Vestibular rehabilitation therapy
Fortunately, most of us go about our daily lives oblivious to the complexity of our body's systems that keep us upright and balanced.
But this only happens until, for some reason, our coordination and balance are disrupted, reminding us how vital simple everyday tasks are. Vestibular Rehabilitation Therapy (VRT) consists of a set of exercises that encourage the brain and spinal cord to restore imbalances that occur due to diseases or abnormalities of the vestibular system or damage to the central nervous system.
This guide will help you understand:
- anatomy of the vestibular system
- why do we need ART?
- What disorders does ART usually treat?
What are the causes of violations
Under normal conditions, we do not think about maintaining balance when walking, or about the position of our eyes when moving, since this happens on a subconscious level. In this case, disruption of the vestibular apparatus leads to dizziness, nausea and other unpleasant consequences. This is explained by the fact that when the body moves in space, the senses receive a lot of contradictory information: the rapid movement of objects in front of the eyes causes irritation of the receptors of the balance organ. The severity of symptoms of dysfunction of the vestibular apparatus depends on the individual sensitivity of the body. In children, the main cause of motion sickness is a weak nervous system, which finally matures by the age of 12-14 years. It should be remembered that everyone is susceptible to manifestations of dysfunction of the vestibular apparatus, so instead of unnecessary worry, you should think about taking appropriate measures to correct existing disorders.
Anatomy
The anatomy and physiology underlying the human body's sense of balance is complex. Many systems are involved, including the brain, spinal cord, eyes, ears, and receptors in the skin, joints, and muscles. Impairment in any of these areas due to injury or illness can negatively impact your sense of balance.
The inner ear, also called the labyrinth, consists of the semicircular canals along with the saccule and the uterus. Collectively, this inner ear system is called the vestibular system or vestibular apparatus.
The inner ear also contains the cochlea, which is the main structure involved in hearing perception.
The three semicircular canals respond to rotational movements of the head. The canals are located at 90 degrees to each other and are filled with a fluid called endolymph. Hair cells are located at the base of each semicircular canal and project into the endolymph. The movement of the head causes movement of the endolymph in the channels, which in turn causes the hair follicles to move accordingly and emit impulses about balance that travel to the brain. Hair cells in the sac and utricle respond to linear acceleration of the head, such as when riding in an elevator or moving forward.
Sensory information from the inner ear is transmitted to the brain through the vestibular portion of the eighth cranial nerve, which is also called the vestibulocochlear nerve. The cochlear part of the nerve transmits hearing information. Certain areas of the brain, particularly the cerebellum and brain stem, as well as parts of the cerebral cortex, process sensory information coming from the inner ear. When both the right and left inner ears send the same information to the brain, the body is balanced. When the body or head moves, the sensory information from the ears is not identical, so the brain perceives the movement and the body adjusts accordingly.
The ears work closely with the eyes to maintain balance. The basis of this is
vestibulo-ocular reflex (VOR). This is an automatic function of the eyes that stabilizes images on the retina in response to head movements. This reflex causes the eyes to move in the opposite direction to the movement of the head so that the eyes remain stationary on the observed target. Thus, precise information from the vestibular system influences the sense of balance.
If one inner ear is affected by disease or injury, then sensory information sent to the brain will falsely indicate movement from that vestibular system. In this case, the eyes will adjust accordingly and move opposite to the perceived movement despite the fact that the head is actually stationary. The result is involuntary back and forth eye movements. This eye movement is called nystagmus and, if present, makes any healthcare professional suspect a vestibular problem.
There are two other reflexes, the vestibulocervical reflex and the vestibulospinal reflex, which also help the body maintain a sense of balance.
The vestibulocervical reflex works in conjunction with incoming vestibular information and the neck muscles to stabilize the head. And the job of the vestibulospinal reflex is to create compensatory movements of the body in response to vestibular input in order to maintain balance and avoid falling.
Disturbance along any part of the anatomical pathway described above can affect the perception of balance or equilibrium. A problem with the part of the inner ear or sensory information transmitted to the brain through the vestibulocochlear nerve is called peripheral vestibular disorder.
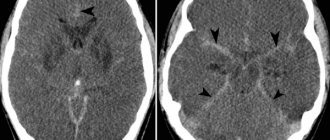
If a problem affecting balance is due to damage to a structure within the brain itself, which then affects the reception and integration of balance information, it is called a central vestibular disorder.
Common disorders treated with ART
The most common peripheral vestibular disorders treated with ART are benign paroxysmal positional vertigo (BPPV) and any injury or disease that results in decreased function of the inner ear. This decreased function may be associated with disorders such as Meniere's disease, vestibular neuritis or labyrinthitis, or acoustic neuroma. The term unilateral or bilateral vestibular hypofunction can be used to describe decreased function of the vestibular system in one (unilateral) or both (bilateral) ears due to disease or injury.
Clinically, any peripheral dysfunction in the vestibular system that affects balance can potentially be treated with ART, however the effectiveness of treatment will depend on the exact cause of the vestibular problems.
Central vestibular disorders such as multiple sclerosis or stroke may also respond to ART, although in general peripheral vestibular disorders tend to respond better.
Benign paroxysmal positional vertigo (BPPV)
BPPV is a common clinical balance disorder characterized by recurrent attacks of dizziness that are brief in nature (usually 10-60 seconds) and most often triggered by certain head positions. Benign, in medical terms, means that it is not life-threatening. Paroxysmal means that it occurs with rapid and sudden onset or worsening of symptoms.
BPPV is the most common cause of recurrent dizziness. BPPV is thought to be caused by calcium carbonate crystals (called otoconia, otoliths, or “ear stones”) in the semicircular canals of the inner ear. Under normal circumstances, these crystals are located within the sac of the ear, but in BPPV, these crystals are thought to dislodge and migrate into the semicircular canals of the ear. This misalignment is thought to have a number of possible causes, such as ear or head trauma, ear infection or surgery, or natural degeneration of the inner ear structures. Often, however, the direct cause cannot be identified.
Otoconia settle in one place of the canal when the head is motionless. The most common canal to be affected is the posterior semicircular canal. A sudden change in head position, often caused by actions such as rolling over in bed, getting out of bed, tilting the head, or looking up, causes crystals to shift. This shift, in turn, sends false balance signals to the brain and causes dizziness.
Dizziness due to BPPV can be severe and accompanied by nausea. The attacks may occur for seemingly no reason and then disappear for several weeks or months before returning again. BPPV usually affects only one ear, and although it can occur at any age, it is often seen in patients over 60 years of age and is more common in women. Nystagmus is usually present.
Meniere's disease
Meniere's disease is a chronic, incurable vestibular disorder characterized by symptoms of episodic severe dizziness, fluctuating hearing loss, ear fullness and/or ringing in the ear (tinnitus), and nystagmus.
This disease gets its name from the French physician Prosper HaMeniere, who in the late 1800s theorized the cause of these symptoms, which he noted in many of his patients.
The exact cause of Meniere's disease has not yet been determined, but it is thought to be due to an abnormal amount of endolymphatic fluid accumulating in the inner ear and/or an abnormal accumulation of potassium in the inner ear.
The early stages of acute attacks of Meniere's disease vary in length from 20 minutes to 24 hours. The attacks may occur regularly over the course of a week or may occur weeks or months later. Other symptoms may coincide with an attack, such as restlessness, diarrhea, shaking, blurred vision, nausea and vomiting, cold sweats, and a rapid pulse or racing heart. After attacks, patients often experience extreme fatigue that requires many hours of rest to recover. For some patients, the time between attacks may be symptom-free, but other patients report persistent associated symptoms even between attacks.
Vestibular neuronitis
Vestibular neuronitis is an inflammation of the inner ear or its associated nerve (the vestibular portion of the vestibulocochlear nerve) that causes dizziness. Hearing may also be affected if the inflammation also affects the cochlear nerve.
Dizziness caused by vestibular neuronitis has a sudden onset and can be mild or extremely severe. Nausea, vomiting, unsteadiness, decreased concentration, nystagmus, and blurred vision may also occur. Most often, infections that cause inflammation of the inner ear or vestibulocochlear nerve are viral rather than bacterial. Proper diagnosis as to whether it is viral or bacterial is important to ensure the most effective and appropriate treatment.
Acoustic Neuroma
An acoustic neuroma is a benign tumor on the vestibulocochlear nerve. Early symptoms include hearing loss in the affected ear, ringing in the ear (tinnitus), dizziness, and a feeling of fullness in the ear. The tumor grows slowly, so symptoms appear gradually and can be easily missed in the early stages. As the tumor grows, it can press on other nerves in the area, and symptoms such as a headache or pain and numbness in the face may occur. Dizziness or other balance problems may occur as the tumor grows.
Vestibular symptoms
Peripheral or central vestibular disorders can lead to a number of different symptoms. VRT can potentially relieve or resolve any symptoms associated with a vestibular disorder.
Common symptoms include:
- dizziness
- blurred vision
- fatigue
- anxiety
- headache
- nausea and/or vomiting
- cold sweat
- ringing/tinnitus
- hearing loss
- twitching orbital stagmus
- ear pressure
- panic attacks
- leaning to the side
- fear of falling
- increased risk of falls
- imbalance
- unsteady walk
- anxiety
- depression
Treatment
Treatment of vestibular syndrome depends, first of all, on the genesis of this syndrome. First of all, it is necessary to exclude damage to the vestibular analyzer of central origin (brain disease, trauma). Treatment will depend on the pathogenesis of vestibular disorders.
In some cases, with vestibular disorders, it is necessary to influence factors of daily activity, such as travel, in a car or elevator, which will reduce the risk of injury. If you have BPPV, your doctor may order a series of simple movements, such as the Epley maneuver, to release the otoconia in the semicircular canals. If you have Meniere's disease, your doctor may recommend dietary changes, such as reducing salt in your diet and limiting alcohol and caffeine. Quitting a habit such as smoking can also have a positive effect. It is possible to administer such an antibiotic in small doses (gentamicin) or a steroid behind the eardrum. In severe cases of Meniere's disease, surgical treatment is possible. Drug treatment of vestibular disorders includes the use of drugs from the group of anticholinergics, antihistamines, and benzodiazepines. Symptomatic drugs, such as cerucal, are also used. Recently, a drug such as betaserc has been used to treat dizziness.
In the presence of inflammatory processes in the middle ear, the use of anti-inflammatory treatment or antibiotics is necessary.
If you have persistent vestibular disorders, you need to take a number of measures to reduce the risk of falling, for example, using handrails when climbing stairs, wearing low-heeled shoes, installing handrails in the bathroom, avoiding driving, etc.
Diagnosis of the cause of dizziness
A detailed history of your medical condition is the most important information your doctor needs to diagnose the cause of your vestibular disorder and then administer appropriate ART.
The doctor will ask you to describe your vestibular symptoms in detail. Any symptoms you experience above or others should be mentioned. Your doctor will want to know when the first episode of your symptoms occurred, how long they lasted, and whether they were related to any other events, such as a car accident, head injury, illness, or infection.
He will also want to know how often symptoms have recurred since the first episode and the general pattern of symptom frequency. Find out exactly what causes your symptoms, such as moving your head in a certain direction or getting out of bed. For dizziness, your doctor will ask about the nature of what you're feeling and whether you experience episodes of true dizziness where you have a spinning sensation.
The doctor will also want to know if there is anything that reduces or increases your symptoms, and if you are taking any medications, or if you have a family history of any inner ear disorders or central nervous system disorders.
He may ask you to rate the intensity of some of your symptoms on an objective scale. Finally, they will ask about all the daily activities that are related to your vestibular problem, such as walking, driving, working, and even household activities such as dressing, bathing, showering, and housekeeping.
He will also want to know if you have any falls.
The doctor will examine your eye movements by asking you to follow certain objects with your eyes or by asking you to move your head while keeping your attention on a specific target.
An examination of the joints and neck muscles is also carried out to determine the cervicogenic nature of dizziness.
Finally, your doctor may ask you to fill out a questionnaire to determine the intensity of your vestibular symptoms.
Depending on what the doctor finds during the initial examination, they may send you for a series of other tests to further determine the cause of your vestibular symptoms.
Vestibular rehabilitation
As stated above, ART can be used to treat various disorders that cause dizziness or balance problems. Almost any disorder that occurs due to vestibular dysfunction and does not receive sufficient compensation can be treated with ART. The effectiveness of ART depends on correct diagnosis of the cause of the imbalance, the skill/training of the therapist in developing and administering the treatment, and adherence to the prescribed exercise program.
As explained earlier, the purpose of ART exercises is to encourage the brain and spinal cord to compensate for any balance deficits that arise due to diseases or abnormalities of the inner ear or central nervous system. In other words, patients teach their vestibular system to do one of several things; adapt to the stimuli presented, substitute other sensory pathways, or become accustomed to changing vestibular signals sent to their brain so that they can manage their vestibular disorder and maintain normal functioning despite possible ongoing symptoms.
In some cases, ART can eliminate vestibular symptoms. Unfortunately, however, this is not always the case, so minimizing symptoms or the frequency of recurrence of symptoms is considered a successful outcome of ART.
Research in the field of ART shows that, in general, ART exercises are effective in reducing many symptoms of vestibular disorder and that these improvements can often persist for several months after therapy. However, the effectiveness of therapy often depends heavily on what exactly is causing the vestibular symptoms in the first place and the use of individualized exercises rather than a standard exercise protocol.
ART, however, is not always effective for all vestibular problems. There are even some vestibular problems where exercise is not considered appropriate, so proper diagnosis of the cause of the symptoms is important.
ART exercises
If your physiotherapist feels that ART is right for you after completing your assessment, they will prescribe a range of individual exercises for you to do regularly. These exercises will focus on your specific vestibular problem and associated symptoms.
Additionally, the exercises you are prescribed will focus on any day-to-day problems you are facing as a result of your symptoms. Some exercises will be done with your physical therapist on a stability platform, and others will be retrained so that you can do them on your own as part of a home exercise program.
Medications to treat your symptoms may be an addition to ART and should be discussed with your doctor.
Treatment of dizziness with cervical osteochondrosis
The treatment method for such manifestations of cervical osteochondrosis as dizziness and headache is determined by the condition of the spine and vascular system. A mandatory examination is carried out (preferably MRI as the most informative). Based on the results of the examination, physiotherapeutic procedures, drugs that improve blood supply in the vertebral artery system and reduce irritation of the nervous system, and massage of the cervical-collar area can be prescribed. Ascorbic acid and retinol help improve cerebral oxygenation (supply the brain tissue with oxygen), which eliminates dizziness. But all drugs must be used with caution and remember that long-term use of even ascorbic acid, especially in large doses, can harm the body.
Electrophoresis is the most commonly used physiotherapy procedure. Its essence is a local increase in temperature and improvement of blood circulation, which relieves muscle spasms, eliminates pain and speeds up the healing process. In general, any thermal procedures relieve muscle spasms and improve blood circulation.
Magnetotherapy involves the use of low-frequency magnetic field inductors aimed at the problem area, which leads to local dilation of blood vessels, improved oxygenation and metabolism, accelerated elimination of toxins and reduced blood viscosity. Thanks to this, magnetic therapy has an anti-inflammatory, analgesic and anti-edematous effect.
Effective assistance in the treatment of osteochondrosis of the cervical spine can be provided by a modern drug - the therapeutic pain-relieving anti-inflammatory patch NANOPLAST forte.
Our approach to treatment (exercises on the stabiloplatform)
Stabilometry is a modern method that allows you to assess the state of a person’s balance in various diseases.
The patient is examined on a special platform that records minimal vibrations of the human body with subsequent computer processing. At the end of the study, a conclusion and recommendations for rehabilitation in the form of training are issued.
With the help of video games, a person, by moving fulcrum points, “guides” the actions of the character on the screen, thereby training his vestibular apparatus. Repeated repetition of such training increases the effectiveness of the therapy.
Treatment on a stabiloplatform with biofeedback is prescribed as part of complex therapy for diseases and pathological conditions such as:
- imbalance, loss of coordination;
- frequent dizziness and headaches;
- diseases of the vestibular apparatus;
- panic attacks accompanied by dizziness
- polyneuropathy;
- vascular diseases, conditions of impaired blood supply to the brain, incl. post-stroke
- various spinal injuries (vertebral displacement, curvature)
- flat feet
Treatment of neck diseases
Some patients who experience dizziness or balance problems also have orthopedic neck problems that cause or worsen their symptoms. In these cases, your physiotherapist at Healthy Sports can also provide hands-on treatment in combination with the other ART exercises described above.
Strategies for self-administration
Secondary damage due to vestibular problems can occur due to frequent falls. As part of your ART, your doctor will talk about simple strategies that can minimize the risk of secondary injuries. For example, you may be advised to use walking aids if you are tired or in a particularly busy environment, such as a grocery store.
Conclusion
ART can be extremely helpful in reducing or eliminating any vestibular symptoms and imbalances you may experience due to diseases or abnormalities of the inner ear or central nervous system. These exercises will lead to the best results if they are prescribed by one of our doctors at the Healthy Sports Medical and Health Complex.
You can undergo an examination at the Healthy Sports Medical and Health Complex, make an appointment by phone: 58-88-28
Which doctors should I contact if a vestibular disorder occurs?
If you notice disturbances in your vestibular state, you should definitely seek advice from a specialist - a neurologist. Based on certain symptoms and external signs, only a doctor can make an accurate diagnosis. Therefore, if you find signs of a neurological disease, seek help from a neurologist. Do not put your health at risk - do not self-medicate.
Primary appointment with a neurologist: 1850 RUR.
Sign up Online 5% discount when registering from the site