Dizziness is the second most common problem with which people turn to neurologists. It occurs only slightly less frequently than headaches. Moreover, the frequency of its occurrence increases proportionally with age, and women suffer from such attacks 2-3 times more often than men. But dizziness refers to quite different symptoms, from the sensation of rotation of surrounding objects or one’s body to darkening of the eyes, unsteadiness of gait, etc. And there are even more reasons for the occurrence of such disorders. One of the most commonplace is an increase or decrease in blood pressure. But if the tonometer readings are within the normal range (120/70) or close to it, you should look for the cause of dizziness elsewhere.
How to determine the cause of dizziness at normal blood pressure
Most often, finding out the cause of a patient’s health problems begins with collecting anamnesis and measuring blood pressure, since in most cases this allows you to immediately eliminate a whole range of disorders. The cause of dizziness without changes in blood pressure can be a rise to altitude, a long trip in a car or boat, or physical fatigue. In such situations, there is usually no threat to health and no need to see a doctor.
In other cases, it is necessary to differentiate systemic dizziness from non-systemic dizziness. In the first case, there is damage to the vestibular analyzer, i.e., the organ responsible for maintaining balance and adequate reactions of the body to changes in the position of the body or head. Non-systemic dizziness is caused by other diseases that are in no way related to the work of the vestibular analyzer.
With normal blood pressure levels and the absence of heart and vascular diseases, systemic (vestibular or true) dizziness is most often diagnosed. According to statistics, about 30% of people encounter it at least once in their lives.
A very important point in determining the cause of a disturbance in well-being is an accurate description of the sensations that arise during an attack. At the same time, it is important to try to avoid the word “dizziness” and talk in as much detail as possible about the feelings that arise.
Systemic vertigo is characterized by the presence of various illusions of movement. This may be a feeling:
- rotation of the body in space or vice versa of environmental objects;
- rocking the bed on which the patient is lying, rocking in a boat, falling into space;
- the ground leaving under your feet, the ceiling collapsing, etc.
With systemic dizziness, which occurs with normal blood pressure, there is no sensation of darkening in the eyes, flickering of spots, fog in the head, lightheadedness, or unsteadiness. Such symptoms indicate the non-systemic nature of the disorder and the need to search for causes in pathologies of other organs, not excluding the heart and blood vessels. After all, during an examination, blood pressure may be normal, but sharply fall or rise in response to a specific trigger.
The main distinguishing feature of systemic vertigo is nystagmus - rapid, involuntary movements of the eyeballs.
Causes of systemic dizziness
Systemic or vestibular vertigo may be central or peripheral. In the first case, the reason lies in damage to the corresponding nuclei of the brain stem and its vestibular centers, disruption of vestibular connections, which is typical for:
- circulatory disorders in the vertebrobasilar system, accompanying a transient ischemic attack or stroke, which is often observed in diseases of the spine and cervical osteochondrosis in particular;
- vestibular migraine;
- multiple sclerosis.
When the central part of the vestibular analyzer is damaged, the severity of symptoms increases smoothly. They are not very pronounced, but can persist for several days or even weeks. In such cases, headaches, visual disturbances, inability to walk and falls are also often observed.
Central vestibular vertigo accounts for 12% of all cases of patients visiting doctors with similar complaints.
In case of peripheral vestibular vertigo, the problem should be sought in damage to the vestibular analyzer or nerve. In such situations, it may consist in the development of:
- benign paroxysmal positional vertigo (BPPV);
- Meniere's disease;
- vestibular neuritis;
- bilateral vestibulopathy;
- neurovascular conflict, etc.
There is a whole range of other peripheral causes of dysfunction of the vestibular analyzer, but they are much less common - less than 0.5% of cases. But almost always, when the vestibular analyzer or nerve is damaged, the attack begins acutely and lasts no more than a day. It is characterized by a sudden onset of a pronounced sensation of rotation. This may be accompanied by nausea and even vomiting, tinnitus and hearing loss.
Causes of non-systemic dizziness
Dizziness while maintaining normal blood pressure levels can be provoked by:
- inflammatory processes of the ear;
- following a strict low-carbohydrate diet;
- Iron-deficiency anemia;
- taking certain medications;
- endocrine disorders, including diabetes mellitus;
- infectious diseases accompanied by a significant increase in body temperature.
But in such situations, patients are usually aware of their problem and the possibility of dizziness. The only exception, perhaps, is iron deficiency anemia, which provokes increased fatigue. But to diagnose it, it is enough to take a general blood test.
When dizziness occurs against the background of normal blood pressure, its psychogenic origin cannot be excluded. This is observed in 15% of cases and therefore deserves special attention.
Methods for treating heaviness in the head
As already mentioned, heaviness in the head in itself is not a disease. This is only a symptom, and it is the root cause of this condition that needs to be treated.
Treatment of the underlying disease is specific, selected taking into account the individual characteristics of the patient’s body and entirely depends on the identified disorders.
However, symptomatic treatment of heaviness in the head and similar accompanying symptoms is also possible. Most often, non-steroidal anti-inflammatory drugs, analgesics, antispasmodics and other drugs are used in therapy to relieve discomfort. In some cases, they resort to blockades.
However, do not forget that long-term drug treatment is addictive, and the drugs lose their effectiveness over time. So this approach to treatment can be truly justified only in a situation where heaviness in the head is caused by serious organic lesions. In other cases, it is recommended to solve the problem, if possible, through safer therapeutic methods without the use of “chemistry”.
Thus, heaviness in the head can be easily eliminated with the help of self-massage of the biologically active zones of the back of the neck, the back of the head, the temporal region, and the crown. Impact on these areas not only relieves tension from the neck muscles, but also stimulates the flow of fresh blood, which helps improve well-being and restore performance.
In addition, you should pay attention to a number of treatment methods that have proven effective in improving blood flow in the cervical spine and normalizing blood supply to the brain. First of all, these include manual therapy and all kinds of physiotherapeutic procedures.
Physical therapy exercises can also give good results in the fight against heaviness in the head, drowsiness, fatigue and other associated symptoms. Physical activity helps saturate the blood and tissues with oxygen. In addition, regular performance of even simple exercises allows you to strengthen the muscle corset and, accordingly, reduce the load on the spinal column itself and protect it from the development of destructive processes.
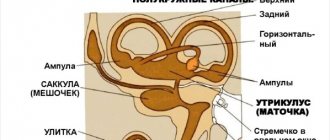
BPPV
BPPV is diagnosed in 17% of patients complaining of dizziness and is the most common cause of its occurrence. Moreover, the frequency of its occurrence increases in proportion to age, and in women it occurs 2 times more often. This is a disease in which otoliths move into the semicircular canals of the inner ear.
Otoliths are calcium carbonate crystals normally located in the otolithic membrane of the inner ear.
With BPPV, attacks are usually triggered by head movements, especially at night, when the patient cannot control himself. There are frequent situations when dizziness occurs after turning in a dream or getting up/getting out of bed. In this case, dizziness begins acutely, but lasts less than a minute, although it may be accompanied by nausea and vomiting, nystagmus. It is not associated with hearing loss, noise, or ringing in the ears.
The duration of the attack usually does not exceed several minutes.
In most cases, the causes of BPPV cannot be determined. Only in certain situations is its development associated with head injuries, ear surgeries, or previous diseases of the inner ear.
But on the other hand, BPPV does not require specific treatment and, as a rule, goes away on its own in a few weeks or months. Patients are only taught special maneuvers to facilitate the release of particles from the affected semicircular canal to eliminate dizziness. But before they are carried out, it is imperative to consult a doctor who will confirm or deny the presence of BPPV and determine its type. Otherwise, as well as if the technique is violated, your condition may worsen.
There are more than 5 different maneuvers to relieve an attack of dizziness due to BPPV. The choice of which one will be most effective for an individual patient depends on which part of the labyrinthitis his otoliths move to. In most cases, the Eple maneuver is recommended. Its essence is as follows:
- turn the head 45° towards the affected ear and lie on your back (this may be accompanied by increased dizziness);
- the head is turned sharply towards the healthy ear so that it is at an angle of 45°;
- continue turning to the healthy side with the whole body so that at the end point the face is directed downward;
- rise to a sitting position, maintaining a head tilt of 45°.
You should remain in each position for about 1 minute, and change them as abruptly as possible.
In half of the cases, correct implementation of therapeutic maneuvers allows for long-term elimination of BPPV symptoms. Although 25-50% of patients experience relapses. In such situations, repeated maneuvers are indicated.
Meniere's disease
According to statistics, Meniere's disease is diagnosed in 10% of patients who complain of dizziness. This is a disease of the inner ear, in which there is an increase in the volume of labyrinthine fluid and an increase in pressure within the labyrinthitis. Most often it occurs after 30 years.
Meniere's disease is characterized by episodes of systemic dizziness, which is associated with a progressive decrease in hearing acuity, tinnitus, and unsteady gait. Often there is also a feeling of stuffiness in the ear. In this case, hearing impairment manifests itself to a greater extent directly during an attack of dizziness, which can last from several minutes to a couple of hours. This is associated with nausea and vomiting.
A characteristic feature of Meniere's disease is the possibility of a so-called aura immediately before an attack. It may manifest itself:
- increasing noise in the affected ear;
- ear congestion;
- hearing impairment.
But the aura is not observed in all cases. Therefore, in its absence, the possibility of dizziness at normal pressure due to Meniere’s disease cannot be excluded.
When the pathology manifests itself, attacks occur frequently and initially their frequency increases. Over time, the trend reverses and dizziness bothers patients less and less.
During the disease there are 3 stages:
- Stage 1 – tinnitus is observed only periodically and is accompanied by a feeling of fullness and congestion, which leads to a decrease in hearing acuity. But at this stage, hearing between attacks is restored.
- Stage 2 – noise and congestion in the ears are constantly present, attacks become more frequent and occur almost daily. In this case, the dizziness is very intense, and hearing between attacks is practically not restored and can completely disappear.
- Stage 3 – the interval between attacks gradually increases, although hearing loss persists and is irreversible. There is also a constant feeling of unsteadiness and instability.
Initially, with Meniere's disease, only one ear is affected, but in 50% of patients, within several years, the second ear is also involved in the pathological process.
When diagnosing Meniere's disease, the main priority of treatment is to prevent the occurrence of attacks, since suddenly appearing intense dizziness significantly reduces the patient's quality of life, and in the early stages can deprive him of his ability to work due to the high frequency of episodes. For this purpose, patients are prescribed a salt-restricted diet, as well as individually selected drug therapy.
Vestibular neuronitis
Vestibular neuronitis or neuritis means inflammation of the vestibular root of the 8th pair of cranial nerves, i.e., the vestibular-cochlear nerve. It has not yet been reliably determined what exactly provokes the development of this disease. According to research, it is assumed that herpes virus infection type 1 is involved in this. This theory is also supported by the fact that most often neuritis manifests itself after suffering from an acute respiratory infection.
The disease is characterized by a sudden onset of severe dizziness with a sensation of rotation of surrounding objects, which tends to gradually weaken over time. But head movements or changes in body position provoke a deterioration in health. The attack is accompanied by nausea, vomiting, and nystagmus. In this case, the oscillatory movements of the eyes are directed towards the healthy ear. There is also an imbalance, with falls more often occurring on the side of the healthy ear. But vestibular neuritis is not accompanied by hearing impairment or neurological disorders.
Dizziness may last for hours or days, and unsteadiness may persist for a week or longer.
When diagnosing vestibular neuronitis, symptomatic therapy is indicated to alleviate the patient’s well-being. It is designed to eliminate nausea, vomiting and reduce the severity of dizziness. Specific drugs are selected by a neurologist individually, taking into account the characteristics of the patient’s condition and the nature of concomitant diseases. As a rule, the course lasts no more than 3 days.
It is also recommended to perform special visual exercises, head movements, walking and balance exercises. They need to be performed daily, devoting at least half an hour to exercise.
In most cases, the measures taken are sufficient to eliminate the disease and normalize the patient’s condition. Within a few weeks, central vestibular compensation occurs, which leads to the elimination of the symptoms of neuritis. But instability and difficulty maintaining balance, especially when moving the head, can persist for a long time. But in 15% of patients, after the symptoms of vestibular neuronitis subside, the development of BPPV is observed, and psychogenic dizziness often occurs.
Cephalgia in children
Pulsating discomfort in a child that is not accompanied by fever, cough and runny nose should alert parents. In such cases, it is important to consult a doctor. Such manifestations may indicate problems with the child’s health.
The phenomenon can be triggered by:
- disease of the vascular system;
- neuralgia;
- migraine;
- injury;
- emotional condition;
- poor nutrition;
- the presence of provoking external factors.
Bilateral vestibulopathy
Bilateral vestibulopathy refers to bilateral deficits in vestibular function, which is clinically manifested by:
- attacks of dizziness while moving with the illusion of rotation of the environment;
- instability;
- imbalances, especially severe in the dark and when walking on uneven surfaces;
- decreased visual acuity while walking and making head movements.
But all the symptoms are observed only when the person is in an upright position. If he sits or lies, there are no such violations.
Most often, bilateral vestibulopathy occurs as a result of taking medications, especially aminoglycoside antibiotics, as well as after suffering from infectious and inflammatory diseases of the brain and some other pathologies.
It is impossible to completely eliminate the disorder, but by performing a special set of exercises selected separately for each patient, it is possible to achieve the development of central vestibular compensation.
What to do?
It is almost impossible to independently determine the causes of frequent attacks of dizziness. Therefore, those who regularly experience vertigo are advised to go to an appointment with a therapist, or a neurologist. The specialist will carefully examine the patient’s complaints and prescribe diagnostic tests. If necessary, the doctor will refer the patient for consultations with an ENT specialist, an ophthalmologist, a cardiologist, or an endocrinologist.
To identify the causes of vertigo, the patient may be prescribed the following tests:
- Neurological tests. They allow you to assess the functionality of the vestibular apparatus.
- MRI or CT. Such brain studies reveal various disorders (hemorrhages, tumors, vascular pathologies).
- Ultrasound Doppler. Using Doppler ultrasound, the condition of the vessels of the head and neck is studied.
- Audiometry. Diagnostics allows us to assess hearing function.
- EEG. To study the activity of the cerebral cortex, the doctor will prescribe electroencephalography.
To quickly cope with dizziness (of course, if it is not caused by dangerous reasons), you can sit on any surface, relax a little and take 5-6 deep breaths. Be sure to open the window (if you are indoors) to provide fresh air. If the causes of vertigo are harmless, then such actions are quite enough for the dizziness to disappear without a trace.
Neurovascular conflict
In neurovascular conflict, episodes of dizziness are caused by compression of the 8th pair of cranial nerves by an abnormally located blood vessel. As a result, the myelin sheath of the nerve becomes thinner, which leads to its constant stimulation by the vessel and overexcitation of the vestibular nucleus.
This is accompanied by short attacks of dizziness, which usually occur with a certain position of the head. This is often associated with tinnitus and hearing loss. In this case, episodes of dizziness can bother the patient several times a year, or 2-3 times a day.
For frequent, severe attacks, patients are prescribed specific drug treatment. If in response to it there is a decrease in the number of attacks, a decrease in their severity and duration, this serves as additional confirmation of the presence of a neurovascular conflict. In such situations, MRI is highly recommended. If its results confirm the diagnosis, it is worth performing surgery to decompress the vestibular-cochlear nerve as early as possible before hyperactivity of the vestibular nucleus develops.
Vestibular migraine
Migraine is a widespread disease, the manifestations of which are very diverse. Most often, in addition to dizziness at normal blood pressure, migraine is accompanied by a severe headache. As a rule, it is one-sided, pulsating and can persist for several minutes, hours, or several days. Often during an attack there is increased sensitivity to light and sounds.
Some patients notice the appearance of an aura before the onset of a migraine. In most cases, it consists of the occurrence of visual disturbances: loss of visual fields, flickering of spots in front of the eyes, luminous lines, etc. The aura usually appears an hour or less before the onset of the attack, and then disappears without a trace.
Migraines are more often diagnosed in women, and episodes of dizziness may be directly related to the phase of the menstrual cycle.
Treatment is carried out with medication. Usually, to eliminate pain and dizziness, the same medications are prescribed as for classic migraine. If attacks occur frequently, basic therapy is selected that is appropriate to the situation. All patients are also advised to avoid stress, eat right, normalize their work and rest schedule, and regulate the amount of physical activity.
Diagnostic methods
The cause of dizziness can be determined through a thorough examination, which includes:
- blood chemistry;
- radiography of the cervical vertebrae;
- vascular ultrasonography;
- magnetic resonance;
- electrocardiogram.
After deciphering the research data, you will need the help of highly specialized specialists:
- neurologist;
- otolaryngologist;
- ophthalmologist;
- cardiologist.
Holter monitoring is also performed. This is a popular way to examine the heart. The procedure resembles a traditional electrocardiogram, but unlike it, the Holter method records changes that occur during the usual daily routine. The following are under surveillance:
- Emotional and physical stress.
- Duration of sleep and wakefulness.
- Other details that the doctor does not always pay attention to when talking with the patient.
Based on the data obtained, the specialist makes a conclusion about the presence of arrhythmias and insufficient oxygen supply to the heart muscle. The effectiveness of dizziness treatment is also under control.
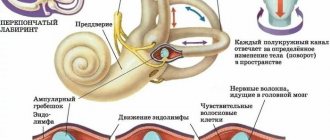
The vestibular, tactile and visual systems are responsible for the correct spatial orientation of a person. When the signal to the brain is disrupted, vertigo forms.