- Gallery
- Reviews
- Articles
- Licenses
- Vacancies
- Insurance partners
- Partners
- Controlling organizations
- Schedule for receiving citizens for personal requests
- Online consultation with a doctor
- Documentation
Dizziness – apparent rotation of objects inside the head or surrounding objects around one’s own body and a feeling of loss of balance.
Dizziness in children is a separate issue; it is very difficult to identify. The fact is that children cannot always describe this symptom. Until a child learns to speak, recognize his feelings and describe them in words, adults do not take his complaints seriously.
How can you suspect dizziness in a child?
Children's behavior changes. They usually close their eyes and lie face down, pressed tightly against the wall or headboard of the crib and unwilling to move. Older children do not want to get out of bed after suffering from illnesses.
As soon as you notice any unusual behavior in your child, you need to consult a doctor. Only he will be able to identify the causes and type of dizziness in a child and prescribe adequate treatment.
If this is not done in time, then a banal ailment can develop into a serious illness.
Headaches in children and adolescents
Headaches are the most common complaint of people, forcing them to go to medical institutions; patients of childhood and adolescence are among them. According to statistics, approximately 3-8% of children complain of cephalgia in preschool age; in adolescence, this figure increases sharply to 57-82%.
A child is able to qualitatively evaluate and differentiate his sensations only at the age of approximately 4-5 years. It is by this time that he psychologically develops the ability to correctly perceive and describe the nature and location of pain. Earlier manifestations of pathology can be indirectly recognized by parents by the behavior, complaints and behavior of their children.
In most cases, attacks of cephalalgia in children have a favorable treatment prognosis, provided that the parents consult a doctor in a timely manner, the diagnosis is correctly established and appropriate therapy is prescribed.
On the one hand, intense vegetative symptoms (nausea, vomiting, dizziness, drowsiness, pallor, etc.) accompanying pain cause excessive concern for parents who seek to exclude severe head diseases (for example, brain tumor) and are overprotective of their children. On the other hand, there is an opinion that sometimes a child may have a headache and this is associated with adolescence and this situation does not require special attention and treatment.
Of course, complaints of headaches in “transitional” age indicate that in the process of age-related adjustment, the body and its functional-adaptive systems cannot cope with increased loads and signal this. Consequently, the child still needs immediate and qualified assistance from a specialist.
Frequent absences by a child from classes at school, sports clubs and restrictions on his active activities due to cephalgia leads to his falling behind the general education program and negatively affects his psychological and mental state, communication with peers.
At the same time, generally available preventive measures (regular and nutritious meals, walks in the fresh air, adequate physical activity, avoidance of overwork, overexcitement, lack of sleep, dehydration, etc.) in combination with proper drug therapy contribute to the treatment and prevention of certain forms of headaches.
Main types of cephalgia
In children and adolescents, just like in adults, headaches are divided into primary and secondary. Primary pain is an independent pathology not associated with any other disease. Secondary or symptomatic - are a consequence of somatic pathologies or underlying diseases of the central nervous system.
The most common primary cephalgia of the younger generation are migraines and tension headaches. Most often they are caused by hereditary factors, that is, they are present in the family history and have specific signs and complications unique to them.
Migraines are characterized by paroxysmal throbbing pain of severe intensity in one part of the head (bilateral pain is much less common). In most cases, there is an alternation of sides of localization of sensations. As a rule, attacks occur 1-2 times a month, less often - 3-4 times, with a duration of 30 minutes to several hours.
Pain can occur unexpectedly at any time of the day; left-sided migraines are more often observed in the morning. Attacks are accompanied by nausea, vomiting, dizziness, photosensitivity and noise sensitivity, vegetative symptoms (redness or pallor of the face, swelling of the eyelids, tearing, pupil dilation due to pathology, etc.).
Often, a painful attack is preceded by an aura in the form of dizziness or a sensation of rotation of the surrounding space, visual disturbances (flickering spots, light spots, blurred images), paresthesia, numbness of the head and/or face, and speech impairment. Physical activity increases discomfort and causes unbearable pain.
Tension headaches are characterized by a dull, pressing or squeezing sensation and are of moderate intensity. During the day, the nature of the pain and its intensity may change. The localization of cephalgia is bilateral, the frequency of attacks is noted from 1-3 times a week to daily. The duration of the attack varies from 30 minutes to several hours, days or even weeks with varying intensity.
Tension headaches usually occur in the afternoon, in schoolchildren after 5-6 lessons. Does not depend on physical activity, may be accompanied by dizziness, fatigue, depressed mood, anxiety, and nervousness. With increased pain, photo and sound phobia, anorexia are observed, and much less often - pallor, nausea, and vomiting.
The most common causes of secondary headaches in children are: sinusitis, middle ear infections, systemic infectious diseases, blood pressure disorders (hypertension or hypotension), traumatic brain injuries and other diseases. Sometimes there are cases of meningitis, encephalitis, the development of intracranial tumors of various etiologies, and even less often - the occurrence of cephalgia while taking certain medications that provoke vasodilation or vasoconstruction (expansion or narrowing of the lumen of the blood vessels of the brain).
Diagnostics
In addition to basic studies and analyzes that influence the choice of treatment and prevention tactics in children suffering from headaches, additional diagnostic examinations can be used.
Electroencephalography in children with the primary form of cephalgia is nonspecific. The study observed: a weakening of the severity of alpha rhythms in the occipital zone of the head and a decrease in the amplitudes of bioelectrical activity.
In some patients, the study reveals epileptic focal changes, both in a static state and during exercise. At the same time, the majority of children with benign epileptiform activity detected on electroencephalography do not have epileptic seizures, but complain of frequent episodic headaches.
In this case, drugs from the group of anticonvulsants can be considered as preventive measures.
Doppler ultrasound makes it possible to judge cerebral hemodynamics (blood movement through the vessels), including venous. It is the disturbances of venous blood flow that influence the nature and course of primary headaches. For example, significant venous dysfunction is found in approximately 87% of children suffering from migraines with aura.
For the prevention and treatment of such headaches, it is recommended to prescribe venotonic drugs.
A consultation with an ophthalmologist allows not only to determine visual acuity, but also to examine the condition of the fundus in order to exclude the diagnosis of intracranial hypertension.
Another cause of chronic persistent headaches in adolescents is visual impairment or improper correction. In this case, cephalalgia appears in the last lessons and the sensations are of a tightening or squeezing nature in the form of a hoop placed on the head.
The pain is localized, as a rule, in the frontal and temporal areas. This happens due to prolonged stay in an unnatural position (with the head lowered or thrown back) in combination with overstrain of the eye muscle fibers (squinting with myopia or farsightedness, astigmatism).
Adolescents and children with visual impairments can help get rid of headaches with well-chosen glasses and a well-lit and equipped workplace.
Factors that cause migraine attacks in children
Migraine is a chronic disease of the body characterized by periodically recurring attacks of intense cephalalgia.
In children of primary and preschool age, pain is bilateral; a unilateral pattern of pain is acquired in adolescence or young adulthood. At the same time, girls experience migraine attacks almost twice as often as boys. This is due to hormonal changes and in most cases, migraine attacks are triggered by menstrual cycles.
Factors (triggers) that provoke migraine in children:
Modifiable:
- Emotional stress:
- psychologically unfavorable situation in the family;
- conflict between parents;
- conflict between parents and child;
- worries and worries about grades or relationships at school;
- conflict with peers.
- Physical exercise:
- overwork;
- muscle overload;
- feeling hungry due to insufficient or irregular nutrition;
- dehydration.
- Rest and/or sleep disturbances:
- lack of sleep;
- sleeping too much on weekends.
- Climatic and external influences:
- heat, being in a stuffy room, cold;
- unpleasant odors;
- continuous noise;
- too bright light;
- vestibular loads.
- Eating disorders:
- excessive consumption of coffee, strong tea, carbonated drinks containing caffeine;
- frequent consumption of products containing artificial sweeteners (aspartame), nitrate preservatives (hot dogs, smoked meats, etc.), monosodium glutamate (used in large quantities in Chinese cuisine), tyramine or phenylethylamine (dark chocolate, cocoa, nuts, hard cheeses etc.);
- drinking alcohol, especially red wine and beer;
- eating large quantities of citrus fruits, bananas, avocados, raisins, prunes, etc.
Uninfluenced:
- External influences:
- sudden changes in weather conditions;
- sudden changes in climatic zones;
- unfavorable environmental conditions (radiation, air pollution with sulfur dioxide, nitrogen dioxide or carbon monoxide).
- Hormonal changes in the body (decrease in estrogen levels before menstruation in girls).
Of course, not every child is equally exposed to all of the above triggers, so parents are advised to keep a diary that will display the duration of attacks, their intensity, accompanying symptoms, food eaten the day before, psychological state (stress, conflict), etc.
Precursors of migraines in young children
Signs that your child may suffer from migraine attacks in the future include:
- Abdominal pain, which is characterized by repeated attacks of dull pain in the abdomen. Cutting or moderate aching pain occurs mainly around the navel, duration - from 1 to 72 hours. As a rule, abdominal pain is accompanied by anorexia, pale skin, nausea, vomiting, possibly diarrhea, a feeling of coldness or tingling in the fingers. In such a case, it is important to differentiate the diagnosis and exclude gastroenterological pathologies, infectious infection or an epileptic attack.
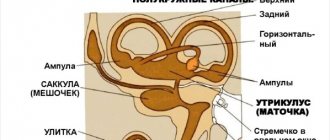
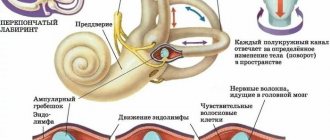
- Benign paroxysmal dizziness, characterized by repeated short-term (from several minutes to several hours), suddenly appearing and suddenly disappearing episodes of dizziness. In some cases, they are accompanied by nystagmus, vomiting, and throbbing headache. Moreover, in the period between attacks, studies of neurological abnormalities, vestibular functions and audiometry, electroencephalography data do not reveal pathologies.
- Cyclic vomiting syndrome is a condition in which a child experiences at least 5 discrete paroxysms of vomiting, each of which is accompanied by 4 episodes within one hour. The average duration of attacks is from 1 hour to 48 hours, the frequency is no more than 2 episodes per week. In the period between attacks (duration 2-4 weeks) there are no complaints about the child’s poor health. This condition can be combined with nausea, abdominal pain, headaches, discomfort during physical activity, and increased sensitivity to loud sounds and light.
Prevention of migraines in children
Preventive therapy for migraines in children begins with non-drug measures, which consist of:
- compliance with the daily routine;
- full sleep with going to bed at the same time, lasting at least 8-10 hours;
- nutritious and regular nutrition, sufficient amount of water (at least 1.5 liters);
- exclusion of physical and mental stress, stressful situations;
- training in relaxation and relaxation techniques;
- regular sports or physical exercise with moderate loads, but training during an attack increases the pain;
- avoiding foods that can cause an attack;
- avoiding long periods of time in front of a computer monitor or TV;
- formation of normal self-esteem in the child, despite the fact that he is tormented by headaches (so that the child does not feel sick, helpless and unable to lead a normal life);
- Keep a diary of the child’s well-being and pay attention if the headache is accompanied by anxiety, depressed mood, or, conversely, irritability and report this to the attending physician.
Treatment of migraines
Although preventative measures have shown good results in the treatment of migraines in children, most still require pharmacological therapy. It is mainly aimed at relieving headaches and eliminating symptomatic signs (regularly taking medications that reduce the frequency of attacks).
Symptomatic drug therapy is recommended for frequent, prolonged (3 or more days per month) and severe attacks, accompanied by significant impairment of well-being, health and limitation of daily physical activity.
Preventive symptomatic treatment is prescribed to children and adolescents during the interictal period with one of the drugs (depending on the individual characteristics of the disease) belonging to the following pharmacological groups:
- Beta blockers (Propranolol, Atenolol, Nadolol). The drugs act indiscriminately on adrenergic receptors, weakening the sympathetic impulses of the heart and lowering blood pressure. The drugs are not recommended for bronchial asthma; they can also cause side effects such as arterial hypotension, asthenia, sleep disturbances, and bradycardia. Not addictive.
- Calcium channel blockers (Verapamil, Nifedipine, Cinnarizine). The drugs have the ability to reduce the resistance of the walls of resistant vessels (arterioles) of the brain by reducing the tone of smooth muscles and reducing the response to vasoconstrictors (adrenaline), as well as prevent hypoxia of neurons, relieving neurogenic inflammation. Side effects of drugs (hypotension, bradycardia, dizziness, nausea, constipation) are observed quite rarely.
- Antihistamines (Peritol, Cyproheptadine) block H1 receptors and calcium channels, have anticholinergic and antiserotonin effects (reduce spasms). The drugs are recommended for children who have frequent migraine attacks combined with atopic dermatitis (allergies) or sinusitis. Medicines in this group can cause severe drowsiness, sedation, and weight gain.
- Antidepressants (Amitriptyline, Glycine) affect the metabolism of serotonin, norepinephrine, dopamine, and quickly relieve pain during migraines. Substances may cause side effects such as drowsiness, dizziness, dry mouth, memory impairment, speech impairment, and gastrointestinal dysfunction.
- Anticonvulsants (Valproate, Topiramate) affect nociception, reduce the activity of sodium ion channels (stabilize neuronal membranes) and modulate the activity of calcium ion channels, that is, they modulate neuronal excitability at the level of biochemical connections. The negative effect of the drugs affects the condition of the hair and epithelial tissues, the functionality of the digestive system, and sometimes provokes sedation and paresthesia.
Tension headaches in children
Due to the fact that tension headaches differ from migraines in their low intensity, not so severe accompanying symptoms and practically do not limit the daily activity of children, parents and patients themselves practically do not pay attention to them. Although, according to statistics, tension headaches are much more common in children than migraines. In early childhood, they are mainly episodic (less than 15 attacks per month are observed) and in adolescence they become chronic (more than 15 episodes per month).
Tension headaches are provoked by chronic psycho-emotional overload, stress, conflict situations that cause uncontrollable muscle spasms, blocks, clamps, tonic tension of the pericranial muscles (frontal, temporal, occipital). This is a kind of protective reaction of the body to the influence of constant external negative factors.
A similar reaction of the muscular system is caused by prolonged stay or work in a static, uncomfortable or non-physiological position, excessive overstrain of the neck, spinal, and eye muscles when working at a desk or computer, and an uncomfortable position during sleep. In most cases, there is a family history of similar cephalgia in the child’s parents or immediate relatives.
Typically, pain occurs in the morning after waking up and changes its nature, intensity and location (migrate from one side to the other or cover the forehead) during the day. They do not depend on daily and habitual physical activity, but react acutely to eye strain or mental fatigue.
Most children describe an undulating course of the attack with short moments of remission, the absence of transient neurological symptoms, but an increase in the level of anxiety, groundless fear, depressive states, and depressed mood.
Diagnostics
For tension headaches, its effectiveness was confirmed by an electromyographic study of biofeedback connections of the frontal muscle groups. Stressful situations or their threat cause an increase in muscle tone in the body and an increase in the electrical activity of muscle tissue, which is displayed on electromyography.
The person himself feels and is aware of only muscle tension during movements; other deviations remain below the threshold of perception. Familiarizing the patient with information about the electrical activity of certain muscle groups allows him to achieve greater results from relaxation, improve his psychological state and at the same time normalize blood pressure, respiratory and heart rhythms, and heart rate.
Therapy for such headaches should begin with reducing or eliminating the child’s exposure to a psycho-emotional or stressful situation. Tension cephalalgia does not completely deprive them of working capacity or physical activity, but causes them constant emotional discomfort, chronic fatigue, weakness, bad mood, which further aggravates the situation.
One of the main pathogenetic factors of tension headaches in children and adolescents is disturbances in the regulation of cerebral circulation. Doppler ultrasound helps to identify pathology and track the dynamics of changes in indicators during treatment.
Treatment and prevention of tension headaches
Prevention and treatment of tension cephalgia consists of a combination of drug therapy, which is aimed at correcting the mental and emotional state, eliminating muscle tension, as well as non-drug measures. These include physiotherapy, massages, baths, swimming, sports, optimization of the daily routine, good nutrition, arrangement of the workplace (desk, table, chair) and rest areas (orthopedic mattress, pillow), etc.
Medicines (painkillers) for episodic tension cephalgia are prescribed for a single dose or in short courses. Overusing analgesics in children and adolescents with chronic pain or mixing multiple types of drugs usually has the opposite effect. A similar result in combination with gastrointestinal dysfunction occurs when using stronger analgesics or their combinations with muscle relaxants (muscle relaxants).
For chronic tension pain, preventive therapy, which is carried out in the intervals between attacks, becomes much more important. For example, taking a course of Amitriptyline (an antidepressant with an analgesic effect), anticonvulsants, muscle relaxants to relieve muscle tension in the occipital and pericranial muscle groups.
Children suffering from tension headaches, as well as from migraines, often experience symptoms of cerebrasthenic syndrome, the main symptom of which is “irritable weakness.” On the one hand, such children are slow, passive, lethargic, quickly get tired and exhausted even with minor physical and mental stress, are constantly in a depressed mood and do not cope well with school memory tasks.
On the other hand, they experience increased irritability, affective outbursts, excessive criticism and a desire to constantly argue. In such a situation, the main thing for parents to remember is that their children are not lazy, stubborn, or have entered adolescence, but that they need medical help. Such children are contraindicated from excessive stress, prolonged stay in a group of peers, they need drug therapy and in no case should parents condemn them or scandals. From stressful situations in the family, headaches will torment the child much more often and more severely, and cerebrosthenic syndromes will worsen.
Another direction has confirmed its effectiveness in the treatment of tension headaches in children and adolescents - therapy with metabolic drugs.
They help improve metabolic processes in the brain, activate and increase the resistance of the central nervous system to various stresses, have anti-asthenic (asthenia - chronic fatigue syndrome) properties, and improve memory. Such drugs include: riboflavin (vitamin B2), coenzyme Q10, drugs containing magnesium, nootropic substances (for example, Actovegin). Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
For what symptoms should you contact an ENT specialist?
Manifestations of the disease depend on its type, but common ailments include:
- earache;
- the appearance of discharge from the ear canal (may be purulent);
- hearing loss and congestion in the ears;
- redness of the visible part of the ear;
- general weakness, drowsiness, headache, dizziness, tinnitus, increased temperature.
With external otitis, redness, swelling, severe pain in the ear, pain when moving the jaw, itching, and discharge from the ear are visible.
With otitis media, the pain is throbbing and shooting, can spread to the teeth and head, hearing decreases, nausea, vomiting, fever, and general weakness may occur. A characteristic symptom of otitis media is autophony - the sound of a person’s own voice in the diseased ear.
With internal ear inflammation, the main symptom is severe paroxysmal dizziness. They can appear when changing body position and sharp turns of the head. There is usually no pain, but nausea and vomiting may occur.
What does the nature of vomiting indicate?
In all cases of vomiting, it is necessary to pay attention to the nature of the vomit:
- Vomiting blood
may indicate bleeding from a stomach or duodenal ulcer and is an indication for emergency treatment. Sometimes a person may not know that he has a peptic ulcer and the first symptom will be bleeding. In addition, vomiting blood occurs when bleeding from dilated veins of the esophagus in people with cirrhosis of the liver. - Vomiting blood mixed with foam most often indicates pulmonary hemorrhage.
- Vomit that is yellow or green in color and has a bitter taste indicates that it is bile. Vomiting bile indicates liver disease, gall bladder and often occurs after eating fatty foods.
Attention! In all cases of vomiting with blood (fresh or dark), the patient should be immediately shown to a doctor!
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |
Diagnostic methods
- Electrocardiography (ECG). After examining the printout, the doctor will be able to determine the type of tachycardia and see, for example, heart failure.
- Daily Holter monitoring is intended to detect paroxysmal tachycardia. Electrodes are attached to the baby's skin and connected to a compact device that takes readings around the clock. Sometimes it takes more than a day.
- Ultrasound of the heart (Echo-CG) - allows you to see the structure of the heart, structural abnormalities, visualize large vessels and heart valves and chambers, the thickness of the walls of the organ, and evaluate its contractile function. Ultrasound allows you to see heart defects.
- A clinical blood test aimed at detecting anemia. With it, a compensatory acceleration of heart rate occurs.
- Biochemical blood test for glucose levels and electrolyte composition.
- Blood test for thyroid hormones.
- Electroencephalography (EEG).
- MRI of the heart - in rare cases.
- Electrophysiological study (EPS) of the heart is necessary to evaluate electrical activity and find the source of impulses in the paroxysmal type of tachycardia.
Treatment of otitis media
Treatment includes the use of medications, physical therapy, and surgery.
Drug treatment is effective in the first stages of the disease and further when accompanied by physiotherapy and after surgery. Involves the use of the following medications:
- anti-inflammatory drugs;
- antibacterial agents: locally (in the form of drops, ointments) and systemically (injections, preparations for oral consumption);
- vasoconstrictor drugs in the nose to relieve swelling of the mucous membrane of the auditory tube.
Physiotherapeutic procedures help stop the process of inflammation, destroy infections and relieve severe pain. The following procedures can be carried out:
- laser therapy;
- tube-quartz;
- electrophoresis;
- phototherapy;
- ultraviolet irradiation.
Surgery is prescribed when medications and physical therapy have not shown the necessary effectiveness. There are two types of operations that are most often prescribed: tympanostomy or paracentesis. Both procedures involve cutting the eardrum to remove pus from the middle ear cavity. But with a tympanostomy, a small drainage (ventilation) tube is inserted into the eardrum. It is needed for a longer evacuation of secretions and the introduction of medications there. In some cases, other methods of surgical intervention may be chosen (sanitizing surgery on the cavities of the middle ear, anthromastoidotomy, tympanoplasty, balloon tuboplasty).