On the Gorzdrav website you can order sedatives for adults that effectively combat increased irritability, anxiety, withdrawal symptoms, high blood pressure, disruptions in the functioning of the cardiovascular system, and insomnia.
The tablets for the nervous system presented in the store catalogs are manufactured by global companies. Choose the compositions that suit you and order them online. We will make sure that they are delivered to the pharmacy on time.
Order calming tablets
Gorzdrav is one of the pharmacy chains operating in St. Petersburg and Moscow, as well as the Moscow and Leningrad regions. By cooperating with us, you can forget about the tedious search for the right medicine throughout the city. Just select sedative tablets on the website, register them, indicate which of the Gorzdrav network pharmacies they need to be delivered to. Then pick up the medicine at the selected branch, telling the pharmacist your order number. Payment is made upon receipt, so you do not risk anything.
On our website you can also read instructions for use and reviews from other customers.
What does traditional medicine say?
If you are not allergic to herbs, you can use the following to relieve nervous tension after binge drinking:
- Peppermint. Calms, reduces nausea, normalizes blood pressure, promotes proper functioning of the gastrointestinal tract.
- Melissa. It exhibits mild sedative and hypnotic properties, reduces inflammation, and stimulates digestion.
- Motherwort. A remedy for the treatment of insomnia and high levels of anxiety. It is known for its diuretic properties, thanks to which toxins are more quickly removed from the body of an alcohol addict. It also reduces inflammation and relieves painful spasms.
- St. John's wort. Herbal healer that helps the liver and brain.
To ensure that recovery from heavy drinking is not associated with severe complications, you should not experiment with medications. The only correct solution for alcohol intoxication is to consult a doctor. If a patient is afraid that he will be registered as a drug addict, he should make an appointment with a narcologist in a private clinic.
Use of sedatives
Anti-anxiety medications are a group of medications that regulate the functions of the nervous system. They stimulate inhibition processes or minimize the severity of excitation processes. As a result of their use, aggression goes away, the attack becomes easier and night sleep deepens, and the effect of the analgesics and sleeping pills used is enhanced.[1]
You should use nerve medications if:
- are bothered by frequent headaches;
- sleep is disturbed;
- a person is in a state of severe stress for a long time;
- CNS diseases have been diagnosed;
- Treatment of abstinence in addicted people is carried out.
Medicines for the nervous system made from herbs, plant extracts, and essential oils are usually sold without a prescription. To purchase stronger drugs, you must obtain a doctor's permission.
Tranquilizers (minor antipsychotics)
Tranquilizers are weaker and milder drugs compared to antipsychotics. They are used mainly once or in short (several days) courses, since long-term use can cause addiction (dependence).
Used for aggressiveness caused by overwork, neurotic and depressive disorders, as a rule, with unexpressed aggressiveness.
Basic tranquilizers:
- brodihydrochlorophenylbenzodiazepine;
- diazepam;
- alprozalam;
- Hydroxyzine.
For whom
Modern pharmaceutical companies offer high-quality and safe fast-acting sedatives not only to adults, but also to children. When taking them, you must strictly adhere to the dosage. Otherwise, you may experience unwanted side effects for your health.
On the Gorzdrav website you can order sedatives:
- for men and women;
- for pregnant;
- for children;
- for people who are depressed;
- for those addicted to drugs or alcohol.
Principles and algorithms for the treatment of neuropathic pain
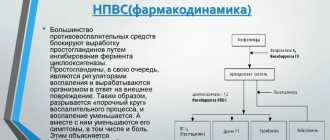
for therapy Neuropathic pain is a pain syndrome caused by damage to the somatosensory nervous system due to a variety of reasons (Table 1). The incidence in the population is 6–7%, and at neurological appointments patients with neuropathic pain account for 10–12%. Clinically, this type of pain is characterized by a complex of specific sensory disorders that can be divided into two groups. On the one hand, these are positive symptoms (spontaneous pain, allodynia, hyperalgesia, dysesthesia, paresthesia), on the other, negative symptoms (hypoesthesia, hypalgesia). This type of pain can be difficult to treat and the pain may not always be completely relieved. Often, such patients have disturbed sleep, develop depression and anxiety, and decrease their quality of life. Many of them suffer for a long time before receiving adequate help. Most patients (about 80%) experience pain for more than a year before their first visit to a specialist. Treatment of the underlying disease (which, of course, is unconditional) does not always lead to pain reduction. We often observe a dissociation between the severity of pain and the degree of damage to the nervous system. Unfortunately, many patients with neuropathic pain mistakenly take NSAIDs, which are ineffective for this type of pain. This is due to the fact that in neuropathic pain the main pathogenetic mechanisms are not the processes of activation of peripheral nociceptors, but neuronal and receptor disorders, peripheral and central sensitization. In the treatment of neuropathic pain, it is best to use an integrated approach. Even within outpatient care, treatment can be initiated with several different methods. Today, there is not enough evidence on the benefits of using conservative non-drug treatment methods (for example, physical therapy, exercise, transcutaneous electrical nerve stimulation). However, given the relative safety of these methods, in the absence of contraindications, the possibility of their use should not be excluded. The most recognized treatment for neuropathic pain today is pharmacotherapy. The main drugs and their characteristics are shown in Table 2. For postherpetic neuralgia, local treatment with lidocaine may first be prescribed. It is believed that the action of lidocaine is based on blocking the movement of sodium ions across the cell membrane of neurons. This stabilizes the cell membrane and prevents the propagation of action potentials and consequently reduces pain. It should be borne in mind that the reduction of pain with local use of painkillers does not extend beyond the area and duration of contact with the affected area of the body. This may be convenient for patients with a small area of pain. Lidocaine 5% in patch or sheet form is indicated for the relief of pain associated with postherpetic neuralgia (PHN). Adverse reactions in the form of burning and erythema can be observed at the site of application with prolonged use. For neuropathic pain of other origin, as well as in case of failure of treatment with lidocaine, it is recommended to begin oral monotherapy with pregabalin or gabapentin, a tricyclic antidepressant or a mixed serotonin-norepinephrine reuptake inhibitor. Of the listed drugs, pregabalin and gabapentin have the best tolerability. These drugs are characterized by an almost complete absence of drug interactions and a low incidence of adverse events. Both drugs have been shown to be effective in treating a variety of neuropathic pain conditions. However, compared to gabapentin, pregabalin, having linear pharmacokinetics and significantly higher bioavailability (90%), has a rapid positive dose-dependent effect: in the studies, a significant reduction in pain of more than 60% of the initial level was achieved within 1-3 days of treatment and persisted for throughout the course of treatment. The speed of pain reduction directly correlates with improved sleep and mood in these patients; a convenient dosing regimen of pregabalin also increases compliance in the treatment of these patients and contributes to a more rapid improvement in quality of life. Pregabalin dosage is from 300 to 600 mg/day. showed to be most effective compared to placebo, significantly reducing pain and sleep disturbances. The drug can be taken before, during or after meals. When treating neuropathic pain, the starting dose may be 150 mg/day. in 2 doses. To obtain ++optimal therapeutic effect, the dose of pregabalin must be increased to 300 mg/day. starting from day 4 of therapy. If necessary, the dose is increased to the maximum (600 mg/day) after a 7-day interval. In accordance with experience with the use of the drug, if it is necessary to stop taking it, it is recommended to gradually reduce the dose over the course of a week. Pregabalin is not metabolized in the liver and does not bind to plasma proteins, so it has virtually no interaction with other drugs. Pregabalin is well tolerated. The most common adverse reactions are dizziness and drowsiness. Tricyclic antidepressants are also effective but cheaper; however, their use is more likely to cause side effects. Moreover, they are relatively contraindicated in cardiovascular disease (an ECG is recommended before prescribing tricyclic antidepressants), orthostatic hypotension, urinary retention and angle-closure glaucoma, and they should also be prescribed with caution in elderly patients. Of the available tricyclic antidepressants in Europe, preference is given to nortriptyline and desipramine, since their use is accompanied by fewer side effects. Newer mixed serotonin-norepinephrine reuptake inhibitors (eg, venlafaxine and duloxetine) are considered to be less effective than tricyclic antidepressants, but at the same time they are better tolerated. It is currently unknown whether failure of one drug predicts failure of another or all subsequent drug therapy. If the first prescribed drug turned out to be ineffective or poorly tolerated by the patient, you should switch to alternative monotherapy with a first-line drug (Fig. 1). If all first-line drugs are ineffective or poorly tolerated, it is recommended to start monotherapy with tramadol or its combination with paracetamol or an opioid analgesic. Unfortunately, this is not always possible, since the prescription of opioid drugs is limited by special requirements for prescribing these drugs. Due to the variety of mechanisms of pain, treatment for each patient must be individualized taking into account the disease that caused the pain, as well as the clinical characteristics of the pain syndrome itself. In addition, many factors should be taken into account, such as: the general condition of the patient, the presence of concomitant diseases (for example, concomitant depression or drug addiction/substance abuse, liver and kidney diseases, etc.), failure/success of previous therapy, and availability medications at a pharmacy or hospital. When developing an individual approach to drug treatment, in addition to the immediate analgesic effect, other positive effects of the chosen drug (for example, reducing anxiety, improving sleep, mood and quality of life), as well as factors such as its tolerability and the possibility of developing serious side effects, must be taken into account . Patients with neuropathic pain require ongoing psychological support. Rational psychotherapy in this case can play a key role. Information about the causes of the disease, actual treatment prognosis and planned therapeutic measures is also extremely important for patients. Treatment of neuropathic pain is a long process that requires regular monitoring of the patient’s health status and compliance with medical prescriptions. At the beginning of therapy, special attention should be paid to the correct titration of the dose of drugs and monitor the possibility of drug interactions. During the treatment process, it is necessary to regularly inquire about how the patient complies with treatment regimens, decide on the need to continue taking the drug, and evaluate its effectiveness. Considering the long-term nature of therapy, the development of long-term adverse events (such as hepato- and gastrotoxicity, changes in the blood system, etc.) that occur while taking certain medications should be monitored and, if possible, prevented. Before starting therapy, an explanatory conversation should be held with the patient and his relatives that the treatment can be long-term, and the reduction in pain will occur gradually. With neuropathic pain, even with the right treatment program, it is rarely possible to achieve 100% pain relief. Thus, the doctor must in a certain way form adequate expectations of the patient and his relatives regarding treatment. In a special study, it was shown that a decrease in pain intensity by 30% from the initial level according to VAS is assessed by the patients themselves as a satisfactory result. This figure should be kept in mind when assessing the effectiveness of the treatment and deciding whether to switch to another drug or add a new drug to the one already taken (rational polypharmacotherapy). Table 3 summarizes the recommendations of the European Federation of Neurological Societies (EFNS) for the treatment of certain conditions associated with neuropathic pain. Experts from this federation analyzed all clinical studies on neuropathic pain registered in the Cochrane Library (a database of evidence-based clinical studies) since 1966. As a result, studies with a high level of evidence were selected, and European recommendations for pharmacotherapy were built on their basis. Rational polypharmacotherapy Pharmacotherapy in the treatment of neuropathic pain is the main method of treatment. However, if monotherapy with first-line drugs does not completely relieve the pain syndrome, then the use of combination pharmacotherapy can increase the effectiveness of treatment with lower dosages of drugs and reduce the risk of side effects. This principle is called rational polypharmacotherapy. Many patients with neuropathic pain are forced to take multiple medications at the same time, despite the lack of evidence-based studies confirming the benefits of such combinations. Recently, information about the effectiveness of various combinations of already known drugs has begun to appear in the literature. In one randomized placebo-controlled trial, the combination of morphine and gabapentin was shown to be superior to either drug alone in terms of analgesic effect. Another study involving 11 patients with neuropathic pain refractory to gabapentin demonstrated the superiority of the combination of gabapentin and venlafaxine over gabapentin alone. Today, there is an obvious need for further research to identify the optimally effective combinations of drugs, select doses and the safest combinations, as well as to evaluate the pharmacoeconomic aspects of therapy. Some aspects of pharmacotherapy Before prescribing any new drug for the treatment of neuropathic pain, a careful analysis of the drugs already taken by the patient is necessary in order to exclude drug interactions. In the case of polypharmacotherapy, preference should be given to drugs that do not have known drug interactions (for example, pregabalin). A potential interaction between opioid analgesics and tricyclic antidepressants has now been described, causing serious adverse events in overdose. If such a combination is used, the benefits and risks of this prescription must be carefully weighed. SSRIs (eg, fluoxetine or paroxetine) and SNRIs (eg, duloxetine) should not be co-administered as they are metabolized by cytochrome P450, which increases the risk of adverse reactions. Most tricyclic antidepressants, anticonvulsants and opioid analgesics have a depressant effect on the central nervous system. To reduce the severity of these and other side effects, gradual titration should be used to achieve an effective dose, starting from the minimum (for example, 1/4 tablet of amitriptyline containing 25 mg) to the maximum tolerated dose over several weeks. In this case, the doctor and patient must understand that pain relief will be gradual. Because tricyclic antidepressants and carbamazepine are rapidly metabolized in some patients, monitoring of drug plasma levels is required before it is safe to further increase the dose if there is no analgesic effect at the lowest dose. Differentiated therapy of pain syndromes Analysis of pain syndrome from the point of view of its pathophysiological mechanisms (nociceptive, neuropathic, mixed) turned out to be very important, primarily from the point of view of treatment. If the doctor assesses the pain as nociceptive, then the best means of treating it are simple analgesics and NSAIDs. If the pain is neuropathic or there is a neuropathic component, then the drugs of choice are anticonvulsants (pregabalin), antidepressants, opioid analgesics and lidocaine, the features of which were discussed above (Fig. 2). In the case of mixed pain syndromes, combination therapy is possible with a choice of drugs depending on the presence of nociceptive and neuropathic components (Fig. 3). Thus, the treatment of neuropathic pain remains challenging at present. The principles and treatment algorithms presented above can help the physician provide the most effective and safe treatment for patients with neuropathic pain syndrome. In the future, the success and prospects of treatment are associated with the development of drugs that affect specific pathophysiological mechanisms of this syndrome.
Literature 1. Danilov A.B., Davydov O.S. Neuropathic pain. Moscow: Borges, 2007. – 198 p. 2. Attal N., Cruccu G., Haanpaa M., Hansson P., Jensen TS, Nurmikko T., Sampaio C., Sindrup S., Wiffen P. EFNS guidelines on pharmacological treatment of neuropathic pain. European Journal of Neurology 2006, 13:1153–1169. 3. Finnerup NB, Otto M., McQuay HJ, Jensen TS, Sindrup SH Algorithm for neuropathic pain treatment: an evidence based proposal. Pain. 2005 Dec 5;118(3):289 –305. 4. Freynhagen R., Strojek K., Griesing T., Whalen E., Balkenohl M. Efficacy of pregabalin in neuropathic pain evaluated in a 12–week, randomized, double–blind, multicentre, placebo–controlled trial of pain– and fixed dose regimens. Pain. 2005 Jun;115(3):254–63. 5. Galer BS, Jensen MP, Ma T., Davies PS, Rowbotham MC The lidocaine patch 5% effectively treats all neuropathic pain qualities: results of a randomized, double–blind, vehicle–controlled, 3–week efficacy study with use of the neuropathic pain scale. Clin J Pain. 2002;18:297–301. 6. Gilron I., Bailey JM, Tu D., Holden RR, Weaver DF, Houlden RL Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005 Mar 31;352(13):1324–34. 7. Goldstein DJ, Lu Y., Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116:109–118. 8. Harati Y., Gooch C., Swenson M. et al. Double–blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy. Neurology. 1998;50:1842–1846. 9. Saarto T., Wiffen P. Antidepressants for neuropathic pain. Cochrane Database of Systemic Reviews 2005; 20:CD005454. 10. Sabatowski R., Ga'levz R., Cherry DA et al. Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: Results of a randomized, placebo-controlled clinical trial. Pain 2004. 11. Siddall PJ, Cousins MJ, Otte A., Griesing T., Chambers R., Murphy TK Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo–controlled trial. Neurology. 2006 Nov 28;67(10):1792–800. 12. Sindrup SH, Otto M, Finnerup NB et al. Antidepressants in the treatment of neuropathic pain. Basic and Clinical Pharmacology and Therapy 2005; 9 6: 399 –409. 13. van Seventer R., Feister HA, Young JP Jr, Stoker M., Versavel M., Rigaudy L. Efficacy and tolerance of twice–daily pregabalin for treating pain and related sleep interference in postherpetic neuralgia: a 13–week, randomized trial.Curr Med Res Opin. 2006 Feb;22(2):375–84. 14. Wiffen P., McQuay H., Edwards J. et al. Gabapentin for acute and chronic pain. Cochrane Database Systematic Reviews 2005a; 20: CD005452. 15. Wiffen P., Collins S., McQuay H. et al. Anticonvulsant drugs for acute and chronic pain. Cochrane Database Systematic Reviews 2005c; 20:CD001133.