Article:
Dysarthria is a complex speech disorder, one of its most common forms is bulbar.
The word “dysarthria” itself comes from the Greek “dys” - “disorder” and “arthroo” - “pronounce clearly”. Bulbar dysarthria manifests itself as slurred, slurred speech with a dull nasal tone. A child with this disorder speaks as if he has porridge in his mouth. A similar disorder occurs due to damage to the speech apparatus of the CNS (central nervous system). The first detailed description of dysarthria appeared more than a century ago. It was compiled by A. Oppenheim and H. Gutzmann. This disorder was studied in more detail in 1888 by A. Kussmaul.
What is bulbar dysarthria
Bulbar dysarthria is a person’s loss of articulate expressive speech caused by a disorder of the articulation apparatus by damage to the cranial nerves (IX, X, XII pairs). The clinical picture of this disorder is as follows:
- slurred speech;
- slow pace (braking);
- monotone;
- paucity of speech;
- dysphonia;
- the swallowing reflex is impaired.
The bulbar type of dysarthria can be established after speech therapy and neurological examination. To identify it, a number of examinations must be carried out - MRI, CT, cerebrospinal fluid analysis and others. The clinical picture of bulbar dysarthria depends on the lesion.
Prevention
Prevention of this disorder consists of preventing serious illnesses that can cause paralysis.
Prevention of pseudobulbar syndrome includes the identification and treatment of cerebral atherosclerosis and the prevention of strokes.
It is necessary to adhere to a work-rest regime, limit caloric intake, reduce the consumption of animal proteins and foods with cholesterol. There is no specific prevention.
It is very important to immediately contact a specialist who will not only select the correct treatment, but also help reduce the manifestations of the disorder in order to improve the patient’s quality of life.
Reasons for the development of the disease
The main cause is damage to the bulbar nerves. If we consider from the point of view of anatomy, the glossopharyngeal nerve connects to the muscles of the pharynx, the vagus nerve to the palatine nerve, the hypoglossal nerve approaches the lingual muscle. Damage occurs precisely to these nerves. Experts identify the following causes of bulbar dysarthria:
| № | Factors of speech impairment | Manifestations |
| 1 | Perinatal factors | Complications during pregnancy, childbirth (improper position of the fetus, gestosis, premature birth, placental abruption, trauma during childbirth) |
| 2 | Head injuries | Bulbar dysarthria can develop due to traumatic brain injury of varying severity |
| 3 | Neoplasms in the brain | The growth of tumors in the brain disrupts the normal functioning of its parts. When localized in the speech department, compression of the bulbar structures occurs. Such tumors can be gliomas, medulloblastomas, benign formations |
| 4 | Neuroinfections | The most common of them are meningoencephalitis, viral encephalitis and others. The infection provokes inflammation and compression of the cranial nerve nuclei |
| 5 | Neurodegenerative processes | Destruction of the cranial nerve nuclei occurs |
| 6 | Encephalopathy and angiopathy | Occurs in somatic diseases (diabetes mellitus, abnormalities of cerebral vessels). As a result of such disorders, the blood circulation in the brain is destabilized. |
Before starting corrective work with bulbar dysarthria, it is necessary to accurately determine the cause of its occurrence. Without eliminating the cause, it is impossible to achieve complete restoration of speech and speech apparatus. Rehabilitation and reasons should be prescribed exclusively by specialized specialists in the field of speech therapy and neurology.
Possible complications
Speech impairments make it difficult, and in some cases completely eliminate, communication with other people. Understanding the presence of a problem with articulation, the inability to convey information to others negatively affects overall mental health, and can also lead to neurotic disorders such as neurasthenia, depression and others. With dysarthria, difficulty eating is often observed. A person often chokes on food and water, which can lead to asphyxia or aspiration pneumonia.
Children suffering from pseudobulbar dysarthria often experience general speech underdevelopment (GSD), which in turn is dangerous due to dyslexia and dysgraphia. Children with a mild form may encounter problems at school (communicating with teachers and classmates). Children with moderate and severe forms are trained in specialized schools. If correctional work is not carried out with the child on time, there is a likely risk of developing intellectual disability and general mental retardation.
Symptoms
The main symptoms of bulbar dysarthria:
- The child's speech is slurred, inhibited, with poor articulation. The “R” sounds are replaced with fricative ones. Instead of the sound “B”, the sound “P” is pronounced “V”, the sound “P” changes to “F”.
- Consonant voiced sounds are completely or partially absent. Unstressed and stressed sounds are pronounced the same. The letter "A" sounds best.
- There is a noticeable rhythm disturbance. Speech sounds less emotional and monotonous. Expressive speech is not available to a child with dysarthria.
- The child often chokes and has problems swallowing when eating food and water.
- The child's voice is low and nasal.
- Facial expressions are poorly expressed, facial asymmetry is observed (with unilateral nerve damage).
A child suffering from this type of dysarthria has simple slurred articulation. In some cases, voiced sounds disappear from speech. The deaf begin to dominate them. Speech loses its expressiveness and emotionality; it is not melodic. Expressive speech causes great difficulty for the patient and quickly tires him.
The exact symptoms depend on which cranial nerves are affected. In some cases, all of these symptoms may occur.
Goals of therapy
Currently, there are no effective treatments for this disease. Therefore, therapy is aimed at:
- slow down the progression of the disease and prolong the period of illness during which the patient does not need constant outside care;
- reduce the severity of individual symptoms of the disease and maintain a stable level of quality of life.
Diagnosis of bulbar dysarthria
Diagnosis of bulbar dysarthria should be carried out only by specialists. To do this, it is necessary to conduct a number of specialized studies:
- Neurological examination. It allows you to determine the location of lesions of the cranial nerves. The doctor must assess the existing pathological process and its severity, as well as determine the causes of their occurrence.
- Speech therapy examination. The specialist evaluates the rhythm of speech and its speed, voice, mobility of the articulatory apparatus, and breathing rhythm during speech. Based on these data, the speech therapist chooses treatment tactics.
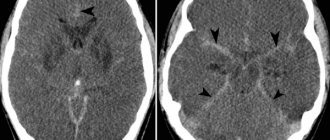
- CT studies, electroencephalography, ultrasound, MRI of the brain. It is necessary to obtain complete information about the pathology, the type of disorders, and on their basis decide on a correction program.
- Lumbar puncture. Necessary for identifying and identifying infectious pathogens.
The doctor may refer the child for additional tests and schedule consultations with other specialists. It may also be necessary to monitor the patient's health over time. Repeated studies may be required during the correction of dysarthria.
Also, the specialist must accurately distinguish the manifestations of bulbar dysarthria from pseudobulbar. The reason for the development of the second is damage to the corticobulbar nerves. To develop rehabilitation, it is necessary to exclude motor, dynamic and acoustic-mnestic aphasia from suspicion of diagnosis.
Forms of pseudobulbar dysarthria
There are three forms of this type of dysarthria:
- spastic (spasmodic);
- paretic;
- mixed (that is, spastic-paratic).
Each of these forms has its own symptoms and treatment features.
Spastic form of pseudobulbar dysarthria
This form of pseudobulbar dysarthria is characterized by tension of the respiratory muscles or hyperkinesia of the larynx, spastic paresis of the lingual muscle, tension of the labial muscles and impaired tone of the palate.
Such manifestations make speech more monotonous, with a nasal tone. It is difficult for a child to maintain articulatory postures, there are difficulties in switching them, and the breathing process may take a long time, which leads to problems in voice formation (articulation). With pseudobulbar dysarthria, the following characteristic phenomena are observed:
- silent articulation;
- there is no prolonged rest of the speech muscles;
- spasms of the labial muscles;
- tension when smiling;
- limited tongue movements;
- disturbances in sucking and swallowing movements are observed;
Often in children with this disorder, the first cry is absent, and breathing is pronouncedly weak and arrhythmic, there is a weak short exhalation, and speech occurs while inhaling. This species is also characterized by the presence of speech phonations, a weak, quiet voice, the rate of speech is fast, but its rhythm is not maintained. In other words, someone who has a spastic form of pseudobulbar dysarthria speaks from spasm to spasm, which leads to the use of short phrases with poor intelligibility, depending on the strength of the voice. At the same time, the meaning of what was said does not suffer.
Paretic form of pseudobulbar dysarthria
This form is observed with hypotonia of the speech and skeletal muscles. The child has pareticity of the tongue, lips, and palate. There is difficulty in switching articulatory postures, asynchrony in breathing and articulatory movements. Often such a child may have increased salivation (salivation).
The inhalation during conversation is short and inadequate, and the exhalation is also weak. The voice itself is loud, ringing, but quickly fading. Speech in this case has a nasal pronunciation, weak and quiet. Some isolated sounds are completely preserved, but in the speech stream they are blurred. Eating is at a disturbed pace and there are difficulties in coordinating chewing movements.
Mixed form
This form is the most common. In the scientific literature it is called spastic-paretic syndrome. With it, there is hypertonicity of one muscle group, for example, the muscles of the lips and cheeks, while the tongue has reduced tone.
Treatment of bulbar dysarthria
Treatment of bulbar dysarthria has better results with parallel rehabilitation measures. A variety of specialists should take part in this work, depending on the causes and severity of the speech disorder. Corrective work consists of several components:
- Etiopathogenetic treatment. It is carried out if dysarthria is caused by infectious diseases. If tumors are present, a special treatment plan is developed together with neurosurgeons.
- Neurometabolic correction. This treatment is aimed at restoring the functioning of cerebral neurons and fibers.
- Speech therapy classes. Aimed at establishing correct sound pronunciation and subsequent automation. Special speech therapy exercises and breathing exercises are used. At later stages, the rhythm of speech and its expressiveness are corrected.
- Rehabilitation therapy. Restores motor skills and psycho-emotionality of the child. This is necessary for proper social adaptation. This work is carried out jointly with a psychologist and psychotherapist.
Motor Neuron Disease: Types
Motor neuron disease has ICD-10 code G12: Spinal muscular atrophy and related syndromes. It belongs to a group of neurological diseases in which motor neurons are damaged. Synonyms: Lou Gehrig's disease, Charcot's disease. In many countries, it is customary to use the term “amyotrophic lateral sclerosis” (ALS) to refer to motor neuron disease, as the most common pathology in this group. This also includes:
- hereditary spastic paraplegia;
- primary lateral sclerosis;
- progressive muscle atrophy;
- motor neuron disease, bulbar form;
- pseudobulbar palsy;
- primary lateral sclerosis.
The disease is characterized by degeneration of motor neurons in the cerebral cortex, brain stem, corticospinal tracts and spinal cord. The result is progressive muscle paralysis.
The disease is rare. Its prevalence is approximately 2-3 people per 100 thousand per year. Most often, the disease occurs in people aged 60-70 years, although it is possible that the pathology may develop in people under 40 years of age.
Reanimatology School of Professor Sergei Vasilievich Tsarenko
Bulbar and pseudobulbar disorders
The most common cause of respiratory failure is damage to the lower parts of the brain stem with loss of functions of the so-called bulbar group of cranial nerves - IX, X and XII pairs. The functions of these nerves are disrupted when their nuclei are directly damaged or when the controlling influence of the overlying supranuclear cortical neurons is lost. With nuclear lesions, bulbar disorders develop, with supranuclear lesions, pseudobulbar disorders develop. Pseudobulbar disorders always occur when the level of consciousness decreases to stupor and coma. Both bulbar and pseudobulbar disorders lead to a decrease in the tone of the muscles of the tongue and pharynx and to swallowing disorders. Obstruction of the upper respiratory tract develops, a violation of the cough mechanism, as well as aspiration of the contents of the oropharynx and nasopharynx into the trachea and bronchi.
Up to a certain point, these pathological mechanisms may not have pronounced clinical manifestations. However, even a slight retraction of the tongue leads to episodes of hypoxia and hypoxemia, which gradually worsen the condition of the affected brain. In addition, even a small aspiration of saliva and food causes the subsequent development of inflammatory changes in the lungs.
Increased cerebral ischemia and intracranial hypertension
With cerebral ischemia, acidosis of brain tissue develops with a compensatory increase in breathing and respiratory alkalosis. The cause of hyperventilation is also an increase in intracranial pressure due to an increase in the volume of the brain, cerebrospinal fluid or blood. At the same time, due to dislocation, the functions of the diencephalic structures, which are the command post for the respiratory center, are disrupted. One of the typical signs of the diencephalic stage of transtentorial herniation is hyperventilation.
Respiratory center damage
Contrary to popular belief, direct damage to the respiratory center is not very common. Neurons of the respiratory center are located in the lower (bulbar) parts of the brainstem and are rarely damaged from the very beginning of TBI. The usual sequence of events is as follows: with supratentorial lesions (that is, localized in the anterior and middle cranial fossae), a comatose state first occurs, and only in the later stages of brain dislocation, when the brain is wedged into the foramen magnum, breathing disorders develop. As a rule, damage to the respiratory center in these cases is combined with hypotension due to simultaneous damage to the vasomotor center. At these stages it is no longer possible to save the patient.
The doctor's close attention requires damage to the respiratory center when the pathological process is localized in the posterior cranial fossa (that is, subtentorial). In this case, there is no usual sequence: first the appearance of depression of consciousness, then breathing disorders. Life-threatening respiratory distress can occur with a slight decrease in the level of wakefulness, for example, to the point of mild stupor. The process of dislocation spreads “from the bottom up”, so first breathing disorders such as hypopnea or even apnea develop, as well as hemodynamic disorders, and only then does deep depression of consciousness occur when the upper parts of the trunk are affected.
Excessive strain on the non-respiratory functions of the lungs
Brain damage, like any resuscitation pathology, is accompanied by disruption of the non-respiratory functions of the lungs. This is due to the fact that the lungs, along with the kidneys, liver and gastrointestinal tract, are an excretory organ. They act as a filter that retains a lot of biologically active substances (serotonin, histamine, prostaglandins), platelet agglomerates, red blood cell fragments, etc. The retained substances and cells are then excreted in the sputum using the coordinated movements of the cilia of the airway epithelium (mucociliary transport). During a resuscitation situation, the development of hypovolemia, disseminated intravascular coagulation syndrome, overproduction of biologically active substances, the amount of sputum increases tens and hundreds of times. Mucociliary mechanisms, damaged due to hypovolemic disorders and ischemia of the lung tissue, cannot cope with the removal of increased amounts of sputum. The cough reflex becomes less effective due to neurological impairment. As a result, sputum retention in the lungs occurs, it becomes infected and the development of inflammatory changes in the form of tracheobronchitis and pneumonia. Purulent-inflammatory complications cause the development of respiratory failure due to damage to the lung parenchyma. In this case, the supply of oxygen to the body is disrupted, and secondary cerebral ischemia occurs.
Filling the alveoli with sputum leads to their exclusion from gas exchange. Blood that continues to flow to the unventilated alveoli is not oxygenated. It enters the pulmonary veins and then into the systemic circulation with low oxygen levels and high levels of carbon dioxide. This process is called shunting of blood in the lungs due to a violation of the ventilation-perfusion relationship. With a large amount of shunted blood, there is a risk of arterial hypoxemia and hypercapnia. In response, two defense mechanisms are activated.
First, the removal of carbon dioxide from the alveoli is increased with normal ventilation-perfusion relationships. This is possible due to the linear nature of the carbon dioxide dissociation curve. It is impossible to increase arterial oxygenation in the same way due to the nonlinear S-shaped nature of the oxyhemoglobin dissociation curve.
A little physiology The relationship between the saturation (saturation) of hemoglobin with oxygen (SO2) and oxygen tension (pO2) in the blood is S-shaped (Fig. 3.16). This means that as pO2 increases, SO2 increases, but not indefinitely. At a certain pO2 value (on average 80-90 mm Hg), all hemoglobin is combined (associated) with oxygen. In other words, hemoglobin saturation reaches almost 100% and no longer increases. When pO2 decreases, the connection between oxyhemoglobin and oxygen is disrupted - oxyhemoglobin dissociates and turns into reduced hemoglobin. The curve described is called the oxyhemoglobin dissociation curve. The curve of the dependence of the volumetric oxygen content in the blood on its voltage has a similar shape. It is called the oxygen saturation curve.
The relationship between the volumetric content of carbon dioxide in the blood and the tension of carbon dioxide physically dissolved in the blood (pCO2), in contrast to the above-mentioned curves, is almost linear (Fig. 3.17). This means that the higher the pCO2 voltage, the higher the CO2 content in the blood. An increase in carbon dioxide tension leads to an increase in the formation of carbonic acid (H2CO3) and bicarbonate. This process is practically unlimited. The described dependence is called the carbon dioxide dissociation curve, by analogy with the dissociation curve of oxyhemoglobin. However, this familiar term, strictly speaking, is incorrect and creates confusion, since CO2 does not dissociate into anything. Probably more logical is the term CO2 saturation curve proposed by a number of authors. Understanding these limitations and conventions, we still prefer to use the traditional term.
Due to the linearity of the carbon dioxide dissociation curve, the removal of CO2 through the alveoli, in which ventilation and blood flow are maintained, is not limited in any way. Increased CO2 removal through these well-functioning alveoli leads to a decrease in carbon dioxide levels in the blood. This process over time can compensate for insufficient CO2 removal from alveoli with poor ventilation-perfusion relationships.
With compensation for the lack of oxygen supply, the situation is more complicated. In alveoli with good ventilation-perfusion ratios, hemoglobin is already almost 100% saturated with oxygen. It can no longer add additional oxygen. In this regard, an increase in oxygen tension in these alveoli does not ensure the addition of additional amounts of oxygen to hemoglobin and cannot compensate for the insufficient saturation of hemoglobin in alveoli with poor ventilation-perfusion relationships.
The second protective mechanism during pulmonary shunting is compensatory pulmonary vasoconstriction. Those vessels that are directed to the unventilated alveoli narrow and practically do not participate in the exchange of oxygen and carbon dioxide. This limits the admixture of venous non-arterialized blood, depleted of oxygen and supersaturated with carbon dioxide, to arterial blood coming from normally ventilated and perfused alveoli. This vasoconstriction may be excessive, for example in respiratory distress syndrome. A number of drugs with vasodilating properties (for example, nitrates) can neutralize the effect of this protective mechanism and thereby increase hypoxemia.
Infection
Sputum filling the alveoli is an excellent breeding ground for microorganisms that enter there in two ways - through the blood and through the respiratory tract. The second path is the main one. Due to bulbar disorders, the contents of the oropharynx flow into the trachea and bronchi. It contains both its own microflora and microorganisms from the intestines that enter the stomach and esophagus due to impaired peristalsis, the presence of antiperistalsis and poor functioning of the sphincters. An important source of infection is the aerogenic introduction of microorganisms from the surrounding hospital environment, through the hands of personnel and insufficiently sterile circuits of breathing equipment.
Infection of sputum repeatedly increases its quantity, which is another factor in the deterioration of ventilation-perfusion relationships, and also causes an increase in the concentration of inflammatory mediators in the lung tissue and increases its damage.
Iatrogenic damage
In contrast to general resuscitation views, in neuroresuscitation, artificial and assisted pulmonary ventilation are considered not only as methods of prosthetics for impaired lung functions. In case of TBI, these methods are therapeutic, since only they are able to provide an effective supply of oxygen necessary to relieve hypoxic damage to the affected brain.
We conducted special studies assessing the dynamics of the neurological status of patients, as well as using methods of non-invasive assessment of brain oxygenation (cerebral oximetry), during which we were able to establish the following facts. One of the most effective ways to increase the level of wakefulness and reduce focal and dislocation disorders, as well as restore oxygenation of the affected brain, was to increase the oxygen saturation of the inhaled oxygen-air mixture. Oxygenation through nasal catheters made it possible to increase the oxygen tension in the blood to 100-110 mm Hg, through a face mask - to 120-130 mm Hg. This ensured complete (almost 100%) saturation of arterial blood hemoglobin with oxygen, but was not sufficient to achieve normal oxygenation of cerebral venous blood (55-75%) in more than half of the patients examined.
We found that to ensure the required level of brain oxygenation in the acute period of injury in the majority of comatose patients, it was necessary to perform mechanical ventilation with an increase in the oxygen content in the respiratory mixture to 40%. In a number of clinical situations, only 100% oxygen was the only therapeutic agent that could urgently increase brain oxygenation. It was possible to stop brain hypoxia only when the oxygen tension in arterial blood (paO2) increased to more than 150-200 mmHg.
It is difficult to explain these data from the usual positions of oxygen transport.
A little physiology According to the classical formula, the amount of oxygen brought by the blood to the tissues is determined as follows:
DO2= CO × (1.34 × SatO2 × Hb + 0.003 × paO2)
where DO2 is oxygen delivery, CO (cardiac output) is cardiac output, 1.34 is Hüffner’s constant, SatO2 is the saturation of hemoglobin with oxygen, expressed as a percentage, Hb is the amount of hemoglobin in g/l, paO2 is the oxygen tension in arterial blood in mm Hg
According to this formula, only oxygen bound to hemoglobin is of fundamental importance for oxygen delivery. Oxygen dissolved in blood plasma has a much lower value, which is reflected by the introduction of a coefficient of 0.003. From this point of view, there is no point in increasing pO2 in arterial blood more than 100 mmHg. Due to the S-shaped nature of the oxyhemoglobin dissociation curve, even at this level, hemoglobin is almost completely saturated with oxygen.
In our studies, normal paO2 levels are 80-100 mmHg. and hemoglobin oxygen saturation of 96-98% were not sufficient to relieve the reduced oxygenation of brain tissue. Normalization of cerebral oxygenation was observed only at high levels of oxygen dissolved in the blood. A possible explanation for this fact is the hypothesis of extrahemoglobin oxygen delivery. It was put forward by researchers who conducted intravital observations of cerebral blood flow in an experiment through a plastic window implanted into the skull. It was found that almost 20% of cerebral vessels do not contain red blood cells (W. Kuschinsky, OB Paulson, 1992). Consequently, there is no hemoglobin in these vessels, and the only source of oxygen for the tissues supplied by them may be oxygen dissolved in the plasma.
The positive effects of hyperbaric oxygenation (HBOT) on cerebral oxygenation are probably based on the same effects. The development of this promising method is hampered by a paradoxical fact: the more severe the patient’s condition, the greater the benefit of HBOT and the more dangerous it is to place the patient in a conventional pressure chamber that is not equipped with prosthetic breathing devices. Perhaps the problem will be resolved by the use of special resuscitation pressure chambers equipped with ventilators. Based on the conducted studies and clinical observations of neurological symptoms and instrumental data, we believe that the indication for artificial and assisted pulmonary ventilation (AVL) for brain damage is not only obvious respiratory failure, but also an increase in neurological disorders.
However, respiratory support methods are aggressive means of intensive care. They can carry significant negative potential due to the risk of iatrogenic lung injury (Fig. 3.18). Modern work on the effect of mechanical ventilation on lung tissue (VM Ranieri et al., 1998) has shown that the injection of large volumes of gas into the lungs under high pressure leads to damage to the alveoli, the entry of air into the interalveolar and intertissue spaces, as well as into the pleural cavities. Developing interstitial emphysema, pneumomediastimum and pneumothorax are manifestations of baro- and volumotrauma of the lungs. They create the potential for micro- and macroactualization of the lungs. Significant forces stretching the lungs during artificial inspiration cause biotrauma of the lungs due to the release of cytokines, prostaglandins, kinins and other inflammatory mediators by alveolocytes (PM Suter, B. Ricou, 1998).
It has been established that if, during mechanical ventilation, the pressure in the alveoli at the end of exhalation decreases to zero, this causes collapse (sticking together) of the alveoli, therefore, during the subsequent inhalation, significant pressure is required to open (unstick) the collapsed alveoli (AS Slutsky, 1993). These cycles of sticking and unsticking have an extremely negative impact on the structure of the alveoli. Another mechanism of adhesion and atelectasis of the lungs is the same mechanical breaths. They can lead to uneven ventilation of the lungs, which causes overdistension of some areas and insufficient expansion of others. Normally, this is prevented by different depths of spontaneous breaths. When high concentrations of oxygen are used, the neutral gas nitrogen is replaced in the alveoli by oxygen. Nitrogen does not participate in gas exchange processes and only fills the alveoli, preventing them from collapsing. Oxygen is absorbed, which leads to the collapse of the alveoli and the formation of so-called absorption atelectasis.
All of the listed mechanisms of atelectasis are called atelectotrauma. This injury is dangerous to the lungs due to the development of irreversible changes in airless areas. Then an infection sets in, and pneumonic foci form. The passage of blood through airless areas leads to disruption of ventilation-perfusion relationships and an increase in shunting processes.
Damage to the alveoli by hyperoxic mixtures, as well as significant tensile loads, also causes a disruption in the production of surfactant, a protein that maintains the alveoli in a stretched (airy) state. Lack of surfactant leads to irreversible collapse of the alveoli.
Iatrogenic damage to the lungs includes overhydration, including due to the use of proteins and colloids. According to some researchers, infusion therapy with these drugs may make an additional contribution to the impairment of non-respiratory lung functions (HF Ginz et al., 1998). Proteins and colloids accumulate in the interstitial space of parenchymal organs, including the lungs. Their stretchability and pliability decreases. For the development of pulmonary hyperhydration, not only the qualitative, but also the quantitative composition of the administered fluid is important. Currently, there is evidence of the need to limit fluid load and use diuretics in pulmonary lesions, in particular in ARDS (RJ Mangialalargi and GR Bernard, 1998).
Another iatrogenic mechanism for pulmonary injury may be antiperistalsis due to the use of gastric tubes during enteral nutrition.
Metabolic disorders
Metabolic disorders in TBI may be important in patients with so-called “difficult weaning from a respirator,” that is, in patients who have been on mechanical ventilation for a long time. The most common cause of weakness of the respiratory muscles is hypokalemia, which causes conduction disturbances at neuromuscular junctions. In addition, excessive enteral and infusion support with glucose-containing mixtures causes excessive accumulation of carbon dioxide and increased demands on the respiratory system for its removal. For unknown reasons, long-term use of muscle relaxants may cause weakness of the respiratory muscles. Perhaps there is rhabdomyolysis provoked by these drugs or a decrease in the activity of enzymes that destroy muscle relaxants.
Embolism of vessels of the pulmonary circulation.
Embolism of the vessels of the small circle during TBI occurs due to the entry into the arterioles and capillaries of the small circle of blood clots from the veins of the legs and pelvis, as well as fat emboli from damaged bones and muscles of the lower extremities. The sudden occlusion of a large volume of pulmonary vessels leads to spasm of the pulmonary capillaries, the development of acute overload of the right ventricle and acute failure of filling of the left ventricle. This situation causes heart rhythm disturbances, even cardiac arrest.
If the patient experiences an acute episode on his own, or the heart rate and breathing are restored after resuscitation measures, then pulmonary infarctions develop, which after a few days turn into areas of infarction-pneumonia.
Much less often events develop according to a different scenario. The patient's shortness of breath gradually increases, but according to the chest x-ray, the lung fields remain clear. The cause of this condition is increasing thrombosis of the pulmonary artery. Areas of infarction-pneumonia do not form, and an accurate diagnosis can be made only after angiopulmonography or spiral CT of the chest. ‹ 3.4. Acute respiratory failure.Up3.4.2. Main syndromes of respiratory disorders. ›