Definition
Benign paroxysmal positional vertigo (BPPV) occurs in repeated episodes, often lasting less than one minute. Attacks are triggered by changes in head position: turning, throwing back, as well as changes in body position, including lying down, even in sleep. Between attacks, autonomic disturbances (nausea, rarely vomiting, fluctuations in blood pressure, sweating) and imbalance may persist, so patients may describe constant dizziness.
Over time, the severity of attacks usually decreases. The word “benign” means that the disease goes away on its own, without treatment, without causing lasting harm to the patient.
BPPV is the most common type of dizziness. Attacks most often develop in older women. However, the disease can occur at any age.
Attacks of BPPV, in most cases, are associated with separation, destruction or increase in size of the otoliths.
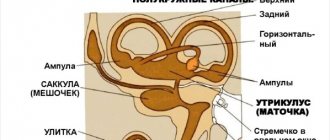
Otoliths (otoconia) are layered pebbles consisting primarily of calcium carbonate crystals, like mother of pearl or nacre. They are immersed in a jelly-like layer that envelops the hairs of sensitive cells on the surface of the macula (macula) of the spherical and eleptic sacs of the vestibular analyzer. The otoliths, the jelly-like layer and the hairs of sensory cells form the otolithic membrane.
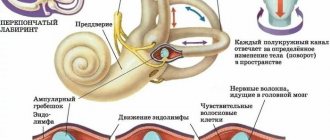
The elliptic sac (uterus) connects to three semicircular tubules (SCC), located in three perpendicular planes: lateral, anterior and posterior. In their extensions at the junction with the uterus, there is also a sensitive area - the ampullar ridge, covered with a structure similar to the otolithic membrane - the cupula. Normally, the cupula separates the RCC and the utricle. It does not contain otoliths. The cupula provides the perception of angular accelerations of the head, responding to changes in pressure in the ampulla arising due to the inertia of the endolymph (the fluid that fills the RCC and the sacs of the vestibular analyzer).
Detached otoliths or fragments thereof may enter the ampullae of the RCC and irritate the cupular areas. This more common variant of BPPV is called canalithiasis.
Thanks to the balance between the formation and resorption of the layers that make up the otoliths, their renewal is ensured, as well as the resorption of detached otoliths. When the balance is disturbed, one of the otoliths becomes large (2-4 times larger than neighboring cells); the large mass leads to greater displacement compared to neighboring fixed otoliths, which is a source of irritation of the vestibular system. This variant of BPPV is called dome lithiasis; it is characterized by a longer course (several months) and lack of effect from vestibular maneuvers.
Asymmetrical signal input to the brain during unilateral stimulation of the vestibular apparatus disrupts the illusion of balance created by the interaction of the vestibular, visual and proprioceptive systems (receiving signals from muscles and ligaments, assessing the position of limb segments). There is a feeling of dizziness.
Sensitive cells of the vestibular analyzer send a signal of maximum intensity to the brain during the first second of stimulation, then the signal strength decreases exponentially, which underlies the short duration of BPPV symptoms.
The most common lesion is the posterior SCC (90%), less often the lateral one (8%), the remaining cases are caused by damage to the anterior SCC and combined damage to several tubules. Classic cases of BPPV due to posterior RCC involvement are idiopathic in 35% of cases, with previous traumatic brain injury (sometimes minor) and whiplash in the neck occurring in 15% of patients.
In other cases, BPPV is caused by other disorders: most often Meniere's disease (30%), vestibular neuronitis, surgical interventions on the organ of hearing, paranasal sinuses, herpetic lesions of the ear ganglion and circulatory disorders of the structures of the inner ear. Population studies have revealed a direct relationship between the likelihood of developing BPPV and age, female gender, migraine, giant cell arteritis, risk factors for cardiovascular complications - arterial hypertension and dyslipidemia, as well as a history of stroke, which confirms the importance of vascular causes in some cases.
Lindsay-Hemenway syndrome has been identified - acute dizziness, followed by the development of BPPV attacks and a decrease or complete disappearance of nystagmus in the caloric test due to circulatory disorders in the anterior vestibular artery system.
The diagnosis of BPPV is made based on the assessment of nystagmus during special maneuvers - techniques that cause angular accelerations of the patient's head.
Types of dizziness when lying down
Dizziness when turning the head while lying down in a relaxed position varies in the nature of its manifestations depending on the type of disorder. Some patients complain of a sudden feeling of lightness, some feel the rotation of the surrounding space. Doctors distinguish two main types of dizziness when turning the head in a lying position - true or systemic and non-systemic.
Among peripheral vestibular disorders, up to 35% are benign paroxysmal positional vertigo.
The disease develops due to the entry of otolith fragments into the posterior semicircular canal, which causes its irritation and the appearance of a characteristic clinic.
Neurologist
Pershina Natalia Sergeevna
8 years of experience
Unsystematic dizziness
This type of dizziness when turning the head in a lying position is accompanied by deterioration in concentration, blurred thoughts, and lack of balance. Many patients complain of fainting sensations. With such symptoms, the first place in the list of possible causes of the disorder is occupied by psychogenic factors, a malfunction of the endocrine or cardiovascular system.
Systemic dizziness
This type is diagnosed if severe dizziness when changing body position while lying down or sitting occurs with a linear displacement of space relative to one’s body or an imaginary displacement of objects or planes. Symptoms occur when the peripheral zone of the vestibular apparatus is damaged - disruption of the inner ear, vestibulocochlear nerve.
Dizziness that appears after a sudden change of position does not cause any concern.
You should take them much more seriously when they arise at rest. They often indicate a violation of the vestibular apparatus, changes in blood pressure, vascular atherosclerosis, brain tumors and other disorders.
This symptom is an indication for urgent examination and treatment.
If, with normal blood pressure, vertigo is often bothersome at rest, damage to the parts of the brain responsible for the functioning of the vestibular system must also be excluded.
A common type of systemic vertigo when lying down is benign paroxysmal positional vertigo (abbreviated as BPPV). It is detected in a quarter of patients. The difficulty of diagnosis is due to the similarity of symptoms with manifestations of osteochondrosis and acute cerebrovascular accident.
What is BPPV associated with?
The reason why you feel dizzy when you turn your head while lying down is the movement of microscopic crystals of calcium carbonate - otoliths. Normally, the pebbles form part of the otolith receptor, located at the entrance to the inner ear. The sensation of rotation occurs when some of the crystals leave their place, moving into the horizontal semicircular canal. In the medical community they talk about the development of canalithiasis.
Sharp dizziness when turning the head in a lying position is accompanied by nausea, vomiting, a feeling of heat, and increased heart rate may occur.
Treatment of discomfort
There is no need to self-diagnose and try to determine why your head hurts and feels dizzy. Only the attending physician will be able to correctly determine the cause of the ailment and prescribe the correct treatment to the patient.
Therapy for the disease directly depends on the characteristics of its course. Dizziness cannot be treated on its own - in order to get rid of this unpleasant symptom, it is imperative to identify the main cause of its occurrence and eliminate it as soon as possible. Treatment of the disease may include both non-drug treatment methods and medications:
- Carrying out manual therapy. It is very important that such therapy is carried out only by a professional specialist, otherwise it will be difficult to avoid complications.
- Reflexology and physiotherapy. In reflexology, the doctor performs acupuncture, which is especially effective for certain types of pathologies.
- Application of the Shants splint.
- Health-improving physical education.
- Use of medications. Depending on the type of lesion, medications may be prescribed to improve brain function, strengthen the walls of blood vessels, etc.
In severe cases, the specialist prescribes therapy from several methods to the patient at once. This treatment allows you to get faster results in the fight against pathology.
The development of dizziness in a horizontal position may directly indicate the presence of a serious illness. Therefore, it is very important to consult a doctor at the initial stage of pathology and carry out a comprehensive diagnosis to find out its causes.
Self-medication in this case can lead to serious problems - the real disease will begin to progress noticeably, and the patient’s condition will only worsen.
Causes
Severe dizziness when turning your head while lying down is not normal. It speaks of problems in the body.
Dizziness and nausea in the morning
Dizziness and nausea are natural physiological responses to mental and physical fatigue.
List of possible causes of dizziness when turning the head while lying down:
- Change in blood pressure. The head may feel dizzy with hypotension (low blood pressure) and hypertension (high blood pressure). In both cases, the walls of blood vessels change, blood flow is disrupted and the nutrition of brain cells deteriorates.
- Disorders of the vestibular apparatus. It is he who is responsible for a person’s orientation in space. Dizziness occurs due to injury or tumor of the vestibular nerve, or when it is damaged by bacterial and viral infections.
- atherosclerosis . In this disease, blood flow to the brain is impaired due to cholesterol plaques in the arteries. The cells are poorly saturated with oxygen, and a person experiences severe dizziness when changing body position from lying to sitting.
- Inflammation of the inner ear (labyrinthitis, otitis media).
- Sinusitis.
- Dehydration of the body.
- Strict diets and fasting.
- Meniere's disease is an accumulation of fluid in the middle ear that irritates the vestibular system.
- Traumatic brain injury and concussion .
- Degenerative-dystrophic changes in the cervical spine lead to oxygen starvation of cells. The arteries are pinched by the spinal discs and impede the flow of blood to the cells.
- Migraine. These are severe headaches that are often accompanied by dizziness.
- disorder . Powerful short-term or long-term stress causes a sharp surge of adrenaline, it can knock the ground out from under a healthy person.
- Iron-deficiency anemia. This disease leads to oxygen starvation of all cells of the body.
- Hypothyroidism of the thyroid gland. In rare cases, it can cause disorientation in space and severe dizziness when turning the head in a lying position.
- Benign positional paroxysmal vertigo (BPPV). Occurs when the otolith organ of the ear is damaged, which regulates the balance and concentration of the body in space. The head begins to feel dizzy when turning to the side or bending over.
It is important to know: severe dizziness when turning your head while lying down can indicate a serious pathology - a brain tumor. In this case, timely contact with a doctor can save your life.
Distinctive signs of dizziness
The content of the article
Dizziness can occur for various reasons. If it occurs only once, it may indicate poor health, which will pass after some time. In the case when such a symptom occurs repeatedly, a mandatory consultation with the attending physician and a more comprehensive examination is required to determine the cause of the negative symptoms.
If a patient experiences dizziness when taking a horizontal position, this may indicate pathological changes in his body, which are very important to identify in a timely manner and begin to treat correctly. In a supine position, this condition is detected by the following signs:
- a feeling of the movement of things around, a change in the spatial position of the ceiling or walls;
- very often, with regular attacks, a person experiences a persistent feeling of anxiety before going back to bed;
- a feeling of rotation of one’s own body (sometimes it haunts a person even at night), begins to feel sick when lying down;
- Vomiting and pain in the head appear.
In addition, the attack may intensify with a change in position - turning the head, a sudden change in body position. Increasing the symptom can provoke increased weakness, which haunts the person throughout the day.
Associated symptoms
During an attack, a person may feel like the room around them is spinning. His sense of balance is disturbed, his palms and feet may sweat, and he may experience nausea and dry mouth.
If you experience dizziness when turning your head while lying down, it is important to pay attention to the accompanying symptoms:
- If you have a severe headache, nausea and vomiting do not stop, your gait becomes unsteady, or you faint, you should immediately call an ambulance. Such symptoms are characteristic of a stroke - a cerebral hemorrhage, which, if help is not provided in time, often leads to death. Signs of a stroke also include problems with speech, coordination, and a sudden and prolonged attack of dizziness.
- With hypotension, the following symptoms may appear: lethargy, immobility, general deterioration of the condition, attacks of severe dizziness when lying down.
- During a hypertensive crisis, the patient's pulse quickens, severe nausea and headache occur.
- Otitis media and diseases of the inner ear are accompanied by symptoms such as tinnitus, purulent discharge, and hearing impairment.
- Increased dizziness when turning the neck and walking, disorientation in space, a crunch in the neck are signs of degenerative changes in the cervical spine.
- tumor is characterized by a gradual increase in dizziness, headache and hearing loss.
- With sinusitis , attacks are mild, dizziness occurs when turning and bending.
- With a viral disease, the patient experiences severe weakness, chills and fever.
The same symptoms can be the result of different diseases, so to determine the root cause of the attacks, it is important to consult a doctor. First of all, you need to be examined by a therapist.
Dizziness: causes and treatment
(from the book Neurology. G.D. Weiss. Edited by M. Samuels. Translated from English - M., Praktika, 1997. -640 p.)
Dizziness is one of the most common and at the same time one of the most “disliked” complaints by doctors. The fact is that dizziness can be a symptom of a wide variety of neurological and mental diseases, diseases of the cardiovascular system, eyes and ears.
I. Definition. Since patients can call a variety of sensations “dizziness,” during the interview it is necessary first of all to clarify the nature of these sensations. They can usually be classified into one of four categories.
A. Vestibular dizziness (true dizziness, vertigo) is usually caused by damage to the peripheral or central part of the vestibular system. It manifests itself as the illusion of movement of one’s own body or surrounding objects. In this case, sensations of rotation, falling, tilting or swaying occur. Acute dizziness is often accompanied by autonomic symptoms (nausea, vomiting, increased sweating), anxiety, imbalance and nystagmus (the latter sometimes leading to blurred vision).
B. Fainting and pre-syncope. These terms refer to temporary loss of consciousness or the feeling of impending loss of consciousness. In a pre-fainting state, increased sweating, nausea, a feeling of fear and darkening of the eyes are often observed. The immediate cause of fainting is a drop in cerebral blood flow below the level necessary to supply the brain with glucose and oxygen. Fainting and presyncope usually develop against the background of arterial hypotension, heart disease or due to autonomic reactions, and the tactics for these conditions are completely different than for vestibular vertigo.
B. Impaired balance is characterized by instability, a wobbly (“drunk”) gait, but not true dizziness. The cause of this condition is damage to various parts of the nervous system that provide spatial coordination. However, patients with cerebellar, visual, extrapyramidal and proprioceptive disorders often define the feeling of unsteadiness as “dizziness.”
D. Vague sensations , often described as dizziness, occur with emotional disorders, such as hyperventilation syndrome, hypochondriacal or hysterical neurosis, depression. Patients usually complain of “brain fog,” feeling slightly intoxicated, lightheaded, or fear of falling. These sensations are quite clearly different from the sensations associated with vestibular dizziness, fainting and balance disorders. Since any dizziness, regardless of its cause, can cause anxiety, it cannot serve as evidence of the psychogenic nature of the disease.
D. Some patients with complaints of dizziness find it difficult to describe their sensations. In this case, it is advisable to conduct provocative tests.
1. The standard set of provocative tests for dizziness includes:
A. Orthostatic test. b. Forced hyperventilation for 3 minutes. V. Sharp turns while walking or spinning in a circle while standing. d. Nilen-Barany test for positional vertigo. d. Valsalva maneuver, which increases dizziness caused by craniovertebral anomalies (for example, Arnold-Chiari syndrome) or perilymphatic fistula, and also causes lightheadedness in patients with cardiovascular diseases.
2. After each test, it is necessary to ask whether the resulting dizziness resembles the sensation that worries the patient. For orthostatic hypotension, hyperventilation syndrome, positional vertigo and many vestibular disorders, test results are well reproducible, which provides important diagnostic information.
II. Clinical examination of patients with vestibular vertigo. In order to evaluate the results of research, it is necessary to have a good knowledge of the relationships of the vestibular system with the oculomotor, auditory and spinocerebellar systems. There are two main types of vestibular reflexes. Thanks to the vestibulo-ocular reflexes, gaze fixation on the objects under consideration is maintained, that is, the constancy of the image on the retina. Vestibulospinal reflexes provide the positioning of the head and torso necessary for coordinated movements and maintaining an upright posture.
A. Nystagmus in patients with dizziness is the most important sign of vestibular disorders. Knowing a few simple physiological principles can help you avoid common mistakes in interpreting nystagmus.
1. Canal-ocular reflexes. Each horizontal semicircular canal is connected through the neurons of the brain stem with the oculomotor muscles in such a way that a decrease in impulses from it causes the eyes to deviate towards this canal, and an increase causes movement in the opposite direction. Normally, the impulses constantly flowing into the brain stem from the right and left semicircular canals and otolith organs are equal in intensity. A sudden imbalance of vestibular afferentation causes a slow eye deviation that is interrupted by rapid cortical activation-induced corrective eye movements in the opposite direction (nystagmus).
2. Lesions of the labyrinth usually cause a decrease in impulses from one or more semicircular canals. In this regard, with acute unilateral lesions of the labyrinth, unidirectional nystagmus occurs, the slow phase of which is directed towards the affected ear, and the fast phase - in the opposite direction. Nystagmus can be rotatory or horizontal. It intensifies when the eyes are moved towards its fast phase (that is, towards the healthy ear). With acute vestibular dysfunction, surrounding objects usually “rotate” in the direction of the fast phase of nystagmus, and the body in the direction of the slow phase. Patients sometimes better determine the direction of rotation with their eyes closed. In a standing position, patients deviate and fall predominantly towards the slow phase of nystagmus (that is, the affected ear).
3. Central nystagmus. Alternating nystagmus, which changes its direction depending on the direction of gaze, is more often observed with drug intoxication, lesions of the brain stem, or pathological processes in the posterior cranial fossa. Vertical nystagmus almost always indicates damage to the brainstem or midline cerebellar structures.
B. Cold test. Normal physiological stimuli simultaneously affect both labyrinths. The value of the cold test is that it allows you to study the function of each labyrinth separately. The study is carried out with the patient lying down; the head is raised at an angle of 30°. The external auditory canal is washed with cold water, thereby simulating unilateral vestibular hypofunction (observed, for example, with vestibular neuronitis or labyrinthitis). Cold water causes movement of the endolymph, as a result of which the impulse from the horizontal semicircular canal decreases. Normally, this leads to nausea, dizziness and horizontal nystagmus, the slow phase of which is directed in the direction being examined, and the fast phase in the opposite direction. Monitor the direction, duration and amplitude of nystagmus. A decrease in response on one side indicates damage to the labyrinth, vestibulocochlear nerve, or vestibular nuclei on that side. The study is contraindicated if the eardrum is damaged.
B. Electronystagmography. The retina is negatively charged in relation to the cornea, so when the eyes move, the electric field changes and an electric current occurs. Recording this current (and therefore eye movements) using electrodes placed around the eyes is called electronystagmography. This method allows you to quantify the direction, speed and duration of nystagmus. Electronystagmography is used in functional vestibular tests to record spontaneous, positional, cold and rotational nystagmus. Electronystagmography can be used to record nystagmus with eyes closed. This provides important additional information since nystagmus is often suppressed during gaze fixation.
D. Hearing loss and tinnitus can occur with diseases of the peripheral vestibular system (inner ear or vestibulocochlear nerve), if the hearing aid is involved in the process. When the central nervous system is damaged, hearing is rarely impaired. For vestibular vertigo, audiological testing often helps establish the diagnosis.
1. In pure-tone audiometry, the threshold for the perception of sounds of different frequencies is measured. For differential diagnosis of sensorineural and conductive hearing loss, the auditory threshold for air and bone conduction of sound is compared.
2. For a more accurate audiological assessment, speech perception and intelligibility, the phenomenon of accelerated increase in sound volume and tone decay are additionally examined.
D. Stabilography - the study of balance using a moving platform - allows you to quantify involuntary postural reflexes that prevent falls, as well as the role of information from various senses in maintaining balance.
E. Functional vestibular tests, electronystagmography and stabilography are complex and labor-intensive procedures. They cannot replace a thorough clinical examination, and for non-vestibular vertigo they are not necessary.
III. Diagnosis and treatment of diseases accompanied by vestibular vertigo. The two most common causes of vestibular vertigo are vestibular neuronitis and benign positional vertigo.
A. Vestibular neuronitis (acute peripheral vestibulopathy, vestibular neuritis).
1. General information. Vestibular neuronitis is characterized by a sudden, prolonged attack of dizziness, often accompanied by nausea, vomiting, loss of balance, and a feeling of fear. Symptoms worsen with head movements or changes in body position. Patients tolerate this condition extremely hard and often do not get out of bed. Spontaneous nystagmus is characteristic, the slow phase of which is directed towards the affected ear. On the same side, the reaction to a cold test decreases. Positional nystagmus is often noted. Sometimes there is noise and a feeling of fullness in the ear. Hearing does not decrease, and the results of audiological examination remain normal. There are no focal symptoms indicating damage to the brain stem (paresis, diplopia, dysarthria, sensory disturbances). The disease occurs in adults of any age. Acute dizziness usually resolves spontaneously within a few hours, but may recur over the next few days or weeks. Subsequently, residual vestibular dysfunction may persist, manifested by imbalance, especially pronounced when walking. In almost half of cases, attacks of dizziness recur after several months or years. The cause of vestibular neuronitis is unknown. A viral etiology has been suggested (as with Bell's palsy), but there is no evidence of this. Vestibular neuronitis is more of a syndrome than a separate nosological form. Neurological and otoneurological examinations help establish the peripheral nature of vestibular dysfunction and exclude lesions of the central nervous system, which usually have a less favorable prognosis.
2. Therapeutic measures. A few simple techniques can significantly reduce dizziness.
1) Since head movements and external stimuli increase dizziness, the patient is recommended to lie in a darkened room for 1-2 days.
2) Gaze fixation reduces nystagmus and dizziness in peripheral vestibular disorders. Often the condition improves - and even to a greater extent than when lying with eyes closed - if patients fix their gaze on some nearby object (for example, on a picture or a raised finger).
3) Since mental stress increases dizziness, it is advisable to combine gaze fixation with mental relaxation methods.
4) In case of persistent vomiting, intravenous fluid administration is indicated to prevent dehydration.
5) Measures for persistent dizziness. With vestibular neuronitis, the condition does not improve significantly in the first 1-2 days. The person feels seriously ill and is afraid of repeated attacks of dizziness. In such a situation, it is important to reassure the patient, convincing him that vestibular neuronitis and most other acute vestibular disorders are not dangerous and pass quickly. It should also be explained that within a few days the nervous system will adapt to the imbalance between both vestibular organs (even if one of them is irreversibly damaged) and the dizziness will stop.
6) Vestibular gymnastics, which stimulates central compensatory processes, begins a few days after the acute manifestations subside.
B. Benign positional vertigo
1. General information. Benign positional vertigo is probably the most common vestibular disorder. Dizziness in this case appears only when moving or changing the position of the head, especially when tilting it back and forth. This condition often occurs when the patient turns over from his back to his side and suddenly, at a certain position of the head, feels that “the room has moved.” Dizziness usually lasts a few seconds. Often patients know in what position of the head it occurs. Changes in head position can worsen vertigo in vestibular neuronitis and many other peripheral or central vestibular disorders, but in benign positional vertigo, symptoms occur only with certain movements and are absent at other times.
2. Differences from positional vertigo of central origin. Positional vertigo can also occur with many other diseases, including lesions of the brain stem (multiple sclerosis, stroke or tumor). In order to distinguish benign positional vertigo from more dangerous diseases of the central nervous system, the Nilen-Barany test is performed. The seated patient is tilted with his head at an angle of 45°, after which he is lowered onto his back. Then the test is repeated, after first turning the thrown back head first to the right, then to the left. The result is assessed by the appearance of nystagmus and dizziness. The latent period, duration, direction and exhaustibility of nystagmus are of important diagnostic importance. In benign positional vertigo, the latent period of nystagmus and dizziness is several seconds, the nystagmus is rotatory, and its fast phase is usually directed towards the affected ear. Nystagmus and dizziness are usually short-lived (less than 30 s) and decrease with repetition of the test (depletion of nystagmus). The Nilen-Barany test can confirm the diagnosis of benign positional vertigo. However, a negative result does not exclude this disease, since its symptoms are transient and are not always triggered by head movement.
3. Etiology. Benign positional vertigo can occur after traumatic brain injury, a viral disease, otitis media or stapedectomy, as well as with certain intoxications (for example, alcohol and barbiturates). Idiopathic cases of the disease, apparently, in most cases are associated with cupulolithiasis, a degenerative process with the formation of otoconial deposits in the cupula of the frontal semicircular canal, resulting in a sharp increase in the sensitivity of this canal to gravitational influences when the position of the head changes.
4. The course of the disease can be very different. In many cases, symptoms resolve on their own within a few weeks and then do not return until months or years later. Sometimes a short-term attack occurs only once in a lifetime. Only rarely does positional vertigo persist for a long time.
5. Treatment. For symptomatic therapy, the above remedies are used, but they are often ineffective. With careful repetition of movements that provoke dizziness, pathological reactions are gradually “exhausted.” Some believe that vestibular exercises, which include provocative head movements, speed up recovery. Patients are advised to hold their head in a position that usually causes dizziness for 30 seconds. This simple exercise, performed 5 times every few hours, in most cases brings improvement within a few weeks. If such vestibular gymnastics is accompanied by too unpleasant sensations, then a soft corset is used that immobilizes the neck and prevents the head from tilting in an unfavorable direction. As with vestibular neuronitis, it is important to convince the patient that, despite the extremely unpleasant sensations, the disease will soon pass and is not life-threatening. It is extremely rare for severe persistent positional vertigo to transect the ampullary nerve coming from the frontal semicircular canal on the affected side.
B. Post-traumatic dizziness. Despite the fact that the labyrinth is protected by a bone sheath, its thin membranes are easily damaged by injury. Uncomplicated concussion is accompanied by dizziness in more than 20% of cases. With traumatic brain injury, transient autonomic disorders (palpitations, hot flashes, increased sweating), which are accompanied by non-vestibular dizziness, are also possible. Post-traumatic dizziness manifests itself in two main syndromes.
1. Acute post-traumatic dizziness. Vestibular dizziness, nausea and vomiting can occur immediately after injury due to the sudden shutdown of one of the labyrinths (labyrinth shock). Less commonly, dizziness is caused by transverse or longitudinal fractures of the temporal bone, which are accompanied, respectively, by hemorrhage in the middle ear or damage to the eardrum with bleeding from the external auditory canal.
Clinical picture. Dizziness is constant. Characterized by spontaneous nystagmus with a slow phase directed towards the lesion, and imbalance with a tendency to fall in the same direction. Symptoms intensify with sudden movements of the head and in a position where the damaged labyrinth is at the bottom.
2. Post-traumatic positional vertigo. Within a few days or weeks after the injury, repeated short-term attacks of vestibular dizziness and nausea may occur, which are provoked by head movement.
A. The clinical picture is the same as for benign positional vertigo.
b. Forecast. In most cases, spontaneous remission occurs within 2 months after injury, and within 2 years in almost all.
3. Perilymphatic fistula. The membranous labyrinth filled with endolymph is surrounded by the perilymphatic space. When a rupture occurs in the area of the oval or round opening, a perilymphatic fistula can form, through which changes in pressure in the middle ear cavity are directly transmitted to the inner ear. The cause of a perilymphatic fistula can be, in particular, barotrauma (from straining, sneezing, coughing, diving).
A. Clinical picture. Characterized by intermittent or positional vestibular vertigo and variable sensorineural hearing loss. Worsening often occurs with elevation (including rapid ascent in an elevator) and with physical exertion similar to the Valsalva maneuver (straining or lifting). Sometimes dizziness occurs with loud sounds (Tullio's symptom).
b. Diagnostics. A perilymphatic fistula should be suspected when vestibular or auditory disturbances appear after trauma. However, due to the variability of symptoms, it can be difficult to distinguish from other diseases (Meniere's syndrome, benign positional vertigo, craniovertebral anomalies). There are no pathognomonic signs in the study of pressor nystagmus, electronystagmography, or stabilography. Perilymphatic fistula is probably one of the common causes of vestibular vertigo of “unexplained etiology.”
V. Treatment. The perilymphatic fistula usually closes spontaneously, which is accompanied by the disappearance of symptoms. In persistent cases, if a perilymphatic fistula is suspected, surgical intervention is indicated (tympanotomy with restoration of the integrity of the oval or round foramen). After surgery, vestibular symptoms usually improve, but hearing is rarely restored.
G. Meniere's syndrome
1. General information. Meniere's syndrome usually begins between 20 and 40 years of age. It is characterized by sudden attacks of severe vestibular vertigo, lasting from a few minutes to several hours. Before an attack, and sometimes after it, there is a feeling of stuffiness and fullness, or noise in the ear, transient hearing loss. After an attack, imbalance may persist for a long time, especially noticeable when walking.
2. The course is characterized by remissions and exacerbations. At the onset of the disease, sensorineural hearing loss (mainly for low sounds) is episodic. As a result of repeated attacks, hearing progressively decreases, but periods of improvement are possible.
3. Pathogenesis. The main morphological changes in Meniere's syndrome are stretching of the walls and an increase in the volume of the endolymphatic space (endolymphatic hydrops). The cause may be impaired absorption of fluid in the endolymphatic sac or obstruction of the endolymphatic duct.
4. Treatment. During an attack, bed rest and vestibulolytic drugs are prescribed. The rational choice of drugs for the prevention of attacks and the assessment of their effectiveness are difficult due to insufficient knowledge about the pathogenesis of the disease and the unpredictability of its course (including the possibility of long-term spontaneous remissions). According to recent studies, any of the existing treatment regimens (including placebo) causes temporary improvement in approximately 70% of patients.
A low-sodium diet in combination with diuretics (thiazides or acetazolamide) has been recommended for the treatment of Meniere's syndrome; it has been suggested that this may reduce fluid accumulation in the endolymphatic space. However, the pathophysiological feasibility of this therapy has not been proven, and in recent years it has been used less frequently.
5. In a small proportion of cases, for frequent, severe, treatment-resistant attacks, surgical treatment is indicated. There is no ideal surgery for Meniere's syndrome. Shunting of the endolymphatic sac reduces dizziness in 70% of patients, but in 45%, hearing continues to decline after surgery. Destructive operations (selective transtemporal transection of the vestibular part of the vestibulocochlear nerve, labyrinthectomy or translabyrinthine vestibulectomy) are indicated for persistent severe dizziness and severe unilateral hearing loss.
6. Differential diagnosis
A. In all cases, it is necessary to exclude a tumor of the cerebellopontine angle (including schwannoma of the vestibular-cochlear nerve. Tumors of this location cause noise in the ear, hearing loss, imbalance, but only rarely - attacks of dizziness.
b. The cause of attacks of dizziness and hearing loss can also be infectious labyrinthitis, perilymphatic fistula, Cogan's syndrome, and hyperviscosity syndrome.
V. Congenital syphilis. Symptoms of labyrinthine lesions in congenital syphilis often appear only in middle age and can mimic Meniere's syndrome. Treponema pallidum persisting in the temporal bone causes chronic inflammation leading to endolymphatic hydrops and labyrinthine degeneration. The course is progressive. As a result, both ears are affected. All patients with bilateral Meniere-like symptoms should be examined for latent syphilis using treponemal reactions (primarily RIF-ABS), since non-treponemal reactions (including the reagin rapid test and the VDRL reaction) in syphilitic labyrinthitis can give negative results.
D. Labyrinthitis
1. Bacterial labyrinthitis. When there is a bacterial infection of the middle ear or mastoid process (such as chronic otitis media), bacterial toxins can cause inflammation of the structures of the inner ear (serous labyrinthitis). Symptoms may be minimal at first, but they gradually worsen without treatment. Direct infection of the labyrinth (purulent labyrinthitis) is possible with bacterial meningitis or disruption of the integrity of the membranes separating the inner ear from the middle ear. Patients experience acute vestibular dizziness, nausea, hearing loss, fever, headache and ear pain. Purulent labyrinthitis is a dangerous disease that requires early diagnosis and antibiotic therapy.
2. Viral labyrinthitis. Damage to the auditory and vestibular organs is observed with various viral infections, including influenza, herpes, rubella, mumps, viral hepatitis, measles, and infection caused by the Epstein-Barr virus. Most patients recover on their own.
E. Functional vertigo occurs as a result of a disruption in the interaction between the vestibular, visual and somatosensory systems, which normally work together to provide spatial orientation. Dizziness can also be caused by physiological stimulation of normally functioning sensory systems.
1. Motion sickness is caused by unusual acceleration of the body or a discrepancy between afferentation entering the brain from the vestibular and visual systems. In a person in a closed cabin on a ship or in the back seat of a moving car, vestibular afferentation creates a sensation of acceleration, while visual afferentation indicates the relative immobility of surrounding objects. The intensity of nausea and dizziness is directly proportional to the degree of sensory mismatch. Motion sickness is reduced when there is sufficient panoramic visibility to verify the reality of the movement.
2. Visually caused dizziness occurs when observing moving objects - due to a mismatch of visual afferentation with vestibular or somatosensory (for example, when a person watches a movie with a car chase).
3. High-altitude vertigo is a common phenomenon that occurs when the distance between a person and the stationary objects he observes exceeds a certain critical value. The often observed fear of heights prevents adaptation to the physiological mismatch of vestibular and visual afferentation.
G. Transient ischemia of the brainstem
1. General information
A. Clinical picture
1) Vestibular dizziness and imbalance are the two most common symptoms of transient brainstem ischemia resulting from damage to the arteries of the vertebrobasilar region. At the same time, only in rare cases are they the only manifestations of this disease. If repeated attacks of dizziness are not accompanied by other signs of brainstem ischemia (diplopia, dysarthria, sensory disturbances of the face or limbs, ataxia, hemiparesis, Horner's syndrome or hemianopsia), then they are usually caused not by vertebrobasilar insufficiency, but by peripheral vestibulopathy.
2) Impaired balance and blurred vision occur both with vestibular neuronitis and with lesions of the trunk, and therefore do not allow us to clarify the localization of the lesion. Acute hearing loss is not typical for ischemic lesions of the brainstem; a rare exception is occlusion of the anterior inferior cerebellar artery, from which the internal auditory artery arises to the inner ear.
b. Differential diagnosis
1) Since transient brainstem ischemia requires active therapy aimed at preventing brainstem stroke, it is important to differentiate it from more benign disorders (in particular, vestibular neuronitis).
2) In the interictal period with transient ischemia of the brainstem, there are no signs of focal brain damage. However, during an attack, careful examination can reveal disorders such as Horner's syndrome, slight strabismus, internuclear ophthalmoplegia, central alternating or vertical nystagmus, etc., characteristic of damage to the trunk, but not the vestibular apparatus. With ischemia of the trunk, it is often possible to induce positional nystagmus. The Nilen-Barany test helps to distinguish central from peripheral lesions. Vestibular vertigo and imbalance may also occur with brainstem lesions of other etiologies, such as multiple sclerosis or tumors.
H. Cerebellar stroke
1. Clinical picture. Damage to the cerebellum due to ischemia or hemorrhage in the posterior inferior cerebellar artery can manifest as severe vestibular vertigo and imbalance, which can easily be mistaken for symptoms of acute vestibular neuronitis. Sometimes the lesion is limited to the cerebellar hemisphere, and in this case there are no signs of damage to the lateral medulla oblongata (dysarthria, numbness and paresis of the facial muscles, Horner's syndrome, etc.). Infarction in the superior cerebellar artery causes abasia and ataxia, which are usually not accompanied by severe dizziness.
2. Diagnostics. Impaired balance with a tendency to fall towards the lesion is observed with damage to both the vestibular system and the cerebellar hemispheres and does not help in the differential diagnosis. Central alternating nystagmus, the fast phase of which is directed towards gaze, and hemiataxia indicate damage to the cerebellar hemisphere. A CT scan can diagnose cerebellar hemorrhage, but may not detect a heart attack (especially if the test is performed immediately after the onset of symptoms). A more reliable method for diagnosing cerebellar infarction is MRI.
3. Current. Cerebellar infarctions and hemorrhages are often limited in size and the outcome is favorable. Typically, gradual recovery occurs and the residual defect is minimal. More extensive lesions, accompanied by cerebellar edema, can cause compression of the trunk and fourth ventricle. This severe complication requires surgical decompression, but it can be prevented by timely dehydration, so early diagnosis and careful monitoring in the acute phase are extremely important for cerebellar strokes.
I. Oscillopsia is the illusion of vibration of stationary objects. Oscillopsia in combination with vertical nystagmus, instability and vestibular vertigo is observed with craniovertebral anomalies (for example, Arnold-Chiari syndrome) and degenerative lesions of the cerebellum (including olivopontocerebellar atrophy and multiple sclerosis).
K. Vestibular epilepsy. Dizziness can be the leading manifestation of simple and complex partial seizures if they occur in the vestibular areas of the cortex (superior temporal gyrus and association areas of the parietal lobe). Dizziness in this case is often accompanied by noise in the ear, nystagmus, and paresthesia in the contralateral limbs. The attacks are usually short-lived and can easily be confused with other diseases that manifest as vestibular vertigo. In most cases, such seizures are combined with typical manifestations of temporal lobe epilepsy. The diagnosis is confirmed by EEG changes. Treatment: anticonvulsants or resection of the affected area of the brain.
L. Migraine
1. Clinical picture. Dizziness can be a leading symptom of basilar migraine. During an attack, visual and sensory disturbances, disturbances of consciousness, and intense headache are also noted.
2. Diagnostics. Recurrent attacks of vestibular vertigo (in the absence of other symptoms) may be a manifestation of dissociated migraine. The diagnosis of migraine in this case is possible only if all other causes are excluded; it is more likely if there are other manifestations of this disease.
M. Chronic vestibular dysfunction
1. General information. The brain is able to correct the disrupted connection between vestibular, visual and proprioceptive signals. Thanks to central adaptation processes, acute dizziness, regardless of its cause, usually resolves within a few days. However, sometimes vestibular disorders are not compensated due to damage to the brain structures responsible for the vestibulo-ocular or vestibulospinal reflexes. In other cases, adaptation does not occur due to concomitant visual or proprioceptive impairments.
2. Treatment. Constant dizziness, impaired balance and coordination of movements can cause disability for the patient. Drug therapy in such cases is usually ineffective. Patients with persistent vestibular dysfunction are shown a set of special exercises (vestibular gymnastics).
A. Exercise goals
1) Reduce dizziness. 2) Improve your balance. 3) Restore self-confidence.
b. Standard complex of vestibular gymnastics
1) Exercises to develop vestibular adaptation are based on the repetition of certain movements or postures that cause dizziness or imbalance. It is believed that this should promote adaptation of the vestibular structures of the brain and inhibition of vestibular reactions.
2) Balance exercises are designed to improve coordination and use information from multiple senses to improve balance.
Diagnostics
To make a correct diagnosis of severe dizziness when turning the head in a lying position, a comprehensive examination of the patient is required. The doctor will definitely find out the features that accompany the symptom:
- additional symptoms does the patient experience
- How often do you feel dizzy and how long does the attack last?
- What exactly feel when they feel dizzy when turning their head while lying down?
- In what position does this condition most often occur - if the patient lies on his back, right or left side.
- intensify when you turn your head and change your body position?
- What do if he experiences severe dizziness when turning his head while lying down?
Dizziness when tilting your head
The head and neck perform functions such as supporting the functioning of the brain, sensory organs and blood vessels.
In this case, the doctor’s task is to identify the factors that provoke the condition. The therapist pays attention to the color of the patient’s skin, mental state, stability of gait and other details.
Taking an anamnesis necessarily includes measuring the patient’s blood pressure in a lying and standing position, and, according to the doctor’s indications, during physical exercise.
If blood pressure decreases in an upright position, then severe dizziness when turning the head in a lying position may represent an attack of lipothymia, when the patient faints if he suddenly rises to his feet. To exclude anemia, diabetes, lack of elements and dehydration of the body, a general and biochemical blood test and urine test are taken.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
If necessary, the doctor prescribes an examination with several specialists at once: a cardiologist, an otolaryngologist, an infectious disease specialist, an ophthalmatologist and a neurologist.
Causes of tinnitus and dizziness
Tinnitus and dizziness can last from a second to several hours.
To identify the causes of dizziness when turning the head in a lying position, various studies are carried out:
- Magnetic resonance imaging;
- CT scan;
- X-ray of the cervical region, spine, temporal bones;
- Ultrasound of neck vessels;
- Dopplerometry - study of blood flow;
- audiometric test - to identify hearing impairment due to damage to the inner ear;
- provocative test - checking the vestibular apparatus and nervous system disorders;
- Romberg test , the study of involuntary eye twitching (nystagmus) in a patient during the Dix-Hallpike test.
To do this, the doctor asks the patient to sit on the couch so that his legs are extended in front of him. Then he carefully turns the patient's head 45 degrees to the side. In this case, the patient’s gaze should be directed to the doctor.
From this position, the patient is placed on his back so that only the torso lies on the couch, and the head is on the edge without support. The patient lies for 30 seconds with his head thrown back, then sits up. Next, carry out the same actions, but with the head turned in the other direction.
After the examination, the doctor makes a conclusion whether nystagmus is the cause of dizziness when turning the head in a lying position.
Possible diseases
In the absence of pathologies, they speak of benign paroxysmal or positional vertigo. It lasts up to 1 minute. In most patients, its episodes are not isolated and appear again with a sharp transition from a lying position to any other.
Pathological causes of dizziness include:
- Meniere's disease;
- vestibular neuronitis;
- Lermoyer's syndrome;
- central positional nystagmus;
- labyrinthitis;
- transient ischemic attack;
- stroke;
- vertebrobasilar insufficiency;
- vestibular migraine;
- perilymphatic fistula.
Only a specialist can make a correct diagnosis after a comprehensive examination. In some cases, no pathologies or abnormalities are detected, but the person experiences dizziness. Then they talk about the psychogenic nature of the condition and recommend reducing the level of stress in life.
Treatment
Treatment is prescribed after the reasons why the patient is dizzy are established.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
A possible list of medications prescribed by a doctor for severe dizziness when the patient turns his head while lying down.
| Drug class affiliation | What effect does it have on the body? |
| Neuroleptics | They have a calming effect in neurotic disorders, psychomotor agitation and depression. |
| Antihistamines | Have an anti-allergenic effect, a relaxing (sedative) effect |
| Drugs for the treatment of the cardiovascular system | Maintains cerebral vascular tone, improves blood supply and cell nutrition |
| Nootropic drugs | Stimulates brain activity, improves memory, helps nourish nerve cells |
Under no circumstances should you self-medicate or take painkillers during attacks. This method will help for a short period of time and will only worsen the disease:
- If the cause of severe dizziness when turning the head in a lying position lies in damage to the vestibular apparatus, the doctor may prescribe special rehabilitation training. It includes exercises to support balance. This method works well after traumatic brain injury, but can only be used for those patients who experience dizziness attacks regularly.
- If dizziness when turning the head while lying down is a symptom of neurotic disorders and depression of the patient, antidepressants and tranquilizers are prescribed, and a neurologist or psychiatrist provides psychological support and assistance.
- If the head is dizzy due to a lack of iron due to anemia, the patient is prescribed a special diet and iron supplements, it is recommended to walk in the fresh air more often, and increase the duration of sleep.
In some cases, surgery is necessary to eliminate the causes of dizziness when turning the head while lying down. This decision is made by the doctor if the patient has a tumor, progressive Meniere’s disease and other serious cases.
Drug treatment
There are no drugs that have a direct effect on canal/cupolothiasis.
Drug treatment is advisable only for frequent attacks or during maneuvers.
Drugs are used that reduce the excitability of the vestibular system, both selectively and through a general sedative effect. The first include drugs with a vestibulolytic effect - blockers of H1 and H3 histamine receptors, cinnarizine, atarax, first generation antihistamines - diphenhydramine, pipolfen.
Evidence has been obtained in favor of reducing the intensity of dizziness when performing the Epley maneuver simultaneously with taking betahistine 24 mg x 2 times a day for a week.
Sedatives, most commonly benzodiazepine tranquilizers (diazepam), are used in hospital settings for the symptomatic treatment of severe recurrent attacks.
Ellie's exercises
A complex of special gymnastics is used as one of the main methods of treating canalithiasis. Exercises that eliminate dizziness when turning the head while lying down are performed in the presence of a doctor according to a certain scheme. The patient needs:
- Sit on the examination table and close your eyes.
- Turn your head sharply to the right 45 degrees.
- Quickly lie on your back, hanging your head from the end of the table at 20 degrees (the angle is controlled by medical staff).
- Turn your head to the left 90 degrees.
- Remain at rest for 30 seconds.
- Perform another turn of the head to the left at a right angle, while simultaneously turning the body in the same way.
- After 30 seconds, sit or stand on the left side of the table.
If, at the end of the gymnastics, the patient still feels dizzy when turning his head while lying down, the doctor considers the option of repeating the exercises. For complete restoration and normalization of the vestibular apparatus, no more than three procedures are required.
Positional maneuvers
Another method of treating dizziness when turning the head while lying down by returning the fallen crystals to their place has something in common with Ellie’s exercises. The number of repetitions and methods of fixing the head and torso change. The most widely used maneuvers are Brandt-Daroff, Semont, Epley, and Lempert.
Brandt-Daroff maneuver
Can be done at home. The best time is immediately after waking up. Actions are performed according to the following scheme:
- Having woken up, the person sits on the bed, dangling his legs.
- Immediately you need to lie on your side with your legs slightly bent.
- Having turned your head 45 degrees, you need to hold it in this position for 30 seconds, then sit down again.
- The exercises are repeated first on the other side.
Do 5 approaches on each side. If during therapeutic exercises you feel noticeably dizzy when you lie down and change position before sitting down, you need to wait until the symptoms subside. You can repeat the exercise before going to bed.
Semont maneuver
The procedure can only be performed under the supervision of a physician due to the risk of heart rhythm disturbances and aggravation of the manifestations of canalithiasis.
First, in a sitting position with legs dangling, the patient turns his head to the healthy side by 45 degrees. Holding the head, the doctor helps the patient lie down on the painful side, leaving him in this position for 2 minutes.
Without letting go of the head, the doctor sits the patient down again, after which he immediately places him on the other side. The patient's face is turned down. After 2 minutes you can return to the starting position.
The method is considered aggressive and is used with extreme caution to treat severe dizziness when changing body position while lying or sitting.
Epley maneuver
Like the previous technique, it is performed under the supervision of a doctor. The patient needs to sit on the couch, turning his head to the painful side 45 degrees. The doctor fixes it in this position and helps the patient lie on his back, keeping his head thrown back.
After a minute, the head is turned towards the healthy ear, then the body is placed on the same side. After another minute, the patient is helped to take the starting position, sitting him on the couch.
Lempert maneuver
The technique is similar to the previous maneuver. The difference is that after turning the body, the gymnastics does not stop, continuing the rotation. From a lying position on the healthy side, the patient needs to turn onto his stomach, face down, and return to the affected side again. After such rotation around its axis, the patient returns to its original position.
To consolidate the result and eliminate dizziness when turning the head while lying down after performing the maneuver, a number of restrictions are observed. In the first 24 hours, while sleeping, the head of the bed is raised 45-60 degrees. During the daytime, bending of the body is limited.
What to do
There is a clear algorithm of actions for providing first aid for dizziness:
- Ventilate the room.
- Remove the patient's tight clothing and unbutton the narrow collar.
- Place a high pillow (at an angle of 30 degrees).
- Call an ambulance .
- Measure your blood pressure if you have a tonometer.
- Do not take medications until examined by a doctor.
If an attack of severe dizziness when turning the head while lying down occurs suddenly, when the person is alone, you need to lie down in a calm state with your eyes closed, and not make sudden movements. If possible, place your head on a high pillow.
Prevention
To prevent attacks of dizziness from happening again, you need to review your daily routine, ensuring your body gets adequate sleep and rest. It is important to regularly be in the fresh air, to adhere to moderate physical activity without sudden movements of the head and torso.
If you are prone to dizziness when turning your head while lying down, you should not endure colds on your feet - in the first days of the illness, be sure to observe bed rest, further treatment is carried out until the symptoms of the disease are completely eliminated.
Dizziness when turning your head while lying down can be caused by external influences: intense exercise, severe stress, changes in atmospheric pressure. In these cases, proper rest and walks in the air help well.
In other situations, severe dizziness when turning the head in a lying position may be one of the symptoms of a serious illness. Therefore, it is important to consult a doctor promptly to diagnose the condition.