The rehabilitation program after brain surgery is usually developed individually, taking into account all the characteristics of the patient and the disease. The directions, goals, and objectives of rehabilitation after brain surgery are determined by the characteristics of the disease for which surgical treatment was performed, the technique of the operation itself, and the course of the postoperative period.
We help patients with the consequences of brain surgery in the form of motor disorders (paralysis, paresis, impaired motor coordination), speech and swallowing disorders, and disorders of higher mental functions (memory, attention, thinking).
Initial consultation with a rehabilitation specialist
+8
Record
Methods for plastic surgery of a bone defect of the skull
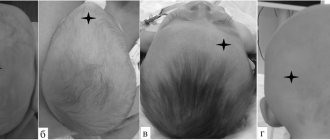
A bone defect in the skull is a hole in it that forms after neurosurgical intervention on the organs of the central nervous system or as a result of trauma.
Let's talk in more detail about skull defects in medical practice. After removing a section of bone and creating a hole in the skull, patients experience not only psychological discomfort, but also the so-called “trepanned skull syndrome.” In both cases, the hole must be closed with an implant. And now about everything in more detail.
4.Preparation for cranioplasty and rehabilitation
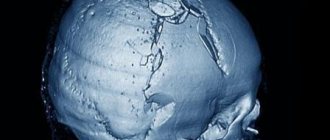
Implant modeling is based on data obtained from preoperative diagnostics. The most informative methods for examining the skull are craniography and computed tomography.
. Based on the results of a thorough examination of the patient, it is possible to manufacture an implant by photopolymerization of a liquid monomer using laser stereolithography before surgery.
Preoperative production of missing skull fragments is especially important in the presence of complex or multiple defects. Finished implants can be slightly modified and brought into absolute compliance with the parameters of the defects during cranioplasty. Creating an implant before surgery allows you to minimize the time of surgical intervention and reduces the risk of complications to a minimum.
As rehabilitation measures
After cranioplasty, the patient undergoes dehydration therapy. A course of antibiotics may also be prescribed
Consequences of skull defects
The bones of the skull not only protect the brain from mechanical damage. The absence of one area can cause a lot of unpleasant symptoms or complications for the patient. It is their presence that serves as a direct indication for surgical plastic surgery.
It could be:
- Headache. It occurs not only at the site of the defect, but also affects other areas. Most often, the symptom intensifies or occurs when there is a change in atmospheric pressure and air temperature. The so-called meteosensitivity appears.
- "Astheno-neurotic syndrome." These include complaints of absent-mindedness, decreased concentration, difficulties in solving intellectual problems, frequent mood swings, decreased ability to withstand stress and tolerance to alcohol.
- Protrusion of the contents of the skull outward. When coughing or sneezing, physical stress or exertion, part of the brain substance can protrude through an opening in the skull, under the skin. This leads to traumatization of internal tissues at the edges of the bone defect.
- Symptomatic epilepsy.
- Mental disorders.
Craniotomy
Like any other part of the body, the brain is susceptible to problems such as bleeding, infection, injury, and other damage. There is a need for surgery to diagnose or treat problems. Craniotomy (craniotomy) is a type of brain surgery. There are several types of brain surgeries, but recovery from trephination is the same as most cases. It is performed most often.
Craniotomy at the Assuta clinic opens up unlimited possibilities in the field of correction of complex diseases and brain injuries. The advantages of visiting a private medical hospital are undeniable:
- Treatment is carried out by the country's best neurosurgeons, who head specialized departments of Israeli hospitals and have undergone training in leading Western clinics.
- Revolutionary technical equipment of operating rooms, the presence of robotic systems, navigation systems.
- Fast turnaround time for organizing treatment—diagnosis and drawing up a therapeutic protocol take only 3-4 days.
We are waiting for you for treatment in specialized departments of the Assuta network. Affordable prices, professional approach, individual treatment regimens.
There are a number of lesions and anomalies that affect the skull and its contents and require a craniotomy:
- Scull. The most common problem is a benign tumor.
- Brain. The most common reasons for treatment are gliomas, metastases to the brain from other organs, an abscess (localized infection).
- Shells. These tissues mainly affect benign neoplasms - meningiomas, which increase in size and put pressure on the brain, leading to its damage.
- Blood vessel. The vessels at the base of the brain can be affected by an aneurysm, which can lead to their rupture and bleeding around the brain (subarachnoid hemorrhage).
- Cerebrospinal fluid. The occurrence of an obstruction in the circulation of the cerebrospinal fluid leads to hydrocephalus (cerebral edema), which in some cases requires trepanation.
In what cases is craniotomy performed - general indications:
- Examination of visible brain problems.
- Serious traumatic brain injury or head injury.
- Removal of a blood clot or hematoma.
- Biopsy – taking a tissue sample to check for cancer cells.
- Drainage of a brain abscess.
- Decreased pressure in the skull due to swelling.
- To control bleeding caused by an aneurysm.
- Restoration of blood vessels.
- Benign and malignant brain tumor.
- Nervous disorders.
- Brain infections.
If left untreated, any condition requiring surgery will cause further damage.
Types of craniotomy
There are several methods of craniotomy, the choice is influenced by the type of operation that follows:
- Traditional trepanation - a bone flap or part of the skull is removed at the beginning of the operation and returned to its place at the end.
- An endoscopic craniotomy is performed through a small hole in the skull using an endoscope.
- Stereotactic trephination - the standard method is complemented by MRI and CT studies. As a result, the surgeon receives a three-dimensional image with precise localization of the lesion. The advantage of the technique is that it clearly separates healthy tissue from pathological ones.
Preoperative preparation
Diagnosis at the Assuta clinic may include a physical examination, blood tests, ECG, and chest x-ray. Neuroimaging is carried out using CT or MRI, arteriogram.
Before surgery, the patient may be prescribed medications to relieve anxiety and reduce the risk of seizures, swelling, and infection after surgery. The use of blood thinners (heparin, aspirin) and non-steroidal anti-inflammatory drugs (ibuprofen, Motrin, Advil) is correlated with an increased likelihood of thrombus formation after craniotomy. Their use is stopped at least 7 days in advance.
When a brain tumor is diagnosed, steroids are prescribed. They eliminate swelling caused by the tumor. Treatment continues after craniotomy as prescribed by the doctor. It is important to follow the instructions carefully. A consequence of taking a steroid is stomach irritation. To reduce it, you need to take the tablets with food or a glass of milk. Sometimes medications are prescribed to prevent irritation.
1-2 weeks before surgery, the patient stops smoking, chewing tobacco and drinking alcohol. These actions cause complications during and after surgery and slow down the healing of the operated area.
The nurse will instruct you when to stop eating and drinking before your craniotomy, usually 8 to 12 hours before the procedure.
The patient at the Assuta clinic is provided with hospital clothes and special stockings that help prevent deep vein thrombosis. After surgery, there is a risk of this undesirable consequence due to prolonged lack of movement.
The surgeon talks with the patient about the operation, side effects and complications. The patient signs the consent form. The patient also meets with the anesthesiologist.
How is craniotomy performed?
Traditional craniotomy includes the following steps:
- The hair on the operated area is shaved.
- The patient is given general anesthesia. A local anesthetic is injected into the scalp to reduce post-operative pain.
- The head is fixed on a special headrest so that the operated area is accessible. Movement is kept to a minimum by holding the head in place using a special device with three bolts placed on the outer surface of the skull.
- Using a preliminary scan and the use of a neuronavigation system, the neurosurgeon determines the most suitable location for trepanation. The procedure begins with an incision in the scalp.
- Using a high power drill, small holes are drilled into the skull.
- A craniotome (a surgical instrument for drilling into the skull) is used to create a removable bone flap (it is formed between the holes). This opens up access to the brain.
- Further, depending on the diagnosis, blood vessels are restored, a blood clot or tumor is removed.
- At the end of the operation, the bone flap is placed in place, fixed with special clamps, and the muscles and skin are sutured. A drain is placed inside the brain to remove excess blood and secured with one suture. This way the wound heals faster.
The duration of the surgical intervention is about 2.5 hours.
Recovery after craniotomy
The patient regains consciousness in the intensive care unit of the Assuta clinic. Nurses provide specialized care. An oxygen mask is used for several hours until the patient recovers from anesthesia.
Immediately after craniotomy, the pupil reaction is tested, after anesthesia, the mental state and movement of the limbs (arms and legs) are assessed.
Blood pressure is carefully monitored along with pulse. A catheter inserted into the artery can be used to continuously monitor pressure. Intracranial pressure is monitored through a small catheter placed inside the head and connected to a pressure gauge.
Nurses take blood samples to determine the level of red blood cells and the amount of sodium and potassium.
An intravenous infusion is provided - saline solution enters the patient's body. When the patient is able to independently take food and liquid, the infusion is removed.
Soon after surgery, the patient begins to perform breathing exercises to cleanse the lungs. He will be able to get up about a day after the trepanation.
Medicines are prescribed to control pain, swelling and cramps. Antibiotics are prescribed to prevent infections.
The drainage is removed the next day. Swelling and bruising will be present on the face for the first time.
Surgical staples are removed 5-7 days after craniotomy. Do not wet your head until the staples are removed.
Extract
The patient usually stays in the clinic for five days, in some cases longer. Medicines that will be needed after surgery are prescribed.
Long-term observation is required if it is an infection or tumor.
Infection suggests a condition such as a brain abscess. The doctor will prescribe specific antibiotics for the infectious agent causing the abscess. In some cases, the treatment lasts several months.
Follow-up care for a tumor depends on its nature - benign or malignant.
Patients with benign tumors are observed by doctors for several years to ensure that there are no relapses. If the disease returns, the operation is repeated or radiation therapy is given.
Malignant tumors have a different perspective. Additional treatment methods are used:
- Irradiation is carried out after removal of metastatic foci and neoplasms that have arisen directly in the brain, for example, glioblastoma. Survival rates double after surgery followed by radiotherapy.
- Chemotherapy is used for glioblastoma, but often helps only slightly and also causes unwanted side effects.
- Immunotherapy improves the functioning of the immune system. For glioblastoma, the tumor is often removed during surgery to make a vaccine. The administered vaccine stimulates blood cells to create lymphocytes that will find and attack the pathological focus. Early studies have shown that immunotherapy improves survival in some patients with minimal side effects.
Rehabilitation after craniotomy
Full recovery takes up to two months, but more often patients return to a full life in less time.
The following factors influence recovery:
- Type of traumatic brain injury.
- The severity of the injury.
- Complications.
- The presence or absence of neurological problems.
- Type of operation performed.
- Side effects or complications of postoperative treatment.
- Age and general health, including the presence of other diseases.
You may feel tired and restless for up to eight weeks after your craniotomy. It's normal to need a nap in the afternoon. Returning to work can be discussed with your doctor. If the work activity does not involve stress, they begin it after about 6 weeks.
Some patients require physical or occupational therapy. Sometimes you need the help of a speech therapist for speech difficulties. These methods help to cope with any neurological problems.
The following activities should be avoided during recovery:
- Driving. The car can be driven after 3 months.
- Contact sports – at least one year.
- Drinking alcoholic beverages.
- Staying in a sitting position for a long time.
- Lifting weights – no more than 2.25 kg.
- Doing housework (loading/unloading the washing machine or dishwasher, vacuuming, ironing, mowing the lawn or landscaping).
After discharge, the necessary medications and painkillers are prescribed. Headaches may occur for about two weeks. Some analgesics cause constipation. It is recommended to eat more fruits, vegetables and fiber, and drink more fluids. Alcohol interacts with some medications, so it is important to consult your doctor beforehand.
The wound may be sore for several days after the craniotomy. As healing progresses, itching occurs. There may be swelling in this area. There may be numbness on one side of the wound for several months.
Some patients experience seizures before or after craniotomy. In this case, anticonvulsants are prescribed. If side effects occur, it is important to consult a doctor.
Seek professional help if there are any signs of wound infection or any other unusual symptoms such as severe headache, seizures, vomiting, confusion or chest pain.
Craniotomy - consequences after surgery
Every surgical procedure carries risks. Complications after craniotomy are uncommon. Factors such as the type of brain damage, general health, and age affect how likely you are to develop side effects.
The surgeon will explain potential complications to the patient and give an idea of the risk of their occurrence:
- Seizures.
- Leakage of cerebrospinal fluid (fluid around the brain).
- Deep vein thrombosis.
- Pulmonary embolism.
- Pneumonia.
- Heart attack.
- Damage to the scalp due to the fixation device.
- Facial muscle injuries.
- Sinus damage.
- Cramps.
- Damage to the brain that can cause deterioration or loss of function - deafness, double vision, numbness, paralysis, blindness, loss of smell, memory loss.
- Brain swelling.
- Stroke.
- Allergic reactions to anesthetic.
- Hematomas.
- Bleeding.
- Urinary tract infections.
- Bone flap infection.
Some of these consequences of craniotomy are quite serious and life-threatening. The frequency of their occurrence is 5%.
Questions you can ask a doctor in Assuta:
- How is the operation performed?
- What tests and preparation are needed before surgery?
- What are the risks associated with craniotomy?
- How often is damage to healthy brain tissue seen during this type of surgery?
- What is the expected outcome of a craniotomy?
- What complications may arise?
- How long does it take to recover?
- How many such operations were performed at the clinic last year?
Cranioplasty
This is the name of the operation to restore the tightness of the skull. It is designed to restore the brain’s protection from external influences, normalize blood and lymph flow, eliminate the above symptoms, cosmetic defects and relieve psychological discomfort.
The essence of the procedure is to close the hole in the skull with an implant. A competent neurosurgeon will help you understand the great variety of implants offered by medicine today and choose the best one. Fill out an application on the website or call us to get advice from a leading specialist to choose the right implant and discuss the features of the upcoming operation.
We will tell you what types of cranioplasty implants there are and how the operation to install them is performed.
1. Reasons for the formation of defects in the skull bones
Defects of the skull bones
– a pathology characterized by the absence of a segment of cranial bone tissue. Defects are divided by location area, damage location, and size.
Causes of formation of skull bone defects
Traumatic brain injury may contribute to the occurrence of a cranial defect.
received as a result of an accident, a fall from a height,
a blow to the head, or a gunshot wound
.
Another cause of the defect is resection of a bone segment
as a result of craniotomy.
Iatrogenic intervention (trephination with removal of part of the bone tissue) is a consequence of pathologies such as a tumor, brain abscess and other types of suppuration, post-traumatic or spontaneous hematoma inside the skull.
A must read! Help with treatment and hospitalization!
Implants
There is a list of mandatory qualities that they must have:
- sufficient strength;
- biocompatibility;
- ease;
- plastic;
- do not cause infectious complications;
- do not have a carcinogenic effect.
Implants can be made from the patient's own bone (autografts) or artificial (xenografts).
Autografts
This is bone that has been temporarily removed to access the patient's brain tissue. If the bone needs to be preserved to close a skull defect later, it is placed under the skin of the patient's abdomen or anterior outer thigh. If such preservation is not possible, other techniques using the person’s own bone tissue are used. And if it is impossible to replace the defect with autografts, they resort to materials replacing them.
Xenografts
The so-called “artificial bones” are made of metal (aluminum or titanium), using methyl methacrylate or hydroxyapatite.
Each of the mentioned implants has its own advantages and disadvantages. For example, hydroxyapatite can be used for defects up to 30 square centimeters. This material is completely biocompatible. And it is able to turn into its own bone tissue after 18 months with small defects. And the risk of infectious complications for this type of implant is the lowest among similar ones.
Titanium is the least likely to cause local inflammatory reactions. And from it it is possible to recreate lost fragments of the facial skeleton, the base of the skull, the vault and the walls of the orbit. This is done using simulation and neuronavigation in the preoperative period.
The doctor will help you understand the variety of implants, as well as find out what the latest medical developments in the field of implantology are, during an in-person consultation. Fill out an application on our website and we will make an appointment with a leading specialist in the field of neurosurgery.
In each specific case, it is important to take into account not only the direct benefits for a person, but also the aesthetic and psychological aspects. As well as restrictions imposed on the patient in connection with the choice (for example, a metal implant does not allow the patient to subsequently resort to MRI examination).
3.Reconstruction of the skull bones
In modern medicine, the main method of reconstructing the skull bones is cranioplasty.
. This is a plastic surgery during which the resulting defects in the cranial bone and dura mater of the brain are closed with an artificial implant.
The need for cranioplasty is determined by the presence of the following symptoms and indications:
- post-traumatic epileptic seizures;
- cerebral (speech, motor) disorders;
- cosmetic restoration;
- prevention of re-damage.
The operation is contraindicated
with the development of an intracranial infection, the presence of a foreign body in the brain, or with a serious condition of the patient.
In the course of eliminating defects in the skull bones using cranioplasty with the surgical production of an implant, first of all, the scar of the meninges is dissected with minimal risk of damage to brain tissue. The most effective fusion with bone tissue is achieved by precisely matching the graft to the size and shape of the defect. The implant is placed behind the exposed edges of the lesion and securely fixed to avoid future displacement.
3D computer visualization technology is used to prepare the implant during surgery.
.
Based on a three-dimensional image of the skull, using laser stereolithography
. Then the missing segments and their molds are reconstructed.
Formatted implants are sterilized before use.
About our clinic Chistye Prudy metro station Medintercom page!
Objectives of rehabilitation after brain or spinal cord surgery
After spinal cord surgery, motor activity is often impaired and self-care skills are lost, but depending on the severity of the disorders, the patient can expect full or partial restoration of lost functions. The objectives of rehabilitation are:
- return to basic self-care skills (bathing, washing, eating, dressing, etc.);
- self-relief;
- restoration of motor activity, including independent movement (with the help of assistive devices if necessary);
- gaining psycho-emotional and physical comfort, a stable desire for recovery;
- restoration of lost or acquisition of new professional skills.
Rehabilitation after brain surgery includes:
- activation of the thought process;
- development of lost speech function;
- improved coordination in space;
- eliminating depression and stress;
- improving cognitive skills;
- establishing fine motor skills;
- elimination of convulsions, weakness in the limbs, paralysis;
- normalization of blood pressure;
- prevention of complications in the immune and cardiovascular systems.