Surgeries on the head are no more dangerous than many others: the surgeon’s intervention is often performed when there is already an existing soft tissue injury or when pathology develops (cysts, tumors, burn wounds, etc.). Care after surgery on the head is similar to procedures after a surgeon intervenes in another place on the human body.
The color of the bandage and its moisture content with blood will tell you about the progress of recovery: after head surgery, blood flows more often and longer than on other parts of the body due to the constant blood supply.
Severe bleeding, when the bandages are completely soaked in blood, should be under medical supervision, seek help.
The resident will suggest a solution:
- Change the bandage
- Apply a second bandage
- Apply cold.
Recovery
The skull repair procedure may vary depending on the type of surgery performed and the physical condition of the patient.
As a rule, they try not to keep the patient in for too long and, when the condition stabilizes, they are sent home to more quickly restore the rhythm of life. A long stay does not allow the immune system to strengthen, which leads to an increased risk of getting an infection in the hospital or after discharge. After the operation, the patient is transferred to a ward where his condition is constantly monitored. After getting rid of anesthesia, the breathing tubes are removed, and then the patient is sent to the neurology and intensive care department for further observation, the period of which does not exceed 2 weeks. During this period, you need to lead a sedentary lifestyle as much as possible, try to make as little body movements as possible.
After discharge, you should take all medications prescribed by your doctor, but you should not exceed or, conversely, decrease the dosage without first consulting your doctor. The patient is prohibited from driving, performing any physical or mental activity, or performing exercises until the doctor gives permission. Not following your doctor's instructions may cause difficulty in recovery and unwanted side effects in the future.
Once cleared by your surgeon, you can begin a program of early exercise, such as stretching your neck and back. You should also take frequent walks in the fresh air, although initially their duration should be minimal.
The recovery process can last up to 4 weeks, and by the final date it will be possible to return to your normal work
However, you will still need to take precautions until your rehabilitation is complete, which can last up to 3 months. Ignoring your doctor's instructions may result in the above consequences, as well as paralysis, loss of mental function, and permanent brain damage.
Craniotomy or craniotomy is a complex medical operation known since ancient times. It is carried out in special cases when the doctor needs to gain access to the brain and its membranes, emerging pathologies and blood vessels. Modern medicine makes surgery safer for the patient compared to past times when it was associated with high mortality.
Disease statistics.
According to the World Federation of Neurological Societies, at least 15 million strokes are recorded annually in the world.
In Russia, the incidence of stroke is more than 450,000 new strokes per year . In Moscow, the number of patients with stroke for a long time (almost 20 years) has not decreased below 36,000 patients per year.
In the United States, stroke is the third leading cause of death, with 500,000 strokes occurring annually. Stroke and its complications kill 150,000 people a year in the United States. 2 million Americans have suffered the consequences of a stroke.
Ischemic stroke in approximately 95% of cases is caused by atherosclerosis of the arteries of the head and necks, damage to small cerebral arteries due to arterial hypertension, diabetes mellitus or cardiogenic embolism.
Risk factors . The main risk factors include age, arterial hypertension, diabetes mellitus, hypercholesterolemia, atherosclerotic stenosis of the cerebral and precerebral arteries, smoking, heart disease (atrial fibrillation, myocardial infarction, artificial heart valve, rheumatic heart valve disease, myocardiopathy, bacterial endocarditis), excessive consumption salt, as well as alcohol abuse. The risk of stroke increases significantly in people who have had a stroke or transient ischemic attack.
Mortality after an ischemic stroke is 20% during the first month and about 25% during the first year. 6 months after a stroke, disability occurs in 40% of surviving patients.
The course, outcome and prognosis of a stroke are determined by the localization and volume of cerebral infarction, the severity of cerebral edema. If motor functions and speech do not improve after 2 weeks. after a stroke, the prognosis for their recovery is unfavorable. Of those who survive, about 60-70% of patients have disabling neurological disorders by the end of the month from the moment of stroke.
| Blood supply to the brain |
It should be emphasized the catastrophic consequences of ischemic stroke - during the first 5 years, up to 85% of patients die or remain disabled and only 15% of patients fully recover. It should be added here that even among surviving patients, 50% have a second stroke in the next 5 years of life; its risk is especially high in the first year after the disease . In Russia, about 100 thousand recurrent strokes are registered annually. The likelihood of death and disability with a second ischemic stroke is higher than with the first.
Ischemic stroke clinic.
Ischemic stroke usually develops within seconds or minutes (less often over hours or days) and is manifested by motor, speech and/or other focal neurological disorders. Disorders of consciousness, vomiting, and intense headache are not observed in most cases, with the exception of infarctions in the brain stem, cerebellum, or extensive hemispheric infarctions. Ischemic stroke often occurs during sleep or immediately after sleep, but it can also occur during exercise, taking a hot bath, drinking alcohol, emotional stress, or without any precipitating factors.
Features of ischemia. With local cerebral ischemia, around the area of irreversible changes there is nervous tissue, the blood supply of which is below the level necessary for normal functioning, but above the critical threshold of irreversible changes - “ischemic penumbra”, penumbra. Cell death in the area of the “ischemic penumbra” leads to an increase in the size of the infarction. However, these cells can maintain their viability for a long time, so the development of irreversible changes in them can be prevented by restoring blood flow. The duration of the period during which restoration of nerve cells in the “ischemic penumbra” region is possible has not been precisely established. Although for most nerve cells this time is limited to hours (or 2-3 days), a longer period can be assumed for some neurons.
Basic diagnostic methods.
• CT scan of the brain and CT angiography or MRI of the brain. • MR angiography of the branches of the aortic arch, intracranial vessels. • Cerebral angiography (if indicated). • Doppler ultrasound of the aortic arch vessels (brachiocephalic arteries). • Dopplerography of cerebral vessels. • ECG and ECHO-CG, Holter monitoring.
| 1. CT scan of the brain with an ischemic stroke in the basin of the left middle cerebral artery (focus of hypodense density in the left parietal and temporal lobes and in the region of the subcortical nuclei on the left). 2. Angiography of the same patient (critical stenosis of the left internal carotid artery leading to ischemic stroke). |
Treatment of ischemic stroke is carried out only in a hospital, according to developed regimens using antiplatelet agents, anticoagulants, as well as vascular, nootropic, antihypoxic and other drugs at the discretion of the attending physician.
All patients must be examined to identify the causes of stroke and, based on the results, a decision is made on the possibility of a surgical approach to treating an existing stroke and preventing recurrences. This requires a comprehensive examination and taking into account indications and individual contraindications for surgery.
Indications for surgical treatment in cases of ischemic stroke, transient ischemic attacks and chronic cerebral ischemia due to narrowing of the lumen of the vessel (of various natures) are determined strictly individually taking into account a comprehensive assessment of the patient’s condition and the results of all examinations of the individual patient.
Types of operations:
• carotid endarterectomy
| Scheme of the operation - carotid endatherectomy (the atherosclerotic plaque and thrombotic masses that caused the development of ischemic stroke are removed from the lumen of the vessel supplying the brain) |
• application of extra-intracranial anastomoses
| Scheme of the operation - application of extra-intracranial microanastomosis (EICMA). An additional source of blood supply to the brain is provided from the external carotid artery. |
• angioplasty and stenting of relevant vessels
Indications for examination and deciding on the possibility of reconstructive surgery:
- Acute occlusion of the intracranial artery.
- Conservative therapy is ineffective and against its background, attacks of transient cerebral ischemia recur.
- Occlusive lesion (severe stenosis or kinking) of both internal carotid arteries.
- Occlusive lesions of the arteries of the vertebrobasilar system.
- Chronic cerebral ischemia.
Craniotomy: when necessary, implementation, rehabilitation
Craniotomy is rightfully considered one of the most complex surgical interventions. The operation has been known since ancient times, when they tried to treat injuries, tumors and hemorrhages in this way. Of course, ancient medicine did not allow one to avoid various complications, so such manipulations were accompanied by high mortality. Now trepanation is performed in neurosurgical hospitals by highly qualified surgeons and is intended, first of all, to save the patient’s life.
Craniotomy consists of creating a hole in the bones through which the doctor gains access to the brain and its membranes, vessels, and pathological formations. It also allows you to quickly reduce the growing intracranial pressure, thereby preventing the death of the patient.
The operation has strict indications, and the obstacles to it are often relative, since in order to save the patient’s life, the surgeon can neglect concomitant pathology. Craniotomy is not performed in terminal conditions, severe shock, septic processes, and in other cases it can improve the patient’s condition, even if there are serious disorders of the internal organs.
Historical reference
In neurosurgery, trephination is the making of a hole in some part of the skull to gain direct access to brain tissue. However, such surgery should not be considered an invention of modern medicine. Archaeological finds indicate that our ancestors could have drilled holes in the skull for medicinal purposes several thousand years ago. Since the Late Paleolithic era (40-11 thousand years ago), trepanation has been used in almost all corners of the planet. The operation was used by ancient Greek and Roman doctors, healers of several parts of Africa, South America and the South Pacific.
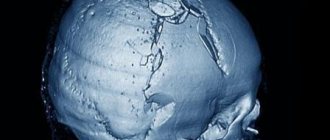
Hippocrates proposed trepanation as a way to treat head wounds, including removing bone fragments from the brain after injury. For this procedure, his followers came up with a special drill. Prehistoric trepanations in the culture of ancient civilizations of Peru were performed with a ceremonial knife called a tumi. Residents of the southern regions of the Pacific Ocean performed surgery using sharply sharpened shells. In Europe, flint and obsidian were used for the same purposes.
The purpose of trephination was not always to open access to the brain for further manipulation. In ancient times, a hole in the skull often served as an outlet for evil spirits, which were considered the cause of disease. Also, the hole in the skull was seen as a kind of channel for obtaining special knowledge and spiritual experience. In Egypt, pharaohs underwent such an operation, presumably to make it easier for the soul to leave the body after death.
Consequences after craniotomy
The severity of the consequences in the postoperative period depends on the reason for the operation, the age of the patient, and the presence of concomitant diseases. If neurological disorders were not immediately detected after trepanation, this does not mean that they will definitely not arise in the future. If the cerebral cortex is damaged, hearing and vision impairment of varying severity, up to complete loss, may occur.
The consequence may be a stroke due to thrombosis or thromboembolism. During trephination for abscesses, pathogenic flora may spread through the membranes of the brain, which will lead to meningitis and encephalitis. After many hours of anesthesia, disorders of the respiratory and cardiovascular systems are possible. If the neurovascular bundles are damaged, numbness, complete loss of sensitivity, and movement of certain areas of the skin, muscles, and limbs are possible. Postoperative consequences can manifest themselves in the form of mental and behavioral disorders.
How is craniotomy performed?
There are 6 main steps during a craniotomy. Depending on the underlying problem being treated and the complexity, the procedure may take 3 to 5 hours or more.
Step 1 - patient preparation. No food or drink is allowed after midnight the night before surgery. Patients with craniotomy are admitted to the hospital in the morning. General anesthesia is administered intravenously while the patient lies on the operating table. The person falls asleep, and his head is in a 3-pin cranial fixation device, which is attached to the table and holds the head in an upright position during the procedure. Inserting a lumbar (spinal) drain into the lower back helps remove cerebrospinal fluid (CSF), allowing the brain to relax during surgery. The patient may be given the drug Manit, which relaxes the brain.
Step 2 - skin incision. After the scalp has been coated with antiseptic, a skin incision is made, usually behind the hairline. The surgeon tries to ensure a good cosmetic result after the operation. Sometimes the hair can be shaved sparingly.
Step 3 - performing a craniotomy, opening the skull. The skin and muscles rise to the bone. Next, the surgeon uses a drill to make one or more small holes in the skull. By inserting a special saw through the holes of the burrs, the surgeon reduces the contour of the bone flap. The cut piece of bone is lifted and exposed to the protective covering of the brain called the dura mater. The bone flap is stored securely until it is replaced at the end of the procedure.
Step 4 - opening the brain. After opening the dura mater with surgical scissors, the surgeon places it back to expose the brain. Retractors placed on the brain need to be repaired or removed. Neurosurgeons use special magnifying glasses (loupe, or operating microscope) to see fine nerves and blood vessels.
Step 5 - fix the problem. Because the brain is tightly enclosed within the bony skull, tissue cannot be easily moved to the side, making it difficult to access and correct any problems. Neurosurgeons use a variety of very small instruments to work deep within the brain. These include long-handled scissors, dissectors, drills, lasers, ultrasonic aspirators (to break up tumors and suck up debris), and computer imaging guidance systems. In some cases, monitoring is used to stimulate specific cranial nerves while the response is monitored in the brain. This is done in order to preserve the function of the nerves and ensure that they are not damaged later during the operation.
Step 6 - closing the craniotomy. With the problem of removing or repairing retractors, the dura mater, closed with sutures, is also removed from the brain. The bone flap is placed back in its original position and secured to the skull with titanium plates and screws. The plates and screws are permanently left to support the skull, which can sometimes be felt under the skin. In some cases, drainage tubes may be placed under the skin for several days to remove blood or surgical fluid. The muscles and skin are stitched back together.
The entire procedure lasts 180-240 minutes.
Provocateurs of hemorrhagic stroke
The trigger for the appearance of HI can be quite a variety of factors that have a negative impact on intracranial hemodynamics and the condition of the cerebral vessels:
- persistent arterial hypertension (in 50% of cases);
- cerebral amyloid angiopathy (12%);
- oral administration of drugs from the anticoagulant spectrum (10%);
- intracranial neoplasms (8%);
- other causes are arteriovenous and cavernous malformations, thrombosis of the cerebral sinuses, aneurysms, vasculitis of intracranial vessels, etc. (20%).
Many of the patients with a history of hemorrhagic stroke have diabetes mellitus. It is a proven fact that diabetics, like hypertensive patients, are at risk. In long-term diabetes mellitus, blood vessels, including cerebral ones, are destroyed due to modification of blood chemistry with a predominance of glucose. If, against the background of elevated blood sugar, there is a tendency to constant increases in blood pressure, the likelihood of a hemorrhagic stroke increases by 2.5 times.
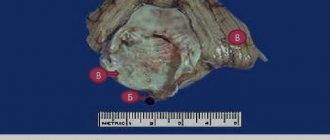
Pathogenetically, a hemorrhagic effect can develop as a result of rupture of a vessel (the predominant mechanism) or the leakage of blood elements into the surrounding brain tissue through the walls of capillaries due to their impaired tone and permeability. In the second option, there is no rupture and, as such, profuse hemorrhage. Just a small vessel allows blood to pass through pointwise. But even small-point hemorrhages, merging, can turn into very extensive foci, with no less fatal consequences than after a rupture of an artery or vein.
Craniotomy - types
To eliminate many pathologies, trepanation is used, the types of which are named based on the location of access to the brain and the method of performing the operation. The bones of the skull (on the vault) are represented by several plastics, covered with periosteum on top and adjacent to the braincase below. If the periosteum, as the main nourishing tissue, is damaged, there is a risk of necrosis and bone death. To avoid this, craniotomy is performed using the following methods:
- classical osteoplastic;
- resection;
- for the purpose of decompression;
- conscious operation;
- Stereotaxy is a study of the brain using a computer.
Osteoplastic craniotomy
The most famous type of craniotomy, a classic method of opening the skull, during which a small section of the parietal bone is sawed out without damaging the periosteum. The cut piece is connected with the periosteum to the cranial vault. The pedicled skin flap is folded back and, after the operation, is placed in place or removed. The periosteum is sutured. After surgery, no bone defect is observed. Trepanation (osteoplastic) of the skull is divided into two types:
- With cutting out a skin-periosteal-bone flap at the same time (according to Wagner-Wolf).
- With cutting out a skin-aponeurotic flap, which has a wide base, and then an osteoperiosteal flap on a narrow stalk (Olivecron trepanation).
Decompressive trephination
One of the methods designed to reduce intracranial pressure and improve the condition (and function) of the brain is decompressive craniotomy (DCT) or Cushing trephination, named after the famous neurosurgeon. With it, a hole is created in the bones of the skull, through which the harmful element that caused the resulting hypertension is eliminated. This could be pus, blood, cerebrospinal fluid, or edematous fluid. Negative health consequences after surgery are minimal, rehabilitation is short.
Resection trepanation
Resection surgery has a less favorable prognosis for rehabilitation; craniotomy is performed by applying a burr hole and then expanding it to the required size (for this, wire cutters are used). The sawed area is removed along with the periosteum without possible restoration. The bone defect is covered with soft tissue. As a rule, this technique is used when trepanation of the posterior cranial fossa is necessary, as well as treatment of cranial wounds.
Awake craniotomy
One of the modern methods of surgery is trepanation without anesthesia. The patient is conscious, his brain is not turned off. He is given relaxation drugs and local anesthesia is injected. Such intervention is required when the pathological area is located too close to the reflexogenic zones (and there is a danger of damaging it). During the operation, surgeons constantly monitor the patient’s condition and the activity of organs, monitoring the process.
Rehabilitation after craniotomy
The first day after the end of the operation, the patient is in intensive care, connected to devices. The next 3-7 days should be spent in a hospital under the supervision of doctors. This period of time allotted for recovery after craniotomy is very conditional; if a person experiences complications, it can increase. During the rehabilitation period, the patient is prescribed medications:
- painkillers;
- antibiotics - to prevent inflammation;
- antiemetics;
- sedatives;
- anticonvulsants;
- steroid drugs that remove excess water from the body.
The sterile dressing is removed from the wound within 24 hours. The skin around the wound should be constantly treated and kept clean. After 2 days, the patient is allowed to get up and walk a little. After discharge home, rehabilitation continues. The following conditions must be observed:
- do not lift objects weighing more than 3 kg;
- stop smoking;
- eliminate nervous unrest;
- take a course with a speech therapist to restore speech;
- bend over as little as possible;
- go on a diet prescribed by a doctor;
- Take short, supervised walks every day.
You should very carefully monitor the emotional state of a person after surgery. Some people become susceptible to depression and nervous disorders
It is necessary to surround them with care and attention, to protect them from unnecessary worries. If you can’t cope with anxiety on your own, you need to consult a psychologist.
What will happen to the wound?
A scar will remain on the scalp, but the advantage of this arrangement is that it can be masked with a hairstyle; after a week the scar will not be visible.
Scars may not remain with minimally invasive intervention through the nasal passages or blood vessels; treatment of such wounds is easier.
The dressing is carried out in the hospital on the first day, then a dry cloth - pad accompanies the patient at home. The bandage should not be allowed to get wet; the patient should be helped to keep the bandages dry. You can resort to careful hair washing after a week.
It is important to comply with sanitary standards and wash your hands with soap and water before touching the bandage: this applies to the patient, caregivers and medical staff.
After healing, a thin scar in the form of a white stripe remains at the intervention site, which is successfully hidden in the hair.
What are the consequences for children and adults?
- Asthenia – constant feeling of fatigue, depression, sensitivity to atmospheric phenomena, insomnia, tearfulness;
- Speech disorders are common in both children and adults. It is difficult to immediately determine whether this phenomenon is temporary. So you just have to wait and watch;
- Psychosis;
- Forgetfulness;
- Paralysis;
- Convulsions (more often in children);
- Loss of coordination (more pronounced in children);
- Hydrocephalus (in children, less often in adults);
- ZPR (in children).
Infectious complication
As after any surgical intervention, trepanation negatively affects the body's protective functions, which increases the risk of infection.
Brain infections are extremely rare, but the wound itself can easily become infected by poorly handling the instruments
The lungs, intestines, and bladder suffer from infection. All these organs tend to catch infections first.
After surgery on the skull, the likelihood of developing a number of infections increases significantly, and infection of the brain tissue itself occurs much less frequently, which is associated with appropriate sterilization of the area undergoing surgery.
The greater risk of infection is the lungs, intestines and bladder, the functions of which are regulated by parts of the brain. This circumstance is largely due to forced restrictions on a person’s mobility and lifestyle changes after surgery. Prevention of such complications is physical therapy, diet, and sleep. Treatment of infections is carried out medically - by prescribing appropriate antibiotics.
Blood clots and blood clots
Pathological processes and changes in brain tissue, poor mobility in the postoperative period can cause blood stagnation, which causes the formation of blood clots. The veins in the legs are most often affected.
If a blood clot breaks loose, it can migrate throughout the body, settling in the lungs or heart. Very often, the detachment of a blood clot leads to death. There are also cases of pulmonary artery thrombosis, which is a very dangerous consequence and requires immediate intervention. This disease leads to very serious consequences, including death.
The best prevention against clots is exercise, plenty of fresh air and anticoagulants (blood thinners).
Neurological disorders
To speed up the healing process, steroidal anti-inflammatory drugs are prescribed.
With more serious errors made during surgery, pathologies may last longer. There are many causes for symptoms, and they all depend on more than one factor.
Bleeding
Bleeding is one of the most common phenomena after trepanation. For several days after surgery, the vessels may bleed. This problem is eliminated by drainage. Usually there is little blood and it does not cause problems.
But there are cases when the bleeding is so profuse that repeated trephination has to be done to stop it and prevent more serious consequences.
Blood that accumulates in the cranial cavity can affect motor centers or nerve endings, causing seizures. In order to avoid such manifestations during surgery, the patient should be given intravenous anticonvulsant drugs in advance.
During facial surgery
Local or general anesthesia for facial surgery causes vomiting in the patient after surgery. The soft tissues swell greatly, the openings of the eyelids, nasal passages, and mouth narrow. To alleviate the condition, you need to rinse the eyelid with a warm saline solution (9% NaCl): moisten a cotton pad, ball or piece of bandage and gently blot the eyelid fold; the materials must be sterile.
If there is a tumor around the lips, nutrition is supplied in liquid form until the organs for eating are restored. Talk to such a patient, but do not let him answer, let the oral cavity be at rest.
Make sure that after oropharyngeal operations the patient can breathe calmly; particles of blood and saliva can develop pneumonia if they enter the lungs. During surgery on the jaw/tongue or others with subsequent swelling inside the cavity, oxygen is supplied through the nose with a special catheter.
A pillow is not needed; during facial interventions, the patient’s head is kept tilted to the right or left while lying on his back.
It is recommended not to sneeze, not to cough, not to cough up secretions, and not to swallow saliva if possible. Rest in this area will help the tissues heal in a shorter period of time.