shown that the most effective in the treatment of all functional disorders are information and educational programs [51], cognitive behavioral psychotherapy, physical therapy rehabilitation, including dosed physical activity and the use of antidepressants. The effectiveness of these methods has been shown for CFS [52], functional vertigo [4], fibromyalgia [53], IBS [54], and FNS [55].
The key concepts in the treatment of patients with functional disorders are psychological involvement in the therapy process with awareness and acceptance of one’s own thoughts, feelings and condition without criticism and condemnation. In this context, the English-language literature uses the term “mindfulness” - “non-judgmental awareness”. The purpose of this line of therapy is cognitive regulation of the perception of symptoms [56].
It is known that the basic drugs for the treatment of chronic pain syndromes of various localizations are antidepressants (AD) [57]. They are effective whether chronic pain is combined with depression or not. ADs turned out to be effective not only for the treatment of emotional disorders and pain, but also for such disorders as tachycardia, dyspnea, frequency and character of stool, postural phobic dizziness, etc. [58-60]. Thus, in a 16-week prospective study of the effectiveness of sertraline in patients with chronic subjective dizziness, it was shown that at a dose of 25–200 mg/day (average dose 100 mg/day), the drug caused more than 50% reduction in dizziness in 73% of patients, and 40% have complete remission [59].
Diagnostics and treatment in our clinic
An experienced neurologist at our clinic will analyze the patient’s complaints and perform a detailed examination. Diagnosis of central nervous system diseases necessarily includes an assessment of the patient’s consciousness, his reflexes, intelligence, etc.
Some diseases are easy to identify by their symptomatic manifestations, but, as a rule, an accurate diagnosis is only possible based on the results of additional studies. In our practice, we use the most modern diagnostic equipment, which allows us to conduct such high-precision studies as:
- computed tomography of the brain;
- ultrasound examinations;
- angiography;
- electroencephalography;
- radiography;
- electromyography;
- lumbar puncture, etc.
Treatment of each disorder of the central nervous system requires a strictly individual and careful approach. The doctor selects therapy, but it should be understood that some disorders are not reversible, so treatment can be purely supportive and symptomatic.
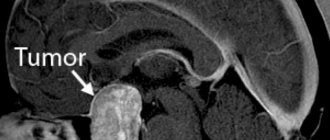
The main method of treating diseases of the central nervous system is medication, but physiotherapeutic procedures, therapeutic exercises and massage also have a good effect. Surgical treatment may be indicated when cysts and tumors are detected. As a rule, all operations are performed using modern microsurgical techniques.