The phenomenon of coma has been known since ancient times and is still not fully understood. The term is translated from Greek as “deep sleep.” In reality, a coma has very little in common with sleep; it is a dangerous near-death state.
The modern medical community views coma as a defensive reaction, which manifests itself in the loss of consciousness in response to critical disruptions in the functioning of the body. When a person remains unconscious for a long time, irreversible changes begin to occur in the body: reflex activity decreases, breathing becomes difficult, blood circulation is disrupted, and failures occur in almost all vital systems.
What causes coma: the main reasons
It is believed that a person can fall into a coma due to impaired blood circulation in the cerebral cortex. Another most common cause is toxic damage to cells of the central nervous system. Various diseases or injuries can provoke the occurrence of pathologies:
- strokes;
- traumatic brain injuries;
- decompensated diabetes mellitus;
- inflammatory diseases: meningitis, encephalitis;
- poisoning resulting in pathologies in the kidneys or liver;
- a series of consecutive epileptic seizures;
- hypoxia as a result of suffocation, drowning, cardiac arrest.
In medicine, there is such a thing as a medically induced coma. In this case, the patient is deliberately rendered unconscious using special drugs. This method is used for complex neurosurgical procedures, as well as to stop epileptic seizures in especially severe cases.
Funeral arrangements
Treatment
Treatment is a complex, comprehensive process that must prevent death, maintain vital body functions, and at the same time combat the root cause of this condition.
The first resuscitation measures aimed at preserving a person’s life are carried out immediately upon the arrival of the ambulance team and during transportation of the patient, before all diagnostic procedures are carried out. First aid consists of fixing the patient's position, ensuring patency of the airway - straightening the tongue, clearing the nose and mouth of vomit, an oxygen mask, tracheotomy with the installation of a breathing tube. It is necessary to normalize blood circulation by administering medications that normalize cardiac activity and blood pressure. If necessary, indirect cardiac massage is performed.
In the intensive care unit, the patient is connected to an artificial respiration apparatus. Medicines are administered aimed at eliminating the pathological symptoms of the disease - anticonvulsants, antipyretics, hemostatics. Intravenous infusions of glucose and saline solutions are required. Measures are necessary to normalize body temperature. In case of hypothermia, the patient is covered and covered with hot water bottles. If there is a suspicion of poisoning with chemical or pharmacological drugs, gastric lavage is performed.
At the second stage, having detailed results of all types of examinations, the cause is eliminated. In case of hyperglycemic coma, measures are taken to normalize blood sugar and insulin levels. In case of renal failure, hemodialysis is performed. If an injury, hematoma or brain tumor is detected, urgent or planned surgical intervention is performed according to indications.
Depth of coma
There is a widespread belief that a person always falls into a coma suddenly. However, this is not the case. In some cases, it can even develop over several days.
Comatose states are divided according to the degree of their depth. It is customary to distinguish several stages:
- Prekoma. It is characterized by the patient experiencing stupor, slowness of reaction, or, conversely, increased excitability. Basic reflexes are preserved, but mental activity is deformed.
- Superficial coma. The person is in a state of stupor or falls asleep. A complete blackout of consciousness does not occur; some simple movements are preserved.
- Deep coma. The patient spends all the time unconscious, muscle movement occurs reflexively. Reactions to external stimuli are weakened.
- Atonic coma. Reflexes disappear, all systems stop functioning independently, and the patient is connected to life support machines.
The last stage of a coma can most likely lead to death. However, medical practice knows cases when even the most severe patients were able to return to consciousness with partial or almost complete restoration of cognitive functions.
Diagnostics
The diagnosis immediately establishes the causes of the comatose case. The conclusion differentiates the condition from other similar disorders of consciousness. The following diagnostic methods are used:
- Anamnesis collection. They find out from the patient's relatives or witnesses whether the patient took medications, and whether empty jars or blisters of medications were found nearby. You should ask about the presence of chronic diseases of blood vessels, endocrine glands, and heart. Clarify that the patient may have voiced complaints. An important factor is the age of the patient and the speed of development of symptoms. Young people more often fall into this state after poisoning with sleeping pills or narcotic drugs. In elderly patients, the formation of a coma occurs against the background of heart attacks, strokes, and other cardiovascular diseases.
- Inspection. During the examination, the possible root cause of the coma is determined. Respiratory rate, pulse rate, blood pressure, body temperature, injection marks, bad breath, bruises are indicators on the assessment of which the establishment of a correct diagnosis depends.
- The patient's position can also characterize the severity of brain damage. During hemorrhages and meningitis, the patient’s head is thrown back, the neck muscles have a pronounced tone - signs of irritation of the meninges. Convulsive attacks, cramping spasms of individual muscles indicate the patient’s status epilepticus, the condition of eclampsia in pregnant women. Unexpressed paralysis of the limbs indicates a stroke, a complete absence of reflexes indicates deep lesions of the cortex and spinal cord.
- A differential feature distinguishing it from other disorders of consciousness was the study of the patient’s function to open his eyes to irritation in the form of sound or pain. If the response to sound and pain stimulation in the form of involuntary opening of the eyes persists, then this is not a coma. If the eyes remain closed, the case is considered comatose by doctors.
- The doctor carefully evaluates the ability of the pupils to respond to light. Its quality makes it possible to determine the damaged area of the brain, and also indicates the factor that provoked the coma. The clarity of the pupil's reaction to light indicates the future prognosis of the disease.
Pinpoint pupils that do not respond to bright light indicate alcohol or drug poisoning. If the pupils of the left and right eyes have different diameters, this is a sign of increasing intracranial pressure. Excessively wide pupils are a symptom of midbrain pathologies. If, when exposed to bright light, the reaction of the pupils is completely absent, their diameter remains wide, this is a very unfavorable symptom, which indicates imminent brain death.
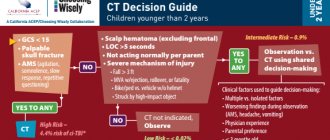
The development of medicine makes it possible to use hardware methods for diagnostic purposes to examine patients with impaired consciousness immediately upon admission to a medical institution. Performing head computed tomography (CT), magnetic resonance imaging (MRI) makes it possible to detect changes in areas of the brain, lesions, tumor-like neoplasms, and signs of intracranial hypertension. The conclusions obtained as a result of the tomograph study serve as the basis for determining treatment tactics - surgical or conservative.
X-rays of the head and spine in several projections are performed if MRI or CT is not possible.
A biochemical blood test can confirm a metabolic failure. Tests for the level of glucose, urea, acetone, and ammonia in the blood are carried out very quickly. The ratio of the content of electrolytes and blood gases is determined. In addition, the blood is examined for insulin levels, adrenal and thyroid hormones, for the presence of narcotic substances, tranquilizers and other toxic drugs, and bacterial blood cultures are performed to identify a possible infectious agent.
During an electroencephalogram (EEG), electrical impulses from the brain are recorded, which make it possible to determine the type of coma and understand what caused it - hemorrhage, poisoning or a tumor.
The role of communication with a person in a coma
There is no consensus on the benefits of communicating with a person in a coma. However, scientists have reason to believe that, to some extent, the patients' subconscious retains the ability to perceive external signals.
The patients themselves, who were lucky enough to emerge from a comatose state, report that their sensations were close to falling asleep. None of the respondents could accurately describe what happened while they were unconscious.
Although the benefits of communicating with comatose patients have not been proven, family members and acquaintances often express a desire to maintain contact with their loved ones. In this case, the recommendations are as follows:
- Introduce yourself and share positive news. You should maintain a calm, measured tone and an average volume of your voice.
- It is better to conduct a conversation with a patient in a coma as if he were conscious and acting as a listener.
- Relatives can express their support by sitting next to, touching, or holding the patient’s hand. Sometimes relatives read books aloud.
- There is a theory about the beneficial effects of music. People who are unconscious are allowed to play their favorite songs in their headphones.
“Are you hurt?”
“I worked for years with patients who were in the gray zone between life and death,” the neuroscientist recalled about this case. “That’s why I agreed to the experiment reluctantly: I had to disappoint relatives many times already, who were sure that the patient had finally begun to show signs of life. In the case of Scott Routley, I felt a special responsibility: the parents did not lose hope for so many years and created all possible conditions for their son. They hoped that he would not leave them without a final conversation. And I was incredibly happy when their expectations were rewarded."
The essence of the experiment is this: while the brain is being scanned by a tomograph, a person is asked questions. The glow in a particular part of the brain proves that it has been activated, and this allows you to receive answers. The scientist asked the comatose man: “Scott, please imagine that you are playing tennis!” In response, spots began to light up on the screen where the brain image was projected. Contact has been established. After a series of simple questions and subsequent obvious reactions on the screen, Adrian, with his parents' permission, asked, “Scott, are you hurt? If not, imagine yourself playing tennis again.” Fortunately, the same spots appeared on the screen as after the first question.
Loss of consciousness or coma? When to call an ambulance Read more
This result came as a consolation to many, many relatives of those who found themselves in the same position as Scott. The neuroscientist communicated with the physicist several more times, but a few months after the first contact was established, the patient died without leaving a coma from an infection.
This, by the way, is one of the most common causes of death for patients in a coma: a decrease in immunity is inevitable, as is an encounter with infections that always walk around hospitals...
How is rehabilitation after a coma?
Bringing a patient out of a coma is often not an easy task. However, doctors are making every effort to ensure that consciousness is restored and the person can return to a full life. For this purpose, various drug therapy regimens are used. In case of a favorable outcome, subsequent rehabilitation is carried out.
The main task at this stage is to create in the patient the mood for a complete recovery and return to his former life. Often, a comatose state and subsequent treatment becomes a difficult experience for a person, and he needs the help of specialists. You should seek support from specialized rehabilitation centers.
In Belarus, in 2004, a medical rehabilitation center was formed on the basis of the Republican Clinical Hospital in the village of Aksakovshchina, Minsk region. Anyone in need can get help here for free.
Anatomical and functional features of the central nervous system
Being the central regulator of all processes occurring in the body, the brain operates in an active metabolic mode. Its weight is only 2% of body weight (about 1500 g). However, for the uninterrupted functioning of the brain, 14-15% of the total volume of circulating blood (700-800 ml) must flow into and out of the cranial cavity every minute. The brain uses 20% of all the oxygen the body consumes. It is metabolized only by glucose (75 mg per minute or 100 g per day).
So, the physiological functioning of brain tissue depends on adequate perfusion with its blood, the content of a sufficient amount of oxygen and glucose, the absence of toxic metabolites and the free outflow of blood from the cranial cavity.
A powerful autoregulation system ensures smooth functioning of the brain. Thus, even with significant blood loss, the perfusion of the central nervous system is not impaired. In these cases, a compensatory reaction of centralization of blood circulation with ischemia of less important organs and tissues is activated, aimed primarily at maintaining adequate blood supply to the brain. The body reacts to another pathological condition - hypoglycemia - by increasing blood flow to the brain and increasing the transport of glucose here. Hyperventilation (hypocapnia) reduces blood flow to the brain; hypoventilation (hypercapnia) and metabolic acidosis, on the contrary, increase blood flow, promoting the removal of “acidic” substances from tissues.
With significant damage to brain tissue, insufficient autoregulation or excessive manifestations of the compensatory reaction of the inflow and outflow of blood, the brain cannot voluntarily change its volume. The closed cavity of the skull becomes its trap. Thus, an increase in intracranial volume by only 5% (with hematomas, tumors, hyperhydration, liquor hypertension, etc.) disrupts the activity of the central nervous system with the patient losing consciousness. In another pathology, excessive growth of cerebral blood flow leads to overproduction of cerebrospinal fluid. The brain tissue is compressed between the blood and the cerebrospinal fluid, swelling develops, and functions are impaired.
Traumatic destruction of brain tissue, edema and swelling, increased intracranial pressure, impaired circulation of cerebrospinal fluid, circulatory disorders and other damaging mechanisms lead to hypoxia of CNS cells. It manifests itself primarily as a disturbance of consciousness.
Mechanism of increase after an attack
If symptoms of a stroke are severe, accompanied by hyperthermia, the patient’s household should call a doctor. Before his arrival, the victim of an ischemic form of pathology can be given Ibuprofen, Paracetamol and Analgin.
When providing primary first aid, it is unacceptable to use strong analgesics, as well as antibacterial and steroid drugs.
In case of hemorrhagic cerebral stroke, the use of any medications before the arrival of an ambulance is prohibited.
Relatives should check the patient for reflexes and consciousness. Upon arrival of the ambulance, the patient is immediately taken to the clinic.
It is difficult to reduce the temperature during a stroke using medications. Hyperthermia is fought with other methods.
- Invasive methods. Intravenous injection of cooled saline solution.
- Catheter monitoring of temperature.
At elevated temperatures, brain cells are not properly oxygenated. This provokes the development of hypoxia, subsequent tissue necrosis and disruptions in cerebral regulation. To avoid such complications, patients have their temperature periodically measured during the first 12 hours after hospitalization.
Drugs for the treatment of post-stroke hyperthermia are prescribed depending on the specific cause that provoked the increase in temperature.
If a high temperature during a stroke is associated with a direct disruption of the hypothalamus, then fever, some time after the stroke, indicates the development of an inflammatory process in the body.
In this case, an increase in body temperature is a protective reaction of the body, but at the same time, it interferes with the normal restoration of cells.
With hyperthermia, cell metabolism accelerates, and against the background of a stroke, this leads to tissue hypoxia. Memory impairment occurs, the functioning of internal organs deteriorates, and stroke treatment becomes ineffective.
If the temperature suddenly becomes high some time (more than 1 day) after a brain stroke, this is an alarming symptom that indicates the development of complications. In most cases, the cause of such hyperthermia is a secondary inflammatory process in the body that developed against the background of a stroke.
- pneumonia;
- cystitis;
- pyelonephritis;
- bedsores;
- deep vein thrombosis.
Sometimes the cause of hyperthermia in the post-stroke period is an allergic reaction to medications that are used in the treatment of stroke.
This complication option is the most favorable for the patient.
It is enough to cancel the inappropriate drug, and the indicators should return to normal.
To determine the allergen, it is necessary to take an analysis.
If the patient previously had chronic infectious diseases, then a stroke will certainly provoke an exacerbation of the inflammatory process, and sometimes it serves as an impetus for the development of a disease for which there were previously only prerequisites. This picture is especially typical for elderly patients with weakened immune systems.
Therefore, it is very important to tell the doctor what health problems the person had before the stroke and provide a medical history card for review. In this case, doctors will be able to anticipate the risk of complications and prescribe additional treatment in a timely manner.
How to help a patient?
First aid to a stroke patient should be provided as quickly as possible, even before the ambulance arrives. If the temperature has increased, it is necessary to give the patient an antipyretic non-steroidal anti-inflammatory group (paracetamol, ibuprofen, aspirin, analgin) in a dosage of no more than 2 tablets and put him to bed. You can give any drug only after making sure that the person’s swallowing reflex is not impaired.
It often happens that the temperature is poorly controlled by medications or does not decrease at all. There are two alternative methods for reducing body temperature:
- Invasive, when the patient is injected intravenously with a cooled saline solution. You should not use this method on your own, since there is a high risk of complications in the form of increased hemorrhage, thrombosis, etc.;
- Non-invasive when the temperature is reduced by cooling the outer skin. The patient is covered with heating pads with ice, or special helmets are used in which coolant circulates.
In the post-stroke period, it is important to provide the patient with quality care, as well as minimize the risk of contracting viral and infectious diseases.
These measures will be the best prevention of complications. If you cannot avoid them, you must follow these instructions:
- For bedsores, use special ointments and creams that do not require rinsing;
- If a tracheostomy is installed, you need to check its patency daily and treat the skin around it with an antiseptic (furatsilin solution);
- If a patient has pneumonia, it is imperative, several times a day, to turn him from one side to the other to ensure the discharge of sputum;
- Thermometry in patients with stroke should be carried out at least 2 times a day, even if the condition improves. Such patients may simply not feel the fever.
Consequences of hyperthermia
Hyperthermia is a consequence of extensive hemorrhage in the brain. Elevated temperature during a stroke is fraught with the following consequences:
- due to a lack of oxygen in the brain tissues, metabolic processes are accelerated;
- inflammation causes cell death, as well as disruptions in cerebral regulation;
- with an ischemic stroke, the affected area expands due to cerebral infarction;
- brain damage;
- damage and subsequent death of brain tissue.
Hyperthermia during a cerebral stroke is always a bad sign; this condition is especially dangerous for an old person. You should call an ambulance, before it arrives, bring the readings down to 37.5 0C as soon as possible and wait for the doctor to arrive.
Elevated temperature during a stroke can cause a number of irreversible consequences that result in disability, coma or death. In any case, hyperthermia in such patients requires special attention. It is necessary to apply all possible methods to ensure that body temperature returns to normal as quickly as possible. As long as the temperature remains above 37.5-38ºС:
- the area of brain damage increases;
- due to hypoxia, all internal organs suffer;
- a large number of dead cells causes an inflammatory process, and tissue necrosis may begin.
Normal body temperature significantly increases the chances of a person who has had a stroke making a full recovery.
First aid
If you suspect the initial signs of a cerebral coma, you should urgently call an ambulance. The victim needs to take a horizontal position, allow access to fresh air and remove clothes that are constricting the chest. It is imperative to calm the victim. Do not leave the patient until specialists arrive!
Clinical Brain Institute Rating: 3/5 — 19 votes
Share article on social networks