Neurologist
Chudinskaya
Galina Nikolaevna
Experience 29 years
Neurologist, member of the Association of Interdisciplinary Medicine
Make an appointment
Plexopathy is damage to the nerve plexuses due to disease or injury. The most commonly affected nerves are the lumbosacral, brachial, or cervical nerves. Plexopathy has ICD-10 code G54. With a long course of the disease, a person loses his ability to work, and in the most severe cases, muscle paralysis occurs. If detected at an early stage, hand plexopathy is completely curable with the help of manual therapy and other modern treatment methods.
Symptoms and signs of plexopathy
Brachial plexopathy according to ICD-10 is classified into several other types depending on the location of damage to the nerve plexuses. Based on this criterion, the most common types of disease are identified:
- brachial plexopathy (G54.0). Of all types, it is more common than others, mainly occurring after injury;
- Duchenne Erb plexopathy (G54.1). Develops when the roots C5 and C6 are affected, manifested in paralysis of the infraspinatus, biceps brachii and deltoid muscles of the shoulder;
- sacral plexopathy and lumbar plexopathy (G1). In most cases, it develops against the background of degenerative processes in the intervertebral discs with protrusions or hernias;
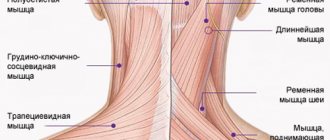
- cervical plexopathy (G2). Damage to the nerve plexuses at the level of C2-C3, which are responsible for the muscles of the shoulder girdle and back of the neck, partially the face and scalp.
Brachial plexus plexopathy according to ICD 10 is the very first one, since it is more common than others. This is explained by the location of the nerve ganglion - it is located in such a place that it is constantly at high risk of injury. This is why post-traumatic brachial plexopathy is diagnosed in most patients who present with characteristic complaints.
Plexopathy occurs in 2 stages:
- neuralgic. It suggests the appearance of spontaneous pain, which intensifies when the affected plexus is compressed, in particular, with various movements;
- paralytic. At this stage, paresis and paralysis occur. They affect only those muscles that are innervated by the affected nerve plexuses.
At the second stage, reflexes also worsen, tactile sensitivity is impaired, swelling and vasomotor disorders appear. Post-traumatic brachial plexopathy most often causes pain in the supraclavicular and infraclavicular region, which radiates to the arm. As the disease progresses, swelling of the hand, pallor and cyanosis of the hands, and sweating of the palms occur.
Kinds
Idiopathic brachial neuritis
Idiopathic brachial neuritis is a disorder of unknown etiology with an asymmetrical arrangement of the brachial plexus. It occurs in all age groups, but is more common between the third and seventh decades. Men are more often affected than women. Intervening events occurring days or weeks before the onset were noted in 28-83% of cases in various ways. Respiratory infections, influenza-like illnesses, immunizations, surgery, and emotional stress were common symptoms, with no triggers found in half of the cases. Idiopathic brachial neuritis is more common in men who engage in vigorous athletic activities such as wrestling, weight lifting, and gymnastics.
The pathophysiology of idiopathic brachial neuritis is not fully understood, and the disease is considered an immune-mediated disorder.
Idiopathic hypertrophic brachial neuritis
This disease is uncommon and tends to gradually affect the brachial plexus. The disease continues for several months or even years, and gradually progressive weakness and wasting of the segments affected by this disease is a key, but at the same time, often ignored symptom.
This disease differs from the above-described idiopathic brachial neuritis in its painless course, although some patients may have minor pain and weakness.
Hereditary neuralgic amyotrophy
Hereditary neuralgic amyotrophy is an autosomal dominant disorder characterized by repeated episodes of paralysis and sensory impairment of the affected limb, preceded by severe pain. Hereditary neuralgic amyotrophy is genetically linked to chromosome 17q25, where mutations in the septin-9 gene have been found. Hereditary neuralgic amyotrophy is a rare disease and its worldwide prevalence is unknown.
Onset of hereditary neuralgic amyotrophy occurs at birth or later in childhood, with a good prognosis for cure. However, individuals with hereditary neuralgic amyotrophy may have permanent residual neurological deficits after repeated attacks.
Neurogenic thoracic outlet syndrome
Neurogenic thoracic outlet syndrome is characterized by pain, paresthesia, and weakness of the upper extremities, which may be aggravated by raising the arms or frequent movements of the head and neck. This is usually seen in women.
Cancer-associated brachial plexiopathy
Brachial plexus involvement is a well-known complication of cancer. Pectoral plexopathy in such cases may be caused by metastatic spread or a consequence of radiation therapy for cancer.
Traumatic form of brachial plexopathy
Trauma is one of the most common causes of brachial plexopathy. These injuries usually result from a motorcycle or high-speed traffic accident, a fall from a significant height, or an impact. This can occur with penetrating trauma and gunshot wounds. This may be the result of iatrogenic trauma. In injured patients, the consequences should be carefully assessed. Determine the extent of head, neck and shoulder injuries. With open injuries, there may be damage to large blood vessels and lungs, in which case urgent surgical intervention is necessary.
Causes and risk factors of plexopathy
Brachial plexopathy most often occurs after some kind of trauma, such as carrying heavy objects for a long time, a dislocated shoulder, birth injuries, or after a car accident. Post-traumatic plexopathy is always associated with some kind of mechanical impact on the shoulder area.
In some cases, the nerve plexuses in the shoulder suffer from compression by the tumor. Then compression plexopathy is diagnosed. In the cervical region, pathology is relatively rare.
The second most common type is lumbosacral plexopathy. It can be connected:
- with a space-occupying formation behind the peritoneum;
- fracture of the pelvic bones;
- hemorrhage caused by an overdose of anticoagulants or hemophilia;
- surgery on the hip joint;
- aneurysm of the aorta or iliac artery.
Forms of plexite
Certain forms of development of plexitis are identified. These include:
- Traumatic. It is detected as a result of injury to the nerve plexus,
- Compression-ischemic. Can occur with prolonged compression of the plexus. Leads to impaired nutrition of nervous tissue,
- Infectious. The disease is associated with infection in the nerve ending,
- Infectious-allergic. Occurs due to an unusual allergic reaction of nerve endings due to the introduction of a vaccine. This is accompanied by excessive inflammation in the plexus,
- Toxic. May develop as a result of poisoning,
- Dysmetabolic. This form of plexitis is associated with impaired metabolism in the body due to poor nutrition.
When to see a doctor
Already when the first symptoms of plexopathy appear, it is necessary to consult a doctor, because the earlier the disease is detected, the more effective the prescribed treatment will be. A neurologist diagnoses this disease. JSC "Medicine" (academician Roitberg's clinic) in the center of Moscow has a whole staff of doctors in this specialization. Our patients receive high-quality treatment and psychological support, which, combined with timely rehabilitation, allows them to quickly return to a healthy life.
Possible complications and consequences
Complications may include a persistent neurological defect, paralysis, weakness in the limbs, and impaired sensitivity.
Among the possible consequences, a violation of labor adaptation as a result of a neurological defect is identified. Due to severe muscle weakness, it is impossible to perform certain types of work. It becomes extremely important to follow the correct regimen, perform physical therapy and start eating right.
It happens that when this disease develops, the patient has to move with the help of crutches. In this situation, it is important to choose them correctly, as well as to know how to use them, so as not to provoke increased pain in the shoulder area.
You can buy an omron compressor nebulizer from us inexpensively.
Treatment
Treatment of brachial plexopathy, depending on the patient’s condition, can be carried out on an outpatient or inpatient basis. Therapy is aimed at eliminating the cause of the disease. If it is an infection, antibiotics are prescribed, if it is a tumor, it is removed, etc.
Upper plexopathy at an early stage can be treated through manual therapy. First of all, this is a spinal traction procedure, which allows you to cope with the effect of compression. As a result, the nerve fiber begins to receive sufficient nutrition and is completely regenerated.
The following medications are prescribed to the patient:
- anticholinesterase;
- B vitamins;
- painkillers;
- trophic means;
- improving microcirculation;
- steroidal anti-inflammatory drugs.
In addition to medications, the following methods are used:
- massage – after acute inflammation subsides;
- physiotherapy: ultrasound, electrophoresis, ozokerite, magnetic therapy;
- physiotherapy;
- balneotherapy, cryotherapy, reflexology, laser therapy.
Erb's plexopathy can also be treated with surgery if pharmacological drugs do not produce the desired results. In such cases, neurosurgical operations are performed to restore the integrity of the nerve column or eliminate its compression (squeezing).
Prevention of plexitis
After completing the course of treatment, the patient should follow preventive measures. They should also be performed by those who have not encountered this disease for prevention purposes. Swimming is very beneficial. It is this activity that helps stimulate and keep all muscles toned and prevents the development of the disease.
Swimming is an excellent remedy against the occurrence of arthritis, arthrosis, and other negative symptoms. It is worth combining physical activity with this hobby to warm up your joints. This will prevent ossification, increase the body’s performance, as well as its resistance to various diseases.
For prevention purposes, it is very important for the patient to wear warm clothes in winter. Don't forget about proper, balanced nutrition. You need to include foods high in fiber in your diet. Such products include vegetables, fruits, and herbs. You should avoid canned, fried, spicy and hot foods. You should eat in small portions, 5-6 times a day. It is important not to spread infectious diseases. Their timely treatment with the use of antibacterial and antiviral agents is the key to good health and prevention of the typical disease of plexitis.
For the purpose of prevention, the patient is also prescribed sanitary and resort treatment in health resorts. Basically, this option for restoring health can be prescribed as a result of identifying a chronic form of the disease. It is very important for a patient with this diagnosis to rest more and not overexert. You should try to adhere to a healthy lifestyle, eliminating bad habits such as smoking and alcohol abuse.
In order to prevent the recurrence of the disease in the future, it is necessary to initially identify the source of infection, preventing its spread.
In many sanatoriums, the following methods of restoring health are used for plexitis:
- Conditions for complete rest are provided,
- Therapeutic baths,
- Restoring the health of the soul,
- Mud treatment
- Thermotherapy,
- Massage course,
- Physiotherapy,
- Acupuncture,
- Proper, balanced nutrition is provided.
A special role is given to a proper diet rich in B vitamins.
Home remedies
Shoulder plexopathy allows the use of traditional methods of treatment, but only after consultation with the doctor and exclusively as a complement to the main therapy. Some effective home remedies include:
- ointment with propolis. Melt 15 g of animal fat in a water bath, then add 1 g of propolis. Mix everything and leave to cool. Use to massage the sore area 2-3 times a day;
- bath with mint. Pour 5-7 tablespoons of mint leaves into 1 liter of boiling water, leave for 2-3 minutes, then pour into a warm bath. Take it within 15-20 minutes.
Causes of elbow tendinitis
Tendons attach muscle to bone and transmit muscle contractions to the bone lever, providing biomechanics for the musculoskeletal system. They consist of compact parallel bundles of collagen fibers. Collagen bundles are quite strong, but not elastic enough, so microdamages often occur that do not have clinical manifestations.
Microtraumas trigger an inflammatory process that culminates in fatty degeneration and calcification (deposition of calcium salts in tissues). A degenerated tendon is less strong and vulnerable, which leads to repeated injuries and inflammation.
Reference!
Long-term, low-grade inflammation causes degeneration and thinning of connective tissue structures. More often, inflammatory processes occur in the tendons and ligaments of the knee, shoulder and hip joints.
The occurrence of tendon pathology
The main cause of tendonitis is intense stress on the musculo-ligamentous system, leading to microtrauma. Tendons are damaged by frequent monotonous movements. At risk are athletes (tennis players, volleyball players, basketball players) and people who have to perform numerous monotonous movements due to their professional activities (painters, bricklayers, hairdressers).
Secondary tendinitis occurs against the background of rheumatic, endocrine, and infectious diseases.
Inflammation of the tendons is possible due to long-term use of medications.
In autoimmune pathologies, the patient’s immune system synthesizes antibodies that destroy fibroblasts and fibrocytes of collagen fibers, which leads to chronic inflammation, degeneration of ligaments and tendons.
Myths and dangerous misconceptions in the treatment of plexopathy
Many patients do not attach much importance to such a treatment method as gymnastics. Medicines only help relieve symptoms in their acute stage, but do not help create a strong muscle corset and ensure good blood flow in the musculoskeletal system.
Only a sufficient level of physical activity, agreed with your doctor, will help with this. The same applies to bed rest during the acute period - 2-3 days are enough, after which it is necessary to get up and begin to engage in physical activity.
Diagnostics
Many adult injuries will not recover on their own, and early evaluation by physicians who are experienced in treating these problems is important. Some injuries can heal over time or with quality therapy. Recovery time may be weeks or months. When the situation is unlikely to improve, several surgical techniques can be used to improve recovery.
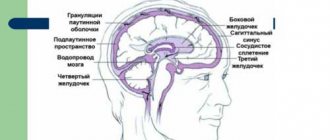
To decide which injuries are most likely to resolve on their own, your doctor will rely on several exams of your arm and shoulder to check muscle strength and feeling in different areas. Additional tests such as MRI scans or CT/myelography may be used. A nerve conduction study/electromyogram, a test that measures electrical activity transmitted by nerves and muscles, may also be performed.
In some cases where nerve repair does not occur, tendon transfer surgery may be performed.
Diagnostic methods
The diagnosis is initially made by a specialist - a neurologist. The main task is to study the patient’s medical history, examination, and identify trigger points that limit the extent of the pathology. At the first diagnostic stage, plexitis is distinguished from other similar anomalies, such as neuralgia. The latter manifests itself after previous cooling of the body and is not accompanied by a violation of the motor functions of the organ.
After a preliminary diagnosis has been made, the patient is referred for hardware tests:
- Electroneurography. Helps evaluate the intensity of the impulse passing through the nerve fibers.
- Ultrasound examination of the articular area.
- X-ray examination of the limb, lungs.
- Laboratory analysis of blood composition, including glucose levels.
- Computer scan of the articular area.
- Magnetic resonance screening of the brachial plexus.
The most effective ways to detect plexitis are MRI and CT. They are prescribed in cases where other diagnostic methods do not show correctness. Diagnostics are carried out using special equipment of high power and resolution. A distinctive feature is the non-invasiveness of the techniques (no instrumental penetration through tissue). If your doctor prescribes a referral for a tomography, you should not ignore the recommendation. In many cases, only hardware scanning can answer the question of the cause of the disease.
Not every district clinic offers a tomogram. Our portal provides a detailed list of diagnostic centers providing this service. Clinics are distributed by rating and popularity. On the pages of the site you can compare prices for diagnostic procedures, read reviews, leave your own comment, and choose a medical organization in any area of the city. You can make an appointment at the selected clinic by calling the single city registration center. Contacts are located at the top of the page. Operators provide portal users with free consultation on remaining issues and help book free time for scanning.