Causes of vascular headache development
Vegetative-vascular dystonia is an outdated name for autonomic dysfunction of the cardiovascular system. VSD is characterized by more than 150 symptoms, the most common of which is vascular headache.
The causes of headaches are:
- decreased tone of the blood vessels supplying the brain, which causes hypoxia (usually occurs with a systematic increase in pressure, which stretches the walls of blood vessels),
- pressure on nerve bundles specifically at the moment of a pressure surge (expansion of the walls of blood vessels),
- venous congestion and cerebral edema,
- arterial spasm.
Types of strokes
Depending on which part of the brain the hemorrhage occurred, there are 4 types of stroke:
- Intracerebral or parenchymal, when the spilled blood saturates an area of the brain. In turn, they also have their division into:
- hemispheric, when an area of the hemispheres is affected;
- subcortical, located under the cortical (gray) matter of the brain;
- hemorrhage in the cerebellum, where the balance centers are located;
- hemorrhage in the brain stem, where the respiratory center and the area that is responsible for the functioning of the heart and maintaining the pressure in the vessels necessary to support life are located.
- Subarachnoid (bleeding into the space between the meninges).
- Ventricular (hemorrhage into the ventricle of the brain).
- Mixed: ventricular-parenchymal, subarachnoid-parenchymal, parenchymal-ventricular-subarachnoid and so on.
Survival depends not only on the location of the vessel rupture, but also on how much blood was released. Small hemorrhages are considered to be those in which from 1 to 20 ml are poured out, medium - from 20 to 50 ml, large - more than 50 ml. The greater the amount of blood shed, the more severe the consequences. A stroke is almost always accompanied by disturbances in cardiac activity, breathing and swallowing, oculomotor disturbances, and changes in the size of the pupils.
Symptoms of headache with vegetative-vascular dystonia
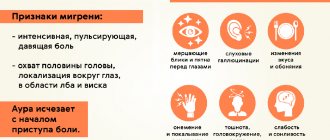
The symptoms of vascular headaches are very diverse, but the main difference from other types of pain is less intensity, rather “background” pain, but painful attacks, for example, migraines, can also occur.
- Headache with VSD accompanies a person constantly with varying intensity. She goes away during sleep, but returns within the first minutes after waking up. Due to the “background” course of pain, it often begins to be perceived as a normal condition. But if you ask such a patient if he has a headache, he will always answer “yes.”
- The pain with VSD is “dull.” It can be squeezing, bursting, pulsating, etc. Its intensity is low (except for attacks, which are also “dull”, although strong), therefore, if the patient complains of acute pain, this most likely will not be VSD.
- A constant headache slightly disrupts the perception of reality: sounds may seem muffled, the movements of the surrounding world are inhibited and excessively smooth. This condition can be dangerous for a person, as he may inadequately assess the situation and, for example, get hit by a car.
- Vascular headache is often accompanied by other vegetative manifestations and neurological conditions: dizziness, unsteadiness of gait and difficulties with balance and coordination of movements, fainting, drowsiness, weakness, nausea, tinnitus, “stars” before the eyes, increased sweating (especially of the palms).
- The pain may intensify when bending over, which once again proves its vascular origin.
- The localization can be absolutely any: the entire head, one half of the head, a “hoop” at the level of the forehead, only the forehead/temples/back of the head/vertex/eye sockets, with irradiation to the ear or neck.
- The nature of the pain is usually aching, squeezing or, conversely, bursting, often pulsating (not necessarily in time with the heartbeat).
- Painkillers are usually ineffective for vascular pain. In some cases, antispasmodics help.
Often, exacerbations of headaches occur during periods of intense and prolonged mental activity, strong emotional stress, physical overload, weather and climate changes, etc. Read more about the causes and symptoms of VSD here.
How does a hemorrhagic stroke occur?
Vascular rupture can occur at any time of the day. This is usually preceded by physical or emotional stress. The person suddenly falls, sometimes with a loud cry, and loses consciousness.
Approximately 30% of patients have warning signs that develop within a few minutes to several days. On the eve of a rupture of blood vessels, there may be severe headaches - ones that the person has never experienced. There is a feeling of a rush and a sharp reddening of the face. Sometimes the sensations of numbness in the limbs, muscle weakness, and facial asymmetry appear.
The main symptoms of hemorrhagic stroke are:
| Contralateral hemiplegia | The nerve pathways intersect, so the paralysis is located on the side opposite to the hemorrhage. During a stroke, the left arm and leg stop moving in the right hemisphere, and the right ones in the left hemisphere. |
| Contralateral hemianesthesia | In paralyzed limbs, sensitivity disappears on the side opposite to the rupture. |
| Aphasia | Loss of speech occurs when the dominant (dominant) hemisphere is damaged. For right-handers - right, for left-handers - left. |
| Spatial hemiagnosia with damage to the non-dominant hemisphere | If a right-hander's left hemisphere is affected, and a left-hander's right hemisphere is affected, then the person behaves as if half of the real space does not exist for him. A person does not realize that he has two halves of the body, that food can be eaten from the entire plate, and not from half. Half of everything that is located around a person is not perceived by him. |
| Facial asymmetry | One half of the face does not receive innervation and cannot contract. One nasolabial fold is smoothed out, the smile becomes one-sided, the tongue deviates to one side, water and food flow out of the mouth. |
From the moment these symptoms appear, there is only 3 hours to help the person as much as possible. After 3 (sometimes 6) hours, irreversible changes will occur, then nothing can be corrected.
Diagnosis of headache due to VSD
A headache can occur in many cases and for various reasons, so it is very important to carry out a differential diagnosis of vascular headache:
- magnetic resonance or computed tomography (to exclude tumors, stroke, vascular malformation, consequences of traumatic brain injury, etc.), electroencephalography,
- X-ray of the head and cervical spine (to exclude sinusitis, skull injuries, displacement of the cervical vertebrae),
- vascular doppler,
- neurological examination (palpation of the neck and shoulder girdle, neurological tests),
- blood tests.
If you suffer from frequent headaches, you need to visit a neurologist who will prescribe the necessary tests and select adequate treatment.
HEADACHE: PATHOGENETIC TYPES AND APPROACHES TO PATHOGENETIC PHARMACOTHERAPY
Since modern medicine does not have methods for objective verification of headaches, semiotics is of decisive importance in its diagnosis - a set of signs and features of the manifestation of subjective symptoms that the patient presents to the doctor in the form of complaints. Headache is a symptom, and therefore all attempts to classify it from a nosological position are baseless. At the same time, attempts at pathogenetic systematization and classification are certainly justified, since the identification of pathogenetic types of headache reveals approaches to the main directions of pathogenetic therapy. Experience shows that from a scientific and practical point of view, the following pathogenetic types of headaches can be distinguished: vascular, muscle tension, liquorodynamic, neuralgic and psychalgic. It should be emphasized that the names of these types are deliberately simplified so that the semantic content of these definitions is clear to doctors of different specialties. 1. Vascular type of headache
The vascular type of headache is associated with different types of craniocerebral arteriovenous dystonia. These variants of regional dystonia very often do not correlate with the main indicators of systemic hemodynamics. Arteriodilatatory (arteriohypotonic) variant of the vascular type of headache
associated with a decrease in the tone of the craniocerebral arteries.
This leads them to excessive stretching of the pulse volume of blood. Thus, the so-called pulsating headache is not a sign of vascular pain in general, but only of its arteriodilatatory variant. Excessive pulse stretching of the hypotonic arterial wall can occur even at normal levels of systemic arterial pressure, but more often when it increases. If the artery of the soft integument of the head is subjected to excessive pulse stretching (for example, the superficial, temporal artery), then compression of its adductor trunk in the temporomygomatic region with a finger can reduce throbbing pain. In some cases, the loss of autoregulation extends to arteriovenous shunts, which inappropriately expand, and then arterial blood, bypassing the capillary bed, enters the veins. Intravascular pressure, unusual for veins, adds to arterial pulsating pain a venous component that is uncharacteristic of venous pain itself. The extreme degree of arterial hypotension - paretic arterial dilatation (loss of arterial autoregulation) - is accompanied by impaired permeability and plasmatic saturation of the arterial wall, perivascular edema. Under these conditions, the amplitude of the pulsation decreases and the headache may lose its pulsating character. The throbbing pain gives way to a dull pain and becomes aching or bursting in nature. In the genesis of such pain, allogeneic vasoneuroactive substances take part, which, when permeability is impaired, penetrate into the vascular wall and perivascular tissue along with plasma. The arteriopathic variant of the vascular type of headache
occurs with “spasm” of the craniocerebral arteries.
From a practical point of view, by arterial “spasm” we can mean such a degree of increase in arterial tone that entails ischemic discirculation and ischemic hypoxia. In this case, the headache can be aching and dull in nature, perceived as a feeling of pressure, accompanied by lightheadedness, nausea, unsystematic dizziness, darkening in the eyes, “black spots” before the eyes. The venous variant of the vascular type of headache
(otherwise known as venous insufficiency headache) is caused by excessive blood filling of the venous vessels (veins and venous sinuses) and difficulty in venous outflow. Patients experience heaviness in the head and a feeling of dull fullness. In some cases, these sensations are limited to the occipital region, where the confluence of intracranial venous vessels is projected. However, due to multiple intracranial vein anastomoses, these sensations are usually generalized throughout the head. Venous outflow is more effective in a vertical position, when the direction of gravity (blood mass in the vessels) coincides with the direction of the venous outflow tract (jugular veins). Therefore, venous insufficiency headaches occur or worsen when lying down, working with the head bowed low, when straining or coughing. One of the characteristic symptoms of venous insufficiency headache is morning headache (“heavy head as soon as I opened my eyes in the morning”). Insufficiency of venous tone and venous outflow is confirmed by dilation of the veins of the fundus, cyanosis of the mucous membranes of the nose and oropharynx, pastiness of the face, in particular the eyelids (especially the lower ones). The nature of craniocerebral angiodystonia can be objectified using rheoencephalography (REG), the indicators of which reflect the state of the tone of the arteries and veins, as well as venous outflow. In order not to be mistaken in assessing these indicators and the role of certain changes in tone in the genesis of headaches, it is necessary to make at least two REG recordings - during a headache and during a period of well-being. It should be remembered that the increase in the tone of the craniocerebral arteries can be compensatory in nature and does not require correction with antispasmodics. To clarify the state of tone and determine the reactivity of the craniocerebral arteries, an REG is recorded with a pharmacological test (1/4-1/2 tablets of nitroglycerin under the tongue). To clarify the degree of venous insufficiency, REG is recorded in different body positions: sitting, lying (with and without a pillow), with the head lowered below the horizontal. Indirect information about the condition of intracranial vessels can be obtained by examining the arteries and veins of the fundus. The vascular type of headache is observed with migraine, regional craniocerebral form of vegetative-vascular dystonia, with arterial hypertension of various origins, including against the background of cerebral atherosclerosis, with systemic vasculitis. For the arteriohypotonic variant of the vascular type of headache, migraine attacks, ergotamine, dihydroergotamine, sumatriptan are prescribed, and for vegetovascular dystonia, xanthine drugs are prescribed: aminophylline, pentoxifylline, xanthinol nicotinate. For the arteriospastic variant, drugs that have an antispasmodic effect: phosphodiesterase inhibitors (papaverine, no-shpa), adenylate cyclase activators (vinpocetine and other Vinca minor drugs), a-adrenergic blockers (pirroxan, dihydroergotoxin, nicergoline), calcium antagonists (nifedipine, nimodipine) . For headaches of venous insufficiency, xanthine drugs are most effective. The effectiveness of pathogenetic treatment of vascular headache increases with adequate pharmacotherapy of the underlying disease. In cases where vascular headache is caused by a combined variant of arteriovenous craniocerebral dystonia, they try to isolate the key link in the pathogenesis and prescribe adequate therapy with appropriate vasoactive agents.
2. Muscle tension headache
Occurs when the muscles of the soft integument of the head are tense or compressed. Patients experience a sensation of the head being pulled together by a bandage or hoop. The pain can be local (forehead, crown, cervical-occipital region), but usually quickly generalizes, because the tension of one muscle is transmitted to other muscles through the tendon anoneurosis of the helmet. Tension headaches can occur in two ways. Firstly, under the action of central or systemic factors that facilitate and enhance transmission at the neuromuscular synapse, for example, stress during neurosis (“neurasthenic helmet”), or acting in a similar way, and humoral-hormonal changes (for example, in thyrotoxicosis), as well as during all cases of psychophysiological (psycho-emotional or psychophysical) failure in somatic diseases, especially with a progressive course (hypertension) or incomplete readaptation after somatic or infectious-toxic diseases, as well as after head injury. Another mechanism can be defined as segmental reflex, when tension in the muscles of the soft integument of the head occurs in response to pathological painful impulses during local processes (disease of the eyes, ears, paranasal cavities, cervical osteochondrosis). According to the traditional view, muscle tension headache is objectified by an increase in the potentials of electrical activity of the muscles of the soft integument of the head on the electromyogram. The debatable issue of the existence of tension headaches without tension of the head muscles will be considered when discussing the psychological type of headache. A muscle tension headache may be accompanied by a feeling of lightheadedness and unsystematic dizziness; patients find it unpleasant to comb their hair or wear a hat. The persistence of headaches makes patients irritable, they do not tolerate loud sounds, bright lights, memory and performance decrease. Pathogenetic treatment of pain of central origin includes tranquilizers and antidepressants. With segmental reflex genesis of pain, local methods of influence can play a significant role: lidocaine blockades, physiotherapy, acupuncture; and in the case of diseases of the eyes, paranasal cavities, ears - treatment of pathological processes that caused excessive painful impulses by the appropriate specialists: an ophthalmologist, an otolaryngologist.
3. Liquorodynamic type of headache
Cerebrospinal fluid (CSF) is produced by the choroid plexuses of the ventricles of the brain, circulates in the system of ventricles, cisterns and subarachnoid spaces, is absorbed by the villi of the pachyonic granulations and is sent further along the outflow tract into the venous system. The constancy of intraventricular, cisternal and subarachnoid cerebrospinal fluid pressure is ensured by the consistency of CSF production and outflow. CSF performs both the function of a fluid medium for brain metabolic processes and the mechanical function of a “cerebrospinal fluid cushion” that stabilizes the position of the brain within the strict confines of the intracranial space, limited by the bones of the skull and separated by the falciform process of the dura mater. Any pathological processes that disrupt the described dynamic balance of secretion and outflow, as well as the circulation of CSF, lead to either intracranial hypertension or intracranial hypotension. With increased intracranial pressure, the headache is bursting in nature, patients experience a feeling of pressure “from the inside to the outside,” “from the depths of the brain.” This pain intensifies with straining, coughing, sneezing and depends on the position of the body and head. All positions that impede the circulation of CSF worsen the headache. The rate of increase in liquorodynamic disturbances is also important. With a slow increase in intracranial pressure, adaptive and compensatory changes in the cerebrospinal fluid circulation are possible. Acute hydrocephalus always causes severe headache. CSF circulation disorders with increased intracranial pressure cause “space-occupying processes” that limit the intracranial space, such as tumors, parasitic and arachnoid cysts, brain abscess, cerebral edema due to trauma, inflammation or cerebrovascular accident. Volumetric intracranial processes (tumor, abscess, cyst) are often accompanied by the appearance of focal neurological symptoms, meningeal syndrome, vomiting, and impaired consciousness. Since these processes can cause a state of compression and/or dislocation of the brain that is incompatible with life, it is necessary to use neuroimaging methods - computed tomography (CT) and magnetic resonance imaging (MRI). Indirect signs of disturbances in intracranial pressure and CSF circulation can be obtained using radioisotope scintigraphy. A sign of increased intracranial pressure is venous congestion in the fundus and swelling of the optic nerve head. The dislocation of the middle structures is indicated by the displacement of the middle M-echo. The combination of these symptoms makes it possible to make a correct diagnosis and not be late in consulting the patient with a neurosurgeon to determine the indications and urgency of neurosurgical intervention. It should be remembered that if there is suspicion, and especially if there is objective evidence of displacement of the midline structures, it is unsafe to perform a lumbar puncture. Pharmacotherapy of intracranial hypertension includes dehydrating agents: osmotic diuretics - urea, manitool, sorbitol, glycerin (in the case of normal osmolarity); diuretics of another mechanism of action - furosemide, ethacrynic acid, hydrochlorothiazide, chlorthalidol, clopamide, potassium-sparing diuretics - triamterene, amiloride, spironoloctone. A decrease in intracranial pressure occurs as a result of a decrease in the production of CSF by the choroid plexuses of the ventricles and is accompanied by a dull generalized low-intensity but prolonged headache. Dysfunction of the choroid plexus occurs after a traumatic brain injury or an inflammatory process. The function of the CSF as a “liquor cushion” is lost. As a result, when the head moves or shakes it (for example, when walking), pain-sensitive intracranial structures - vessels, membranes, nerves - are stretched, and pain occurs, which intensifies in an upright position. Because this type of headache occurs after CSF is removed during a lumbar puncture, it is sometimes called a “drainage” headache. Sometimes the puncture site of the membranes after a lumbar puncture “does not close” and for some time CSF leaks through this hole, leading to a decrease in pressure. Drainage headaches are especially intense after a pneumoencephalographic contrast study with the extraction of a large amount of CSF and its replacement with air. Currently, due to poor tolerability, but mainly due to the introduction of CT and MRI into diagnostic practice, this method is not used. A decrease in CSF production can also occur in individuals with a long-term decrease in systemic blood pressure, for example, in patients with a hypotonic type of vegetative-vascular dystonia. If a decrease in systemic blood pressure is combined with hypotension of the cerebral arteries, then with reduced intracranial pressure the amplitude of the pulsation of the intracranial arteries may increase. Then the headache becomes throbbing. A decrease in CSF pressure is confirmed by lumbar puncture; other intracranial and cerebral disorders are clarified using CT and MRI. There are no drugs that could increase the production of CSF by the choroid plexuses of the ventricles. Therefore, indirect approaches can be proposed for treatment. Since the intracranial contents normally consist of the volumes of CSF, brain and intracranial blood supply (especially in the veins), with intracranial hypotension, bed rest is recommended, which increases blood supply, as well as drinking plenty of fluids with a higher than usual content of sodium chloride in food, which leads to a relative increase fluid-containing colloidal mass of the brain. To normalize liquor production, general restoratives and vitamin therapy are prescribed.
4. Neuralgic headache
As stated earlier, this type of pain is classified as facial pain (prosopalgia). They are distinguished by paroxysmal nature, with short paroxysms usually following each other, often causing the patient to suffer from neuralgia for hours or days. Pain, usually piercing, shooting, which, “like lightning” or “electric current”, strikes the patient. The second distinguishing feature is the presence of trigger or trigger zones, the irritation of which provokes an attack. The third characteristic sign is the irradiation of pain to neighboring or distant areas. It is believed that in most cases the cause of facial pain is a focus of pathological activity in the central structures of nociception related to the system of the trigeminal nerve and its central projections [just as the occurrence of an epileptic attack is explained by the presence of a focus (generator) of pathological activity in the systems that regulate the level of wakefulness and consciousness, or systems of motor activity]. For neuralgia of central origin, treatment with antiepileptic drugs, such as carbamazepine, is most effective. In some cases, neuralgia occurs when the sensory nerve is compressed through the mechanism of tunnel syndrome. It is precisely this mechanism that most often occurs with neuralgia of the occipital nerve, which is not included in the group of prosopalgia, but is cranial neuralgia. In these cases, in addition to antiepileptic drugs, they also resort to local effects: lidocaine blockades, physiotherapy, acupuncture.
5. Hallucinatory headache, or psychalgia
The traditional approach to the interpretation of visual or auditory hallucinations requires considering them as an objective sign of mental illness, although no morphological substrate in the form of damage to the structures of the visual or auditory analyzer is found. It is believed that the origin of hallucinations is associated with a neurotransmitter imbalance, leading to the emergence of a focus of pathological excitation in the system of a particular analyzer. A similar mechanism explains hallucinatory headaches that occur during the formation of a focus of pathological excitation (generator) in the central nociception system. Since this focus is formed in the system of structures of the central psycho-emotional perception of pain, the definition of “psychalgia” is applied to this type. It is very important to emphasize the difference between the definition of “psychogenic” (i.e., resulting from psychological stress) headache and the name “psychalgia”. Psychogenic, i.e. caused by stress, can be vascular, muscle tension headache, or neuralgic. And psychalgia itself can be psychogenic when it appears or intensifies after emotional stress. Many authors associate psychalgia with hidden (masked, larved) depression. Many patients with hidden depression complain of pain in the heart, stomach, intestines, etc., while in others hidden depression manifests itself as a headache. This projection of psychalgia onto the head area gave rise to another name - “conversion headache.” An important feature of psychalgia is the absence of specific physical characteristics in the patient’s description of the headache. Instead of specific definitions (for example, squeezing, bursting, pulsating), the patient resorts to vague metaphorical characteristics when describing pain. As a rule, when examined using instrumental methods, no pathology is found in such patients. To treat psychalgia, antidepressants, tranquilizers or antipsychotics are used. If a doctor, during dynamic observation of a patient and after conducting instrumental research methods, diagnoses hallucinatory psychalgia, then it is advisable to refer such a patient for observation to a psychiatrist, since most often the underlying disease is hidden depression.
6. Headache of mixed origin
Previously, different pathogenetic types of headaches in their “pure form” were given. However, we often deal with headaches of mixed origin. Even with migraine, a combination of different pathogenetic types can be observed: arteriohypotonic, venodystonic and muscle tension headache. Even more often, a combination of different headache mechanisms is observed in severe cerebral diseases: stroke, severe traumatic brain injury, meningoencephalitis. Of course, in these cases, the headache, although it requires pharmacological correction, recedes into the background before disorders that threaten the patient’s life. In such situations, the correct combination of symptomatic and nosological pathogenetic treatment is especially important. Summarizing the pathogenetic classification of headache, we consider it necessary to recall that headache is a symptom and as a symptom may not be indicated when formulating a detailed nosological diagnosis or appear in the background or third plan. At the same time, regardless of whether data on headache is included in the diagnosis, all data that allows one to establish the pathological type of headache must be included in medical documents - a medical history or an outpatient card.
Some controversial aspects
of the classification of headaches
As indicated, sharing the concept that a good classification should be based on one defining and dividing sign, in relation to the classification of headache as a symptom, we consider it adequate only to distinguish pathonetic types of headache. Classification according to nosological principle is impossible. All other attempts to group diseases that cause headaches are untenable. However, they have been and are being undertaken (1962 and 1988). Information about the classification of the International Classification Commission of Headaches of the International Headache Society was brought to the attention of neurologists in our country in the article by O.A. Kolosova and V.V. Osipova [1] and in the work of the chairman of this commission and the president of the European Federation of Neurological Societies J. Olesen [2]. The objectives of the article do not include a detailed analysis of the proposed classification. Nevertheless, neurologists in our country should be familiar with the proposals of the International Commission of Experts. The proposed classification divides headaches into 13 groups. Here is a list of these names: 1) migraine; 2) tension headache; 3) cluster headache; 4) various forms of headache not associated with structural lesions; 5) headache associated with head injury; 6) headache associated with vascular disorders; 7) headache associated with non-vascular intracranial disorders; headache associated with the use of certain substances or refusal to take them; 9) headache associated with extracerebral infection (i.e., a general infectious disease - author's note); 10) headache associated with metabolic disorders; 11) headache or facial pain associated with pathology of the skull, neck, eyes ,
2) tension headache; 3) cluster headache; 4) various forms of headache not associated with structural lesions; 5) headache associated with head injury; 6) headache associated with vascular disorders; 7) headache associated with non-vascular intracranial disorders; headache associated with the use of certain substances or refusal to take them; 9) headache associated with extracerebral infection (i.e., a general infectious disease - author's note); 10) headache associated with metabolic disorders; 11) headache or facial pain associated with pathology of the skull, neck, eyes ,
nose, sinuses, teeth, mouth or other facial structures;
12) cranial neuralgia, neuropathy and disafferentation pain; 13) unclassifiable headache. We cannot agree that this list of diseases and conditions can be accepted as a classification of headaches. J. Olesen writes that the first four groups can be classified as primary headaches. In our opinion, only points 1 and 3 can be definitely attributed to primary headache. Point 2 cannot be included regardless of approaches and predilections to interpretations of genesis and names. If we use the previous term “muscle tension headache,” then the headache is secondary either to neurosis or to local pathological processes in the head area. If we use the new term “tension headache,” then it is secondary to depression (or, again, to neurosis). The names of other groups are extremely vague and cannot be considered classification. We believe that the doctor’s thought should follow from the patient’s complaints to establishing the pathogenetic type of headache, from the type of headache to important accompanying symptoms, from the symptom complex that characterizes not only the headache, but the disease as a whole, to the nosological diagnosis of the underlying disease. We wrote about this back in 1987 [3]. The authors who took the trouble to introduce our neurologists to the international classification did not provide the full title of the work of the International Commission either in the title or in the text of their articles, but it reads like this: “Classification and diagnostic criteria for headaches, cranial neuralgia and facial pain.” Therefore, if the division into 13 groups cannot be accepted as a classification, this division and especially the explanation for it can only be considered as a diagnostic algorithm that can be used in the transition from establishing the pathogenetic type of headache to establishing a nosological diagnosis. It is important to understand that the same pathogenetic type of headache can be observed in different diseases and, conversely, with the same disease, the same patient may experience headaches of different pathogenetic types. An example is hypertension. Classics of Russian medicine G.F. Lang and A.L. Myasnikov perfectly described the types of headaches associated with hypertension: neurasthenic, vascular, “typical,” and toxic. From the point of view of our presentation, neurasthenic is a headache of muscle tension, vascular is arteriohypotonic, “typical” is a headache of venous insufficiency, toxic is liquorodynamic. In other words, the essence is the same, the names are simply clarified from the point of view of pathogenesis. Thus, the same patient at different stages of the disease may have a headache of one or another pathogenetic type. Or another example: cervical osteochondrosis. The same patient may have muscle tension headache, occipital neuralgia, headache of vascular origin as part of the posterior cervical sympathetic syndrome (Barre-Lieu vertebral artery syndrome).
Literature:
1. Kolosova O.A., Osipova V.V. Classification of headaches // Journal. neurology and psychiatry named after. S.S. Korsakova, 1996, No. 3, p. 8-11. 2. Olesen J. Diagnosis of headache // Neurological Journal, 1996, No. 3, p. 4-11. 3. Shtok V.N. Headache. M.: Medicine, 1987, 303 p. 4. Classification Committee of International Headache Society. Classification and Diagnostic Criteria for headache disorders, cranial neuralgia and facial pain. Cephalgia 1988;8(Suppl.1.7):1-96.
Treatment of vascular headache and prevention of VSD
There is no actual treatment for vascular headache, i.e. It is extremely difficult to stop an attack of pain. Therapeutic measures are aimed at increasing vascular tone, restoring normal blood circulation to the brain and improving the functioning of the cardiovascular system. Read more about the treatment of vegetative-vascular dystonia and specifically headaches at the Aximed neurology clinic “here”.
In addition to drug treatment for people suffering from headaches and other symptoms of VSD, Aximed neurologists recommend:
- eliminate stressful situations from your life as much as possible (change jobs, undergo a course of family psychotherapy, etc.),
- maintain a sleep/wake and work/rest schedule,
- stop smoking (this constricts blood vessels and weakens the elasticity of the walls),
- eat a complete and balanced diet,
- Jogging is highly recommended, since in the process the brain is actively saturated with oxygen (which may be lacking due to reduced blood supply to the brain),
- massages (especially the collar area).
Are you plagued by headaches? Consult a neurologist. Vegetative-vascular dystonia can be treated, but the more advanced the case, the longer it will take, and the more likely it is that the pain will return again. Do not delay treatment, because life without pain is much more pleasant.
How to cure a headache with one injection?
The Center for the Study of Pain of JSC "Medicine" (clinic of Academician Roitberg) uses targeted (targeted) treatment of migraines with the monoclonal antibody drug "Irinex", which is administered subcutaneously by injection. This method has already helped thousands of patients in the USA and Europe, and has now become available in Russia.
Specialists at the Pain Research Center approach migraine treatment in a comprehensive manner. This approach allows us to minimize the impact of the disease on the body and overall health. The combination of various methods of rehabilitation and therapy allows you to achieve excellent results in a short time and a significant improvement in the quality of life.