body .attr-article__date{ background: none; padding: 0; }
NEAD EAD SEAD South Administrative District South-Western Administrative District CJSC Central Administrative District SZAO Northern Administrative District 01 02 03 05 06 07 08 09 1 0 1 1 1 2 14 18 15 16 17 Babushkinskaya Prospekt Mira Pervomaiskaya Baumanskaya Paveletskaya Teply Stan Shipilovskaya Prague Academic University Barrikadnaya River Station Oktyabrskoye Bratislava Taganskaya Academician Yangelya October Field
The call center is open 24 hours a day
Ambulance 24/7
Date of publication: 04/19/2017
until October 31
We're giving away RUR 1,000 for all services per visit in October More details All promotions
Symptoms of a concussion
A concussion occurs when an external impact or force causes a sudden movement of the head. In this case, the brain is displaced inside the skull, and brain tissue “impacts” against its walls, which leads to the development of concussion symptoms.
The most common symptoms of a concussion
:
- headache;
- dizziness;
- nausea;
- confusion;
- deterioration of concentration and memory;
- memory loss;
- irritability, personality changes;
- increased sensitivity to light and sounds;
- sleep disturbance;
- decreased mood;
- disturbances of smell and taste.
A concussion is not always accompanied by loss of consciousness!
Only less than 10% of people lose consciousness with a concussion.
You don't have to hit your head!
Damage to other parts of the body, as well as sudden acceleration or deceleration of movement, can also lead to a concussion.
All cases of concussions require seeking medical help!
Recommendations for a speedy recovery
Complete rest is the key to recovery.
Avoid any mental or physical activity that may make your condition worse.
Avoid physical overexertion, which can worsen symptoms
:
- Sport
- Any vigorous activity
Limit mental stress or activities that involve high concentration as this may worsen your condition:
- video games
- watching TV
- reading
- correspondence
- using a computer
- school lessons
Do not take medications containing ibuprofen or aspirin for headaches caused by concussions.
because these drugs may increase the risk of bleeding. Acetaminophen-based medications can be used.
Do not resume sports activities
before your doctor allows you to do so.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Make an appointment
Consequences of fights and falls - concussion
We will try to answer this question in this not very long article!
There are few people in the world who have not heard anything about concussions. Most, both men and women, can talk about situations in which they have been and received various types of injuries. In some cases there were concussions, and maybe someone was on the verge of it. But no one can give a clear answer. They usually say that there was a severe headache and dizziness, but “I” did not turn anywhere.
Let's get creative! Imagine a decent-sized egg - it will be a human head, where the skull replaces the shell, the brain is the yolk inside, and the white is cerebrospinal fluid. Introduced? Now let’s shake the egg or hit it. The yolk floating inside collides with the shell, and each touch leaves marks on the yolk.
The same thing happens with the human brain (usually everyone has one!). He is very gentle and fragile. Any contact of the brain with the skull leads to a change in the shape of brain cells or a so-called concussion. The condition of a concussion is not a pleasant one. There are cockroaches rushing somewhere in my head all the time! But this is much better than if, upon impact, the integrity of the skull was not preserved.
The consequences of such injuries can be different. For example, loss of connection. This can occur selectively between any brain cells, and maybe between entire departments. There is poor interaction between the trunk and its identical opposite hemispheres.
Some symptoms of a concussion
Such symptoms include an increase in the size of the eye pupils, vomiting, even slight memory loss, partial or complete loss of taste and impaired sense of smell. But a head concussion does not always cause these symptoms, and if something bad happened to you, after which you have been dizzy for several days or have signs of a headache, contact the clinic. See a neurologist to examine your skull.
Concussion
Most concussions occur due to some kind of blow. And blows reach our heads in different ways and usually cause swelling and minor hemorrhages. These can, of course, include reckless fights, serious falls with injuries and, of course, accidents. A concussion occurs only due to a strong blow (the direction does not matter) to the head, because the brain must be displaced in such a way that a collision with the skull occurs. A weak impact does not cause a concussion.
After such a strong blow, damage occurs and sometimes even destroys some of the nerve cells that are responsible in the body for the passage of impulses to the brain. There comes disorder in their work, you can call it a neural storm in the brain. It is cellular rabies that leads to significant loss of vision and loss of memory (full or partial), vomiting and nausea, headaches, etc.
The brain heals us!
It's good that our amazing brain itself is engaged in our treatment. He voluntarily begins the process of pacifying rebellious neurons by increasing glucose production. After all, with the help of glucose, blood vessels contract, and this means the work of the brain slows down. And the restoration process will end only when everything returns to its normal appearance.
Self-medication usually takes several weeks. The only requirement: do not receive new concussions or negative impacts during this period. Otherwise, new damage may not be reversible and will lead you to dementia. The main medicine in this situation is peace and only peace!
Lie down and rest in silence, preferably without TV.
So as not to disturb the nerve cells. If you notice similar symptoms, consult a doctor, as rest alone may not be enough! You may need treatment with medications, because the head is not to be trifled with! Take care of your health! Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
How to prevent a concussion?
In children:
For parents of little fidgets
Many childhood injuries can be prevented by following simple tips. Read about how to avoid childhood injuries.
- Always supervise your child on the playground. Make sure he can maintain balance on slides, horizontal bars and other sports equipment.
- Teach your child to jump correctly even from low obstacles.
- If you are teaching your child to ride a two-wheeler, be sure to purchase a helmet
. - If your child is involved in a sports section, make sure that the coach strictly follows all safety rules.
- Be sure to buy your baby a full set of protective equipment
. - Do regular exercises with your child to develop balance and coordination.
For adults:
- Carefully follow the safety precautions
and rules of the sport you are involved in. - Soberly assess your strength when playing sports, especially when mastering new sports equipment.
- For cycling, horseback riding, skiing or skateboarding, be sure to purchase a special protective helmet.
- Avoid alcohol. Intoxication increases the risk of falls and head injuries.
- Don't forget about exercises to develop balance and coordination. They are useful for everyone.
For what symptoms should you urgently call a doctor?
- If you fall from a height onto a hard object or surface
- If a person who has been injured loses consciousness and does not come to his senses for more than 2 minutes
- If a child is injured and loses consciousness for at least a couple of seconds
- If there is a loss of consciousness of a delayed type: the person first loses consciousness, then comes to, then passes out again
- If after injury there are repeated bouts of vomiting
- If a person has a confused consciousness, a clouded perception of reality
- If after an injury a person becomes sleepy, he cannot move, experiencing severe weakness
- If you have a severe headache
- If there are memory lapses or complete loss of memory
- If a person constantly repeats the same word or gesture.
First aid for concussion
- If one or more symptoms are present, immediately call an ambulance or take the victim to a doctor.
- Treat a wound on the head if it appears as a result of an impact.
- For an hour or until the doctor arrives, it is important not to fall asleep, but to remain at rest.
- If you lose consciousness, lay the person on his side, bend his knees, and put his hands under his head.
- If symptoms of a concussion do not immediately appear, it is recommended to rest and not begin vigorous activity.
Post-traumatic vertigo
Dizziness ranks third in frequency among complaints in patients with a history of traumatic brain injury and whiplash injury of the cervical spine, after headache and neck pain. Post-traumatic dizziness may be based on psychogenic or neurogenic (usually organic) causes. Conventionally, all forms of post-traumatic dizziness are divided into central and peripheral (vestibular).
Central post-traumatic vertigo
The main clinical forms of central post-traumatic dizziness include:
- Dizziness due to concussion/contusion of the brain (mainly due to damage to the brain stem and/or cerebellum);
- Post-traumatic psychogenic (stress-induced) dizziness.
Dizziness due to concussion/bruise of the brain
Experimental and clinical studies have proven that traumatic brain injury (TBI) causes pathological changes in various parts of the brain that persist for many months after the injury, which causes long-term post-traumatic disorders and leads to partial or complete disability.
Primary (mechanical) damage in TBI can be local or diffuse. Local damage causes a contusion (contusion) of the brain - a focus of traumatic crushing of brain tissue, which usually occurs at the site of impact (the zone of direct application of external mechanical force) or counter-impact (at the opposite wall of the skull, to which the brain is displaced during the impact). The formation of a contusion focus may be accompanied by a fracture of the skull bones and rupture of superficial vessels with the development of intrathecal hemorrhage.
In any TBI, diffuse axonal damage occurs due to the rupture of axons during brain movement due to linear or rotational acceleration, which causes displacement of the cerebral hemispheres relative to the rigidly fixed trunk and a transient increase in intracranial pressure.
The result is tension and twisting of long axons in the deep white matter of the hemispheres, the corpus callosum and the trunk, causing diffuse axonal damage.
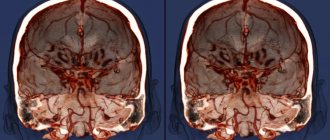
| A | B |
A - CT image of a subdural hematoma (*) in a patient after a fall from a height. B — MRI image of the patient’s brain after an accident; The arrow indicates an area of altered signal visible on magnetic resonance imaging as a result of diffuse axonal damage.
Currently, traditional therapy for TBI includes nootropic, neuroprotective, vasoactive, anticholinesterase drugs, antioxidants, anxiolytics and B vitamins. In addition, complex treatment uses betahistine 24 mg 2 times a day (at least 1 month), neuromidin 20 mg 3 once a day for 2 months (in the absence of convulsive syndrome).
Post-traumatic psychogenic (stress-induced) dizziness
The clinical picture and treatment of post-traumatic psychogenic dizziness are similar to phobic postural dizziness. Treatment is also carried out with medicinal (antidepressants, antipsychotics) and non-medicinal (psychotherapy, vestibular and breathing exercises) methods of treatment.
Post-traumatic peripheral vestibular vertigo
The following forms of post-traumatic peripheral vestibular vertigo are distinguished:
- Post-traumatic benign positional vertigo;
- Post-traumatic vestibulopathy;
- Perilymphatic fistula;
- Decompression dizziness;
Post-traumatic benign positional vertigo
The pathogenesis and treatment of the disease are the same as for idiopathic benign paroxysmal positional vertigo.
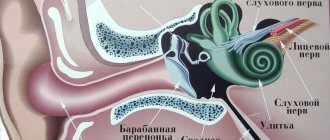
Post-traumatic vestibulopathy
In some cases of brain injury, it is possible to develop unilateral hemorrhage into the labyrinth or a fracture of the temporal bone pyramid with damage to the vestibulocochlear nerve or labyrinth. In addition, it must be remembered that with TBI, mechanical energy is transmitted to the labyrinth not only directly through bone tissue, but also indirectly through brain structures, mainly due to the hydrodynamic wave formed during a lateral impact on the skull. In such patients in the post-traumatic period, severe dizziness, nystagmus, and impaired coordination of movements are observed. The diagnosis is established on the basis of complaints, anamnesis, and characteristic objective symptoms. Particular attention is paid to the condition of the external auditory canal and the eardrum (the presence or absence of bleeding from the external auditory canal, ruptures of the eardrum).
Patients who have suffered a TBI with a temporal bone fracture usually have severe general cerebral neurological symptoms that mask auditory or vestibular disorders.
Longitudinal fracture of the temporal bone in a patient with post-traumatic vestibulopathic syndrome (computed tomography)
Decompression dizziness
Decompression sickness occurs in workers of various professions whose work involves exposure to conditions of high atmospheric pressure. These include divers, workers involved in the construction of bridge supports, subway tunnels, excavation of flooded mine shafts and other structures in water-saturated soils or under water. In addition, this pathology is often found in divers.
Decompression dizziness often occurs in novice divers who make mistakes in calculating their ascent time.
The main danger when deep-sea diving or performing work at depth is a violation of the decompression regime (the period of equalization of atmospheric pressure) during ascent. If the transition from normal to increased atmospheric pressure and back occurs faster than the time set for this, various pathological manifestations may develop, including decompression (caisson) sickness.
The disease occurs due to the transition of blood gases and body tissues from a dissolved state to a free one. The resulting gas bubbles disrupt normal blood circulation, irritate nerve endings, and deform and damage body tissues. One of the forms of moderate decompression sickness is decompression dizziness or Meniere-like syndrome. It occurs as a result of the formation of gas bubbles in the labyrinth of the inner ear. The clinical picture most often develops after the diver reaches the surface (a short latent period is possible). Suddenly there is a sharp weakness, heaviness and pain in the head. These symptoms intensify and are combined with severe systemic dizziness, vomiting, noise and ringing in the ears, and hearing loss. Victims experience severe pallor, sweating, and weakness. Dizziness bothers me even when lying down. Patients complain that all objects rotate before their eyes; A slight turn of the head significantly intensifies the painful phenomena. Upon examination, spontaneous nystagmus and a decrease in heart rate are determined; loss of consciousness is possible.
The only reliable method of treating decompression dizziness is therapeutic recompression in a special pressure chamber, which involves re-placing the victim under high pressure conditions. The earlier recompression is started, the better the prognosis for functional recovery. Before the start of therapeutic recompression, continuous oxygen inhalation is indicated. Analgesics and drugs to normalize blood pressure are prescribed upon request.
← Back
It takes time to recover
A person who has suffered a head injury needs time to recover. Do not return to exercise until your doctor allows it.
Those who begin vigorous physical activity too early have a high chance of suffering a second concussion due to poor coordination and balance. New head injury may cause permanent damage
brain
Try to stop reading (especially on mobile devices!), watching TV, and working on the computer for at least a week.
Brain injury
The disorders that occur after a traumatic brain injury are very varied and often very dangerous.
Doctors distinguish between acute disorders (developing immediately after brain damage) and long-term disorders (appearing long after the injury).
Call us and we can help you!
According to statistics, after a TBI, acute symptoms develop within three days; this is the critical period after which, most likely, the most severe consequences of brain injuries should no longer be expected.
The consequences of a traumatic brain injury can be completely unpredictable and very dangerous. The fact is that after a head blow, a so-called “lucid interval” may occur, during which the symptoms of a traumatic brain injury are completely invisible, even when examined by an experienced doctor.
Danger of TBI
This is the great danger, because symptoms of cerebral edema or subarachnoid hematoma can develop only after 24 hours or more. In this case, the patient is in great danger.
I have heard more than once from emergency department doctors how subarachnoid or subdural hematomas went unnoticed, which leads to a high risk of patient mortality.
Therefore, after a traumatic brain injury, even if you feel well, you must urgently, within a few hours, seek help from a specialist, a neurologist, and carry out the necessary diagnostic procedures.
As a result of traumatic brain injuries, a concussion (commotion) can occur - a relatively mild injury or a bruise (contusion) of the brain - a more serious condition.
- Most often they manifest themselves as gross disturbances of consciousness in the form of:
- coma (unconscious state) or
- stupor (a condition resembling stupor),
the duration and severity of which depends on the degree of mechanical impact on brain tissue.
Long-term consequences
Long-term consequences of TBI can manifest as neurological disorders:
- sensitivity disorders (numbness of the hands, feet, burning sensations, tingling sensations in various parts of the body, etc.),
- movement disorders (tremors, coordination disorders, convulsions, slurred speech, stiffness of movements, etc.),
- changes in vision (double vision, blurry focusing)
- mental disorders.
Mental disorders and behavioral disorders due to brain injuries can be expressed in different conditions: from fatigue to a pronounced decrease in memory and intelligence, from sleep disturbances to incontinence of emotions (attacks of crying, aggression, inadequate euphoria), from headaches to psychoses with delusions and hallucinations.
The most common disorder in the picture of the consequences of brain injuries is asthenic syndrome.
The main symptoms of asthenia after traumatic brain injury are complaints of fatigue and rapid exhaustion, the inability to bear additional stress, and unstable mood.
Characterized by headaches that worsen with exercise.
An important symptom of an asthenic condition that occurs after a traumatic brain injury is increased sensitivity to external stimuli (bright light, loud sound, strong smell). It is very important to know that much depends on whether the concussion or brain injury occurred for the first time, or whether the patient has repeatedly suffered such injuries at home. The outcome and duration of treatment directly depends on this.
If a patient has a history of more than 3 concussions, the period of treatment and rehabilitation is significantly longer and the likelihood of complications also increases.
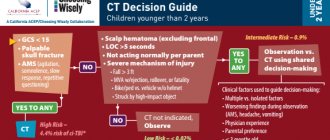
Diagnosis of traumatic brain injury
In case of traumatic brain injury, diagnostic procedures must be performed urgently.
It is also important to be examined and observed by specialists monthly after injury. As a rule, methods of magnetic resonance imaging, computed tomography, and radiography are used in the diagnosis of TBI.
What to do?
What to do if you have a concussion? Treatment of a concussion is most often carried out in a neurosurgical department for a period of 7 to 10 days (although it is not always required, and often patients refuse further therapy after 2-3 days of treatment), followed by rehabilitation in a clinic at the place of residence if necessary (the presence of a bruise soft tissues, limb fractures, etc.). Sick leave is given for two weeks and only if absolutely necessary is extended for a longer period. The most important point of treatment is the appointment of bed or semi-bed rest for a period of one week to ten days.
Drug therapy is represented by restorative and symptomatic drugs. For significant headaches, painkillers are prescribed (Dylaxa, Ketonal, etc.). It is always possible (but not necessary) to prescribe neuroprotective treatment; Phenotropil, Glycine, Ceraxon, etc. are used. All manifestations of the injury completely disappear within the first month.
Specific treatment for dizziness due to a concussion is not required. Maximum - it makes sense to prescribe general-acting drugs, for example, Mexidol, Glycine and similar neuroprotective drugs for a short course.
According to medical statistics, based on the results of many studies, there are no consequences after a concussion, because there are no changes in the brain tissue itself. But still, even weak, but repeated injuries in combination with disturbances of blood circulation in the vessels of the head and neck, dysmetabolic processes (diabetes mellitus) can lead to encephalopathies of combined genesis, the treatment of which is the prerogative of a neurologist. Dizziness as a symptom is in first or second place in frequency.
Classification
Concussion is classified into three degrees:
1.
Mild degree.
The victim is conscious, and within half an hour after the injury there are typical complaints of headache, dizziness, nausea, and disorientation in space. After half an hour the condition returns to normal. 2.
Average.
Consciousness is preserved, short-term memory loss occurs, the symptoms are similar to mild, dizziness persists, there may be a headache, nausea, the victim is disoriented in space. 3.
Severe degree. For her, loss of consciousness lasting a couple of minutes, maybe several hours, is accompanied by retrograde amnesia. Symptoms of headache, dizziness, nausea, disorientation in space can remain for two or three weeks, problems with sleep, and loss of appetite occur. Organic brain lesions lead to the appearance of vascular dementia. This is a secondary disease, that is, occurring against the background of some pathological process. The main reason is a previous ischemic or hemorrhagic stroke.
Long-term consequences of traumatic brain injuries
Long-term consequences of traumatic brain injuries occur when full recovery does not occur after the injury. This depends on many factors: the severity of the injury, the age of the patient at that moment, his state of health, character traits, the effectiveness of the treatment and the influence of additional factors, for example, alcoholism. Traumatic encephalopathy
Traumatic encephalopathy is the most common form of mental disorder during the long-term consequences of brain injury. There are several options.
Traumatic asthenia (cerebral asthenia) is expressed mainly in irritability and exhaustion. Patients become unrestrained, hot-tempered, impatient, unyielding, and grumpy. They easily enter into conflict and then repent of their actions. Along with this, patients are characterized by rapid fatigue, indecisiveness, and lack of faith in their own strengths and capabilities. Patients complain of absent-mindedness, forgetfulness, inability to concentrate, sleep disturbances, as well as headaches, dizziness, aggravated by the weather and changes in atmospheric pressure.
Traumatic apathy manifests itself in a combination of increased exhaustion with lethargy, lethargy, and decreased activity. Interests are limited to a narrow circle of concerns about one’s own health and the necessary conditions of existence. Memory is usually impaired. Manic episodes are more common than depressive episodes and occur predominantly in women.
Depression is accompanied by tearfulness or a dark, angry mood. Depression with anxiety and fear is often combined with clouded consciousness (mild stupor, delirious phenomena). If depression is often preceded by mental trauma, then a manic state is provoked by drinking alcohol.
An elevated mood sometimes takes the form of euphoria and complacency, sometimes excitement with anger, sometimes foolishness with feigned dementia and childish behavior. In severe cases of psychosis, clouding of consciousness such as twilight or amentive occurs, which is less prognostically favorable. Attacks of psychosis are usually similar to one another in their clinical picture, like other paroxysmal disorders, and are prone to repetition.
Hallucinatory-delusional psychosis
Hallucinatory-delusional psychosis is more common in men after 40 years of age, many years after the injury. Its onset is usually provoked by surgery or taking large doses of alcohol. It develops acutely, begins with clouding of consciousness, and then deceptions of hearing (“voices”) and delusional ideas become the leading ones. Acute psychosis usually becomes chronic.
Paranoid psychosis
Paranoid psychosis, unlike the previous one, develops gradually over many years and is expressed in a delusional interpretation of the circumstances of the injury and subsequent events. Ideas of poisoning and persecution may develop. A number of people, especially those who abuse alcohol, develop delusions of jealousy. The course is chronic (continuous or with frequent exacerbations).
Traumatic dementia
Traumatic dementia occurs in approximately 5% of people who have suffered a traumatic brain injury. More often observed as a consequence of severe open craniocerebral injuries with damage to the frontal and temporal lobes. Trauma in childhood and later life causes more pronounced intellectual defects.
Repeated injuries, frequent psychoses, additional vascular lesions of the brain, and alcohol abuse contribute to the spread of dementia. The main signs of dementia are memory impairment, decreased interests and activity, disinhibition of drives, lack of a critical assessment of one’s own condition, importunity and misunderstanding of the situation, and overestimation of one’s own capabilities.
Prognosis for traumatic brain injury
Concussion is a predominantly reversible clinical form of traumatic brain injury.
Therefore, in more than 90% of cases of concussion, the outcome of the disease is the recovery of the victim with full restoration of ability to work. Some patients, after the acute period of concussion, experience certain manifestations of post-concussion syndrome: disturbances in cognitive functions, mood, physical well-being and behavior. 5-12 months after a traumatic brain injury, these symptoms disappear or are significantly smoothed out. Prognostic assessment in severe traumatic brain injury is carried out using the Glasgow Outcome Scale. A decrease in the total number of points on the Glasgow scale increases the likelihood of an unfavorable outcome of the disease. Analyzing the prognostic significance of the age factor, we can conclude that it has a significant impact on both disability and mortality. The combination of hypoxia and arterial hypertension is an unfavorable prognosis factor.
Possible symptoms of a concussion
- Brief confusion or loss of consciousness. With a strong blow, the moment of injury disappears from memory.
- Dizziness even at rest, and when turning, bending or other changes in body position, the symptom intensifies.
- Severe headache, nausea and vomiting.
- Double vision, inability to concentrate on one point.
- Increased sensitivity to light and sounds.
- Impaired coordination of movements.
- Reaction inhibition - the victim gives an answer to the question after some time.
- Pale skin, weakness, sweating.
Important! A concussion is not always accompanied by visible head injuries, so the absence of wounds does not exclude brain injury.