Translation of the presentation “Anomalies and normal variants of the intracranial arteries: proposed workflow for classification and significance.”
| Congress: | ECR 2016 |
| Poster No.: | C-0199 |
| Authors: | A. Hakim1, J. Gralla1, C. Rozeik2, P. Mordasini1, F. Pult1, L. Leidolt1, E. Piechowiak1, K. Hsieh1, M. El-Koussy1; 1Bern/CH, 2Loerrach/DE |
| DOI: | 10.1594/ecr2016/C-0199 |
| DOI-Link: | https://dx.doi.org/10.1594/ecr2016/C-0199 |
Translation into Russian: Simanov V.A.
1.1. Variants of origin (discharge) of vessels
1.1.1. Common origin : two different vessels can have the same origin (discharge)
SCA/PCA: 2-22% Fig.3 :
The common trunk arises from the basilar artery, then branches into the posterior cerebral artery (PCA) and the superior cerebellar artery (SCA) [1].
PICA / AICA: common option Fig. 4 :
The anterior inferior cerebellar artery (AICA) shares a common trunk with the posterior inferior cerebellar artery (PICA) [2].
1.1.2. Funnel: 7-15% Fig.5 :
It is a funnel-shaped dilatation of the vessel at the origin. Its diameter should be no more than 3mm. It is most common at the origin of the posterior communicating artery (Pcom). A similar variant has also been described in the anterior communicating artery (Acom), ophthalmic artery and anterior choroidal artery [2].
1.1.3. Abnormal origin (discharge) due to persistent fetal circulation:
Fetal type PCA:
The posterior communicating arteries are the terminal branches of the basilar artery. During development, RCAs originate from the internal carotid artery (ICA). This variant, if it persists into the postnatal period, is called “fetal origin.” This option can be classified into two subtypes: Fig. 6
- Complete fetal PCA: 4-26% unilateral, bilateral 2-4%. PCA is entirely derived from the ICA. The P1 segment is absent, i.e., only the ICA supplies the occipital lobes [3]. In bilateral complete fetal type PCA, the basilar artery may be hypoplastic Fig. 7 .
- Partial fetal PCA: 11-29% unilateral, 1-9% bilateral. The P1 segment is still present, but is smaller or equal in diameter to Pcom, i.e. Most of the blood supply to the occipital lobes comes from the ICA[3].
Persistent dorsal ophthalmic artery (PDOA): 1.1% Fig.8, Fig.46 :
During embryonic development, the orbit is supplied with blood through the anterior and posterior rami, which originate from the ICA. Typically, the posterior branch is obliterated, while the anterior branch continues to supply the orbit. However, with this option the opposite happens. The PDOA enters the orbit through the superior orbital fissure [4].
The ophthalmic artery can also arise from other parts of the ICA, including the cavernous segment, in 8% of the population [2] Fig. 9 .
MMA from the orbital artery: 16% Fig. 10 :
During embryogenesis, the middle meningeal artery (MMA) arises from the stapedial artery. The stapedial artery gives off branches to the ECA. One of these branches is the supraorbital artery, which forms an anastomosis with the developing ophthalmic artery. Along this anastomosis, failure of segmental regression or persistence of segments that should regress leads to a number of anomalies, such as the origin of the MMA from the ophthalmic artery [2]. In this case, the foramen spinosum will be absent.
Fig. 3 TOF MRA, common trunk of PCA and SCA (red arrow) and ipsilateral dominant vertebral artery (white arrow)
Fig. 4 3D TOF MRA of the AICA (white arrow) extending caudally, supplying the PICA territory. Note the absence of PICA ipsilaterally. The contralateral PICA is present (green arrow).
Fig. 5 3D TOF MRA, funnel-shaped expansion (funnel) at the origin of Pcom (arrow).
Fig. 6 3D TOF MRA, complete fetal PCA (white arrow) with P1 segment absence on one side and partial fetal PCA (red arrow) with P1 segment hypoplasia (green arrow) on the other side. Note fenestration of the proximal part of the P1 segment (blue arrow).
Fig. 7 3D TOF, complete fetal PCAs on both sides and hypoplastic basilar artery
Fig. 8 Persistent dorsal ophthalmic artery: MIP (a) and 3D TOF MRA (b) show the ophthalmic artery arising from the posterior surface of the ICA (arrow in a ) and marked in red ( b ).
Fig. 9 Cavernous origin of the ophthalmic artery: MIP TOF lateral view (a), 3D TOF MRA ventral view (b), and 3D rotational DSA lateral view (c) showing the ophthalmic artery (white arrow) arising from the lateral surface of the cavernous segment of the ICA . Note the incidentally discovered Pcom aneurysm (red arrow).
Fig. 10 DSA (a) showing the MMA (red arrow) arising from the ophthalmic artery (white arrow). MIP reconstruction in the CT bone window (b), showing the absence of the foramen spinosum on the left side. Foramen spinosum on the right side is marked for comparison (blue arrow).
Medical Internet conferences
O.A. Fomkin - Saratov State Medical University named after. IN AND. Razumovsky Ministry of Health of Russia, assistant at the Department of Human Anatomy, Candidate of Medical Sciences; V.N. Nikolenko - State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after. THEM. Sechenov Ministry of Health of Russia, Vice-Rector for Scientific and Innovation Activities, Professor of the Department of Human Anatomy, Director of the Research Institute of Molecular Medicine, Professor, Doctor of Medical Sciences; Yu.A. Gladilin – State Budgetary Educational Institution of Higher Professional Education Saratov State University named after. IN AND. Razumovsky Ministry of Health of Russia, Associate Professor of the Department of Human Anatomy, Doctor of Medical Sciences.
Introduction. Variability as a general biological phenomenon does not lose its relevance and deserves the attention of many scientists [1, 2]. Variability shows the plasticity of living systems and is associated with the implementation of the adaptive strategy of a natural population. The study of variability makes it possible to judge the interaction of the genotype with environmental factors during ontogenesis [3].
In response to the demands of clinical medicine, at present, detailed information is required not so much on the typical structure or average anatomical norm of an organ, but on the entire spectrum of its individual, typical and combined variability [2]. This also applies to the arterial vessels of the brain.
The subject of this study is the posterior communicating artery (PCA). As a branch of the cerebral part of the internal carotid artery, it participates in the formation of the arterial (Circle of Willis) circle of the brain. It has been proven that blood through this artery can flow in both directions [4]. In this regard, the PCA plays an important role in the implementation of compensatory collateral blood flow between the systems of the internal carotid and vertebral arteries.
The structure of the posterior communicating arteries varies greatly. Compared to other cerebral arteries, they have a small diameter and almost a pinpoint lumen [5-7].
Purpose of the study: to determine the variants of the posterior communicating artery (PCA) of adults depending on the individual and combined variability of its morphometric parameters.
Materials and methods . The study material was PCA obtained from autopsies of 115 corpses of people aged 21 to 84 years who died for reasons not related to acute or chronic cerebrovascular pathology. A total of 230 artery samples were examined. To study the morphology of the artery, transverse millimeter sections were made using a razor. Then the sections were placed in a Petri dish with saline solution and the outer diameter and wall thickness of the artery were measured under a microscope with an accuracy of 0.01 mm. The diameter of the artery lumen is presented in the study as the difference between the outer diameter and twice the thickness of the artery wall.
The obtained data were processed by the variation-statistical method using the Statistica-6 application package and Microsoft Exsel Windows-XP. To check the presence of a normal distribution, the Kolmogorov-Smirnov test was used. The distribution of parameters in the studied sample did not differ from normal. In this regard, for all parameters, the minimum and maximum values, the arithmetic mean (M), the error of the arithmetic mean (m), the standard deviation (s), and the coefficient of variation (Cv) were determined. To assess the reliability of differences between series, a parametric test (Student's test) was used. In this case, the differences were considered significant at a 95% probability threshold (p < 0.05). When studying individual variability, like most researchers dealing with the range of anatomical norms, we took the variation interval M ± σ as the average value of a trait. Since statistically significant gender differences in the length, wall thickness and lumen diameter of the PCA were found [6], variations in these parameters were calculated separately for men and women.
Results. The average values of the morphometric parameters of the PCA (230 samples), excluding gender, age and cerebral hemisphere, were: 1) length 12.26±0.19 mm (A=5.30-20.10 mm; s=2.89 mm; Сv=23.6%); 2) outer diameter – 1.33±0.02 mm (A=0.80-2.10 mm; s=0.26 mm; Cv=19.2%); 3) wall thickness – 0.23±0.01 mm (A=0.12-0.40 mm; s=0.06 mm; Cv=26.2%); 4) lumen diameter – 0.88±0.02 mm (A=0.46-1.46 mm; s=0.25 mm; Cv=28.0%).
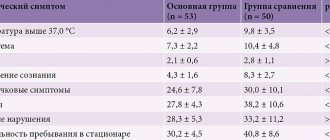
Significant variability in the morphometric parameters of the PCA made it possible to identify groups of variants of their values (Table 1).
According to the length of the PCA, they were divided into: short - length less than 9.89 mm in men and less than 8.80 mm in women; medium in length - with a length from 9.90 to 15.72 mm for men and from 8.81 to 11.51 for women; long – with a length of more than 15.73 mm in men and more than 11.52 mm in women. The average age of subjects with short PCAs was 1.2 times greater than that of people with long arteries – 51.3±2.9 years and 43.0±2.6 years, respectively (p=0.039). The quantitative ratio of men and women in the group of subjects with short arteries is 39.5 and 60.5%; in the group of subjects with long arteries – 71.9 and 28.1%.
Based on the size of the outer diameter, SSAs are: thin - diameter less than 1.06 mm; medium diameter (medium wide) - the diameter ranges from 1.07 to 1.59 mm and wide - with a diameter of more than 1.60 mm. Subjects with wide PCA were on average 1.2 times older than people with thin arteries - 55.0±3.0 years and 45.5±2.1 years, respectively (p=0.011). The quantitative ratio of men and women in the group of subjects with thin arteries is 59.0 and 41.0%; in the group of subjects with wide arteries, the representation of men and women is equal – 50% each.
Based on the wall thickness, the PCA was divided into: thin-walled - wall thickness less than 0.17 mm in men and less than 0.14 mm in women; medium in thickness - with a wall thickness from 0.18 to 0.30 mm for men and from 0.15 to 0.25 mm for women; thick-walled - with a wall thickness of more than 0.31 mm in men and more than 0.26 mm in women. The average age of subjects with thick-walled PCAs was 1.7 times greater than that of people with thin-walled arteries - 69.2±2.3 years and 40.7±2.5 years, respectively (p=1·10-6). The quantitative ratio of men and women in the group of subjects with thin-walled arteries was 25.7 and 74.3%; in the group of those studied with thick-walled arteries – 78.9 and 21.1%.
Depending on the size of the lumen diameter, we have identified PSA: with a narrow lumen - the lumen diameter is less than 0.58 mm in men and less than 0.68 mm in women; with an average lumen - the diameter of the lumen varies from 0.59 to 1.07 mm in men and from 0.69 to 1.19 mm in women; with a wide lumen - the lumen diameter exceeds 1.08 mm in men and 1.20 mm in women. The age of subjects with a narrow and wide lumen of the PCA did not differ significantly - 51.2 ± 2.5 years and 45.6 ± 3.1 years, respectively (p = 0.163). The quantitative ratio of men and women in the group of subjects with a narrow lumen of the PCA was 75.6 and 24.4%; in the group of those studied with a wide lumen of the PCA – 43.6% and 56.4%.
It was noted that approximately 71.9% of all thin ACAs had a narrow lumen, and 28.2% had an average lumen. At the same time, thin PCAs had thin wall thickness in 23.1% of cases, thick wall thickness in 5.2% of cases, and medium wall thickness in 71.8% of cases (Table 2).
Medium-wide arteries in 87.1% of cases were characterized by an average lumen diameter; in 7.7% of cases, such PCAs had a narrow, and in 5.2%, a wide lumen diameter. Medium-wide arteries, as a rule, had an average wall thickness (67.1% of observations); thin- and thick-walled PCA were also found in this group – in 12.9 and 20% of cases, respectively.
Wide PCAs had a wide lumen diameter in 86.1% of cases and an average lumen diameter in 13.9% of cases. Moreover, in 13.9% of cases they were thin- or thick-walled, and in the remaining 72.2% they were characterized by an average wall thickness.
The combined variability of the morphometric parameters of the PCA made it possible to identify 18 of its types. The most common are medium-wide ACAs with an average wall thickness and an average lumen (43.0%). Rare types (frequency of occurrence less than 1%) include thin PCA (with an average wall thickness and lumen diameter, with a thin wall and a narrow lumen, a thick wall and a narrow lumen, a thick wall and an average lumen); ASA with a medium outer diameter, a thick wall and a wide lumen; wide PCA with a thick wall and medium lumen (Fig. 1). Thin-walled SSAs based on our material never had a wide lumen diameter.
Rice. 1.Frequency of occurrence of types of PSA,% ( OD – outer diameter , TS – wall thickness, DP – lumen diameter ): 1 – average for ND, TS and DP; 2 – thin with medium TS and narrow DP; 3 – wide with medium TC and wide DP; 4 – average in ND, with a thick wall and average DP; 5 – average according to ND with a thin wall and average DP; 6 – thin with a thin wall and medium DP; 7 – average according to ND with a thick wall and narrow DP; 8 – average according to ND, with a thin wall and wide DP; 9 – average for ND, vehicles with narrow DP; 10 – wide with a thin wall and wide DP; 11 – wide with average wall thickness and average DP; 12 – wide with a thick wall and wide opening; 13 – thin with medium TC and medium clearance; 14 – average in ND, with a thick wall and wide DP; 15 – thin with a thin wall and narrow DP; 16 – thin with a thick wall and narrow DP; 17 – thin with a thick wall and medium DP; 18 – wide with a thick wall and medium DP.
Discussion. The vast majority of works concerning PCA are devoted to variants of its development: aplasia, hypoplasia, the presence of a vascular network at the site of the artery, etc. [5, 8, 9]. We presented information on the individual typological variability of the morphometric parameters of the PCA for the first time.
As a result of the study, it was revealed that the morphological parameters of the PCA (length, outer and inner diameter, wall thickness) are characterized by significant individual variability. The coefficient of variation of the studied parameters varies from 19.2% (outer diameter) to 28.0% (lumen diameter). For each of the parameters, we have identified 3 groups of arteries: I – with a value of the attribute less than average (<М-σ); II – with the average value of the trait (M±σ); III – with a trait value greater than average (>M+σ). No clear pattern was found in the predominance of men or women in the extreme groups of variability (groups I and II). Thus, among subjects with short, thin-walled arteries and arteries with a wide lumen, women predominate, and among subjects with long, thin, thick-walled arteries and arteries with a narrow lumen, men predominate. In the group of those studied with wide ACAs, the percentage representation of men and women is the same.
The average age of subjects whose PMA, based on the size of their outer diameter, wall thickness and lumen diameter, belongs to group III, is statistically significantly 1.2-1.7 times greater than that of people with PMA belonging to group I variability. The average age of men and women with short PCA (group I), on the contrary, is 1.2 times greater than that of people with long PCA (group III). The age of subjects with narrow or wide lumen PCA did not differ significantly.
Conclusion. Thus, the analysis of individual variability in the length, outer and inner diameters and wall thickness of the PCA made it possible to identify 3 groups of artery variants for each of the parameters: with an average value of the attribute, with a value of the attribute less and more than the average. The combined variability of the morphometric parameters of the PCA made it possible to identify 18 of its types.
The data obtained will complement and organize the existing information on the dimensional characteristics of the PCA, which is important for a better understanding of the area of neuromorphology under study, and can also be useful in modeling blood flow in the arterial circle of the brain.
1.2. Change in the number of vessels
1.2.1. Reducing the number of vessels
ICA agenesis: 0.01% Fig.11 , Fig.47 :
Around day 24 of embryogenesis, the ICA develops from the dorsal aorta and third arch. Subsequently, at approximately the 5th - 6th week, the base of the skull begins to take its shape. Thus, absence of ICA will result in absence of the carotid canal, identification of which is the most practical method in identifying this anomaly in a clinical setting. Typically, patients with ICA agenesis are asymptomatic due to well-developed collateral circulation through the ECA and vertebrobasilar system [2].
Aplasia of the A1 segment: 1-2%. Fig.12 and Fig.15 :
In this situation, both A2 segments are supplied by the existing A1 segment [2].
Azygos ACA: less than 1% Fig. 13 :
Both A1 segments form a common A2 segment, which supplies blood to both hemispheres[2].
Lack of Acom: 5% Fig.14 [2]:
Typically, the absence of the anterior communicating artery (Acom) is not easy to detect on time-of-flight MR angiography because the artery may be present but the flow signal is too weak to be visualized.
Lack of Pcom: 0.6% Fig.15 :
The posterior communicating artery (Pcom) is usually smaller than the P1 segment. Complete absence is rare [2].
Artery of Percheron: 4-11.5% Fig. 16 :
The thalamo-mesencephalic arterial supply can be divided into 3 types: type 1 is the most common, with perforating arteries on both sides arising from the P1 segments; type 2 , known as the artery of Percheron, arising from one of the P1 segments, supplying both sides; type 3 is an arch that connects both P1 segments and from which the perforating arteries arise [5].
1.2.2. Increase in the number of vessels
Incremental MCA: 2.7% Fig. 17 :
Literary definitions of accessory middle cerebral artery (MCA) and MCA duplication are quite dichotomous. In this paper, we use the definition of Teal et al., who limited the term “accessory MCA” to the branch arising from the anterior cerebral artery (ACA) and the term “duplicate MCA” to the artery arising from the distal segment of the ICA [6]. To distinguish an accessory MCA from a duplex one, the dominant vessel must be identified by carefully searching for the MCA bifurcation. Comparison with the contralateral side is also useful to find the level of ICA bifurcation [1].
Duplication: refers to two separate arteries that do not exhibit distal fusion. For example:
- MCA duplication: 0.2-2.9% Fig. 18 : MCA duplication is an artery that arises from the ICA and runs parallel to the main trunk of the MCA. This variant should not be confused with early branching of the MCA, in which a short single M1 segment is present. It should also not be confused with the anterior temporal branch, which often arises from the M1 segment.
- Acom doubling: 18% Fig. 19 [1].
- SCA doubling: 14% Fig. 12 [2].
Trifurcation:
- ACA trifurcation: 2-13% Fig. 20 : trifurcation refers to the presence of three A2 segments and is described by various names such as pericallosal triplex, arteria mediana corporis callosi and persistent primitive median artery of the corpus callosum [2]. Early origin of a frontopolar branch, for example from Acom, may appear as a third A2 segment.
MCA trifurcation: 12% Fig. 21 : The horizontal segment of the MCA is divided into superior and inferior trunks in approximately 78%. In 12% there is an additional (middle) trunk, this situation is called trifurcation, and the presence of more than 3 trunks, for example, quadrifurcation, is observed in approximately 10% Fig. 22 [2].
Fig. 11 Agenesis of the left ICA. TOF MRA (a), no signal from the flow in the left ICA. MIP CTA (c), CCA continues as ECA with no ICA. Bone window CT (b), absence of bony carotid canal on the left side. The normal carotid duct on the right side is marked with a red arrow for comparison.
Fig. 12 3D MRA, absence of A1 segment of ACA, both A2 segments extend from the contralateral side. Note the partial fetal PCA (white arrow), duplication of the superior cerebellar artery (blue arrow), and hypoplastic vertebral artery (red arrow) that terminates as the PICA.
Fig. 13 3D MRA, fusion of both A1 segments to form a single A2 segment (azygos ACA) (arrow).
Fig.14 3D TOF MRA, no Acom.
Fig. 15 3D TOF, absence of Pcom and A1 segment on one side. The significance of this option is that if the ICA is occluded on that side, there will be no possibility of collateralization through the circle of Willis. Incidental finding: aneurysm of the terminal portion of the contralateral ICA (arrow).
Fig. 16 MIP (a) and 3D TOF (b), type 2 thalamo-mesencephalic arterial supply (artery of Percheron) with a single arterial trunk (arrow) arising from the P1 segment, the branches of which supply blood to both sides.
Fig. 17 3D TOF, additional MCA (arrow) extending from the A1 segment.
Fig. 18 3D TOF of a duplicated MCA (red arrow) extending from the distal ICA. This artery should not be confused with the anterior temporal branch (white arrow), which is a common finding.
Fig. 19 3D TOF, Acom duplication (white arrows), proximal A2 segment fenestration (red arrow), A1 segment aplasia and complete fetal PCA (blue arrow).
Fig. 20 3D TOF, ACA trifurcation with three A2 segments (arrows), the third branch arises from Acom
Fig.21 3D TOF, MCA trifurcation with additional middle trunk.
Fig.22 3D TOF, MCA quadrifurcation.
1.3. Change in morphology
1.3.1. Hypoplasia
ICA hypoplasia: 0.079% Fig. 23 :
In contrast to agenesis, the thin vessel is identifiable. Again, skull base tomography is useful in visualizing the bony carotid canal, which is thinner than normal in hypoplasia [2].
Hypoplasia A1: 10% Fig.24 :
Asymmetry of A1 segments is observed in 80% of cases. Hypoplasia is defined when the vessel diameter is less than 1.5 mm [2].
Hypoplasia A2 (bihemispheric ACA): 7% Fig. 24 :
One of the A2 segments is hypoplastic. In this variant, the blood supply to the ipsilateral hemisphere occurs mainly from the contralateral (dominant) A2 segment [2].
Hypoplasia Pcom: 34% Fig.25 :
but complete absence is a rare finding [2].
Hypoplasia of the vertebral artery:
50% on the right side (left dominant), 25% on the left side (right dominant), 25% codominant. In approximately 0.2%, the vertebral artery ends in the PICA Fig. 12 and Fig. 26 [7] [2]
1.3.2. Hyperplasia
Hyperplasia of the anterior choroidal artery: 2.3% Fig. 27 :
The anterior choriodal artery arises from the posterior surface of the terminal segment of the ICA, distal to the origin of the Pcom. This is usually a small branch. If it is enlarged (hyperplastic), then it supplies blood to part of the territory of the posterior cerebral artery (occipitotemporal branch) [1, 2].
1.3.3. Early bifurcation (early division):
Early MCA bifurcation: This is a common finding Fig.28 :
The horizontal segment of the MCA is usually 12 mm long, but may be shorter, with early branching (bi- or trifurcation) [1].
1.3.4. Fenestration: 0.7% including all intracranial vessels Fig. 6 , Fig. 19 and Fig. 29 . Fenestration is the division of the lumen of an artery into two separate channels. Each canal has its own endothelium and muscle layer and can separate the adventitia. These two canals merge distally. Fenestration is most often observed in the posterior circulation [1, 2].
- Fenestration A1: 0-4% [1]
- Fenestration A2: 2% Fig. 19 [1]
- Acom fenestration: 12-21% [1]
- Fenestration of the vertebral artery Fig. 29 : 0.3-2% [1].
Fenestration of the basilar artery Fig. 29 : 0.12-1.33%: the basilar artery is formed by the fusion of two longitudinal neural arteries. Incomplete fusion results in segmental fenestration, which is usually present in the proximal segment of the basilar artery [2].
Fig. 23 CTA (a), hypoplastic ICA (arrows). CT bone window (b) asymmetrical bony carotid canal
Fig. 24 3D TOF, hypoplasia of the A2 segment (white arrow) and the contralateral dominant A2 segment “bihemispheric ACA”. Note hypoplasia of the A1 segment (red arrow).
Fig. 25 MIP CTA, right Pcom hypoplasia (arrow). Note the pathological occlusion of the contralateral ICA.
Fig. 26 3D TOF, hypoplasia of the vertebral artery (white arrow) that ends as a PICA (green arrow).
Fig. 27 3D TOF, hyperplasia of the anterior choroidal artery (white arrow). The contralateral anterior choroidal artery is of normal caliber (green arrow). Red arrow points to fetal PCA, blue arrow to Pcom.
Fig. 28 3D MRA, early bifurcation with short prebifurcation segment M1 (arrow).
Fig. 29 Fenestration of the A1 segment (a), Acom (b), M1 segment (c), V4 segment (d) and the proximal part of the basilar artery (e).
Symptoms
As mentioned earlier, in the early stages, signs of hypoplasia may be completely absent.
The development of the pathological process can last for years and only when the arterial lumen narrows to a certain value will some symptoms appear. The paradox is that in the complete absence of manifestations of pathology in the early stages, the entry of the disease into the so-called active phase is accompanied by a rich clinical picture. However, in each patient with narrowing of the vertebral artery (right or left), symptoms manifest themselves completely differently:
- Headaches of different nature and specificity. Painful sensations can be periodic or constant, intensify after intense physical activity or occur at rest. With hypoplasia of the cerebral artery, the pain also differs in intensity, from strong, which has to be relieved with analgesics, to weak, which many tolerate without medication. As for the specifics, in most cases we are talking about dull and aching pain, however, they can also be sharp, stabbing.
- Unreasonable dizziness indicates cerebral circulatory disorders. This clinical sign is the second most common and also varies in nature. In some cases, dizziness is not associated with physical exertion, emotional state and other factors; they simply occur more frequently and disappear as quickly as they appeared. In other cases, dizziness begins after a change in body position, any load, stress, etc.
- Often hypoplasia of the right vertebral artery is accompanied by emotional disturbances. A person experiences frequent and sudden changes in mood, depression, which can last up to 2-3 days, then disappear without a trace, constant lethargy, states of apathy and even depressive states.
- If we talk about hypoplasia of the left vertebral artery, this form of the pathological process is more often characterized by changes in blood pressure. Yes, with right-sided hypoplasia they are also present in the clinical picture, but in this case they are noted more often.
- The pathology affects the patient’s body with a state of drowsiness, fatigue, and a feeling of weakness. People with hypoplasia do not get enough sleep even with a full, sound eight-hour sleep, are in a lethargic state, and often yawn.
- The pathology may be accompanied by disorders affecting the vestibular apparatus. In this case, dizziness is also present among the clinical signs, but they become more intense, and are accompanied by nausea, excessive sweating, and changes in skin color (pallor or, conversely, redness of the face). The clearest signs of damage to the vestibular apparatus and the progression of this pathology will be impaired coordination. A loss of balance appears, the gait becomes uncertain, the person sways from side to side, all movements become unclear, and loss of space may develop.
Over time, the symptoms worsen; severe forms of vertebral artery hypoplasia are accompanied by damage to the nervous system. On the one hand, this is expressed in numbness of certain parts of the body (usually limbs), on the other, visual hallucinations. In some cases, partial paralysis even occurs.
1.4. Changing the course
1.4.1. Aberrant lateral pharyngeal ICA, tortuous ICA, and kissing carotid arteries:
During embryonic development, the ICA is thought to begin to unwind as the dorsal aortic root descends into the thorax, providing a direct pathway for the ICA. Failure in unwinding results in tortuosity of the ICA, which runs close to the midline of the posterior pharyngeal wall, called the aberrant lateral pharyngeal artery [6].
This morphology is more commonly seen in older patients or those with hypertension, but should not be confused with the fetal variant, although both have the same meaning (see below). The incidence of aberrant lateral pharyngeal ICA is approximately 5%, but the exact prevalence of the anomaly is unknown as it cannot be differentiated morphologically from tortuosity. Studies conducted by Ekici et al. showed that the least affected age group with ICA tortuosity was the younger age group [8].
The term "kissing carotid arteries" describes the elongated carotid arteries that meet at the midline; can be observed retropharyngeal or intrasphenoidal / intrasellar Fig. 30 [2].
1.4.2. Persistent primitive olfactory artery: 0,14%
The ACA is derived from the primitive olfactory artery, which regresses to form the recurrent artery of Heubner. Violation of regression leads to preservation of the primitive olfactory artery. This artery has an extreme anterior-inferior course in the A1 segment, which moves along the olfactory tract before the posterosuperior transition to the A2 segment, forming a hairpin-shaped configuration [9].
1.4.3. Persistent embryological anastomosis
+ persistent carotid-vertebrobasilar anastomosis:
During embryonic development, the anterior circulation supplies the hindbrain through several anastomoses, since the posterior circulation is not yet sufficiently developed. After the development of the vertebral arteries, these anastomoses regress. Impaired regression results in abnormal communication between the anterior and posterior circulation in the postnatal period. The most common form of these anastomoses is the fetal type PCA (see variants of origin/origin of vessels). Recognizing the course of these abnormal vessels, as well as the level of entry into the skull, is critical for their differentiation Table 1
- persistent trigeminal artery (PTA): 0.1-0.2% Fig. 31 Fig. 48 : PTA originates from the cavernous segment of the ICA and communicates with the basilar artery. Proximal to the level of the anastomosis, the basilar artery is usually hypoplastic. On the angiogram, when viewed from the side, it has a characteristic “Trident of Neptune” or Tau sign configuration, reminiscent of the Greek letter “Tau” [1] [2]. There are two different classifications Table 2 Fig. 32 and Fig. 33 [10].
- PTA variants (Saltzman III): 0.18-0.76%: Arteries that supply the posterior fossa, arising from the precavernous segment of the ICA and not communicating with the basilar artery [1].
- Persistent auricular artery (otic artery): the rarest carotid-vertebrobasilar anastomosis. The existence of the auricular artery is controversial because it has not been identified in lower animals. It passes from the petrosal segment of the ICA to the basilar system through the internal auditory canal [2].
- Persistent primitive hypoglossal artery (PPHA): 0.03-0.26% Fig. 34 Fig. 49 : This artery runs from the cervical segment of the ICA to the basilar artery through the hypoglossal canal. The vertebral artery is hypoplastic. CT scan of the skull base shows an enlarged bony hypoglossal canal [1, 2].
- Proatlantal intersegmental artery: very rare. Connects the cervical segment of the ICA or external carotid artery (ECA) to the vertebrobasilar system. The artery enters the base of the skull through the foramen magnum, which allows it to be differentiated from the hypoglossal artery. There are two types:
- Type I: joins the vertebral artery above the atlas.
- Type II: enters the vertebral artery through the atlas [1, 2].
+ persistent internal-external carotid anastomosis
- Aberrant intratympanic ICA: very rare. This variant is an anastomosis between the ICA and the ECA, as it is believed to arise from agenesis of the cervical segment of the ICA and the development of an anastomosis between the horizontal (petrosal) segment of the ICA and the enlarged inferior tympanic artery, which is a branch of the ECA. The ICA (or rather the enlarged inferior tympanic artery) in this case has a smaller diameter than the usual ICA, with the absence of the ascending part of the carotid canal as it enters the base of the skull, posterior and parallel to the jugular bulb, which resembles a mass in the hypotympanum; there is also no bone plate between the carotid canal and the tympanic cavity [1].
- Persistent stapedial artery: 0.48%. This anomaly occurs due to the persistence of the anastomosis through the stapedial artery, which is usually present during development between the ECA and ICA. The artery arises from the petrosal segment of the ICA, passes through the obturator foramen, and ends as the MCA in the epidural space of the middle cranial fossa. A CT scan of the skull base may show a small canal near the carotid canal. Foramen spinosum, which contains MMA, will be absent. a persistent stapedial artery may be associated with an aberrant ICA [1, 2].
Table 3 shows the frequency of variants discussed, however, there are other rare variants that cannot be included in a single document. Finally, having a fully developed Circle of Willis can be considered an option since it is present in less than 50% of the population [2]
*NB: Frequency varies between authors depending on the type of study performed (CT, MRI, surgical or post-mortem). Frequency may also vary depending on geographic distribution; Published data may not always be applicable to other populations.
Table 1: Types of persistent carotid-vertebrobasilar anastomoses
Table 3: occurrence of anatomical variants
Fig. 30 Coronal MIP CTA of a patient with a history of hypertension shows elongated carotid arteries reaching the midline (“kissing” carotid arteries).
Fig. 31 3D TOF, lateral view (a) and dorsal view (b), persistent primitive trigeminal artery (red arrow) arising from the cavernous segment of the ICA and communicating with the basilar artery, which is hypoplastic to the level of the anastomosis (white arrow). In lateral view, the anomalous artery with ICA resembles Neptune's trident and the Greek letter "tau".
Fig. 32 MIP CTA of persistent primitive trigeminal artery (red arrow) in two different cases. According to Salas there are 2 types: medial sphenoidal or intrasellar (a), which extends into the sella turcica and perforates the dura mater or dorsum sella (green arrow), as in this case, and lateral petrosal or parasellar (b), in which the vessel goes with the sensory roots of the trigeminal nerve, on the side of the sella turcica.
Fig. 33 3D TOF showing two different cases of persistent primitive trigeminal artery (red arrow). Classification according to Saltzman: Type I (a), in which the PCA supplies the superior part of the basilar artery, including the posterior territory, and type II (b) with the fetal PCA (white arrow).
Fig. 34 3D CE MRA oblique (a) and posterior (b) views showing the persistent primitive hypoglossal artery (red arrow) which arises from the cervical segment of the ICA (green arrow) and continues as the vertebrobasilar artery (blue arrow). ECA is marked with a white arrow.
Causes
Hypoplasia, that is, an anomaly in the development of tissues or an organ, which in this case concerns the vertebral arteries, as mentioned earlier, is a congenital pathology. This means that the main reason for underdevelopment of the artery is problems in the embryonic stages. At the same time, a number of factors can be identified that contribute to the fact that hypoplasia of the vertebral artery occurs in a newborn and manifests itself at a certain age:
- Infectious diseases transmitted by the mother during pregnancy.
- Exposure of the fetus to radiation or ionizing exposure.
- Mechanical injuries, including blows, bruises and other injuries to the abdominal cavity during pregnancy.
- Narrowing of the artery in a newborn can be caused by a genetic predisposition, for example, if the family history includes pathologies of a vascular nature.
- Toxic factor - if during pregnancy a woman smoked, abused alcohol, worked at a chemical plant, or took any potent drugs for a long time, there is a high probability that hypoplasia may be associated with each of these factors.
Meaning
The list in Fig. 35 shows the values of the anatomical options.
2.1. Recognition of anatomical patterns and the ability to distinguish them from pathological changes:
2.1.1. Knowledge of normal variations is part of the anatomical knowledge that is important for every radiologist and surgeon. Knowledge of normal variants and their proximity to other structures facilitates the understanding and diagnosis of various diseases, such as:
- Trigeminal neuralgia, which can be caused by the presence of a variant of PTA (less commonly PTA), due to the proximity of the vessel to the trigeminal nerve [11].
- Glossopharyngeal neuralgia or hypoglossal nerve palsy, which can be caused by a persistent hypoglossal artery [1].
- Pulsatile tinnitus in cases of persistent stapedial artery [1].
2.1.2. Option against pathology:
- Infundibulum: The Pcom infundibulum should not be confused with an aneurysm Fig. 36 .
- ICA hypoplasia may be confused with dissection or fibromuscular dysplasia, while ICA agenesis may be confused with occlusion. Visualization of the skull base aids differentiation, as the bony carotid canal will be narrow in cases of hypoplasia and absent in cases of agenesis, but will appear normal in other acquired diseases Fig. 11 and Fig. 23 .
- Different patterns of perfusion abnormalities may occur with normal variations that can cause confusion, especially in the context of stroke:
- Asymmetry of CT or MR perfusion in the occipital lobes, in the case of unilateral fetal PCA. The contralateral side may show delayed perfusion because it is supplied by the posterior circulation Fig. 37 .
- Bilateral perfusion delay in the occipital lobes compared with the frontal and parietal lobes may be observed in the absence of bilateral Pcom Fig. 38 .
- Relative hypoperfusion in the PICA territory in cases of vertebral artery hypoplasia. Hypoperfusion may present as prolonged time-to-peak, prolonged main transit time, or decreased cerebral blood flow, but it never affects cerebral blood volume ) Fig.39 [12].
2.2. Hemodynamic effect of normal variants and abnormalities:
2.2.1. Understanding collateral function: The presence of hypoplasia or aplasia of segment(s) in the circle of Willis can affect collateral function when one or more arteries are occluded Fig. 15 .
2.2.2. Explains unclear cases of stroke:
Vascular conditions that cause changes in unexpected vascular territories can be explained by normal variations such as:
- Ischemia in the posterior territory may accompany ICA pathology due to the presence of fetal PCA Fig. 40 .
- Bilateral ischemia and ischemia in certain areas may draw attention to the presence of pathology in one of the options, such as:
- Bilateral anterior infarction in case of thromboembolism of azygos ACA or dominant bihemispheric ACA Fig. 41 .
- Bilateral mesencephalothalamic infarction with Percheron's artery Fig. 42 .
2.3. Association with vascular and nonvascular congenital anomalies and other diseases:
2.3.1. Association with aneurysms: Changes in vascular anatomy may be a sign of lack of vascular maturity and vulnerability to aneurysm formation. In the work of Lazzaro et al., normal variants of the circle of Willis were more common in cases with ruptured aneurysms than in cases of unruptured aneurysms [13]. Based on a review of the literature, the following variants and abnormalities were associated with aneurysms: Table 4 Fig. 43
- Fenestrations: The incidence of aneurysms (IoA) is approximately 7% of all fenestrations. A defect in the media of the fenestrated segment and turbulent flow at both ends of the fenestration can lead to aneurysm formation. Additionally, in the work of Hudák et al., fenestration was a common finding in patients with unexplained subarachnoid hemorrhage due to a weak arterial wall [1] [2] [14]
- ICA agenesis and hypoplasia: IoA 67% [2].
- A1 segment aplasia: IoA14% [15].
- Azygos ACA: IoA 41%. Due to increased flow from both segments of A1 [2].
- Persistent dorsal ophthalmic artery: IoA 45% [4].
- Persistent primitive olfactory artery: In the work of Uchino et al, 2 intracranial artery aneurysms were found in 14 patients with PPOA (IoA about 14%); one of them is in the hairpin bend (7%) [9].
- PTA: IoA 14% [1].
- Persistent hypoglossal artery: IoA 26% [16].
- Proatlantal intersegmental artery: IoA 10% [1, 2]
- Other variants and anomalies associated with aneurysms whose cases have been reported but not available include infraoptic ACA, superior anterior communicating artery, accessory MCA, MCA aplasia, variant PTA, and asymmetry of the circle of Willis [1, 2].
2.3.2. Association with other vascular anomalies and diseases:
- Fenestration of the vertebral artery is associated with arteriovenous malformation in 7% [6].
- PTA is observed in vascular anomalies such as AVM, carotid-cavernous fistula, and Moyamoya disease in 25% of cases [17].
- Proatlantal intersegmental artery: The incidence of cerebrovascular disorders such as AVM, vein of Galen malformation and aortic arch variants is 59% [18].
- Spontaneous vertebral artery dissection was slightly more common in subjects with hypoplastic vertebral artery than in controls (30.4% vs. 17.4%). It was also found that spontaneous vertebral artery dissection occurs more often with hypoplastic vertebral arteries than with dominant vertebral arteries (68% versus 32%) [19].
2.3.3. Association with other congenital anomalies:
- Azygos ACA may be associated with holoprosencephaly and migration abnormalities Fig. 44 [1].
- ICA hypoplasia is associated with anencephaly and basal telangiectasia [2].
- Fenestration of the vertebral artery may be associated with vertebral fusion [6].
2.3.4. Association with other disorders:
- Pituitary dysfunction and acromegaly in intrasellar “kissing” carotid arteries[2].
- It was found that migraine with aura is more common in patients with an open circle of Willis [20].
2.4. Preoperative planning for cranial surgery, head and neck surgery, and neurointerventional procedures:
The description of normal variations is very important for surgeons and interventional radiologists, as some of these variations must be considered to avoid catastrophic consequences during intervention.
2.4.1. The risk of catastrophic hemorrhage exists in the following cases:
- Transsphenoidal pituitary surgery in cases of PTA or intrasellar “kissing” carotid arteries.
- Middle ear surgery in cases of persistent stapedial artery and aberrant intratympanic ICA.
- Pharyngeal surgeries such as otopharyngeal tumor resection, tonsillectomy, adenoidectomy and palatopharyngoplasty in cases of aberrant lateral pharyngeal artery.
2.4.2. Knowledge of normal variations is important in interventional procedures. This knowledge may help to gain vascular access, such as dominant versus hypoplastic vertebral or variant access, or avoid complications during procedures such as tumor embolization through ECA catheterization in cases of MMA arising from the ophthalmic artery, which can lead to blindness . Fig.45 Fig.50
2.4.3. The presence of persistent carotid-basilar anastomoses should be excluded before certain procedures, such as the Wada test: in this case, injection of amytal can lead to loss of consciousness and apnea [2]
Fig.35 Meaning of normal options
Table 4: Variants associated with aneurysms and their occurrence
Fig. 36 3D TOF MRA, funnel-shaped dilatation with origin of Pcom (white arrow), which should not be confused with an aneurysm. Note the small aneurysm at the origin of the contralateral Pcom (red arrow). Also note the trifurcation of the ACA.
Fig. 37 MR perfusion, TTP map (a) shows slow perfusion in the left occipital lobe; no abnormalities were found in other perfusion parameters. 3D TOF (b), showing fetal PCA on the contralateral side (arrow).
Fig. 38 TTP perfusion map (a) shows a symmetrical delay in the occipital lobes, no deviations in other perfusion parameters were noted. 3D TOF shows no Pcom on both sides.
Fig. 39 (same patient as in Fig. 12) with hypoplasia of the right vertebral artery, which ends as the PICA. TTP map shows perfusion delay in the territory of the right PICA. An examination performed 6 weeks later for other reasons (not shown) showed no pathology in this area.
Fig. 40 MRI of a 56-year-old patient complaining of headache shows dissection of the left ICA (red arrows) with intramural hematoma on T2 (a) and T1FS (b). DWI (c) and ADC (d) show subacute infarction in the territory of the left PCA, which is due to the presence of fetal PCA (TOF not shown).
Fig.41 72-year-old patient with hemiplegia, epilepsy and impaired consciousness. DWI (a) and ADC (b) show bilateral infarcts in the ACA territory. DSA (c), shows proximal occlusion of the azygos ACA (arrow).
Fig. 42 Bilateral acute thalamic infarctions on DWI (a). DSA shows occlusion of the P1 segment of the left PCA (b). Minimal recanalization after intra-arterial thrombolysis (c), with mild opacification of the artery of Percheron (arrows) arising from the left PCA.
Fig. 43 Aneurysms (arrows) associated with abnormalities; a) A1 aplasia with Acom aneurysm. b) Azygos ACA with pericallosal aneurysm. c) fenestration of the basilar artery with proximal basilar aneurysm after coiling.
Fig. 44 Axial (a) and sagittal (b) MRI images of a child with holoprosencephaly, anterior cingulate fusion, and abnormal beak and genu corpus callosum. Note the empty flow of the anterior cerebral artery (arrow), which is single (azygos) and displaced anteriorly.
Fig. 45 55-year-old patient involved in an accident. Initial CT scan (a) shows a fracture of the left temporal bone. She later complained of pulsating tinnitus. DSA (c) with flat panel CT angiography (b and d) was performed. Reconstructed images showed the middle meningeal artery (yellow arrows) arising from the ophthalmic artery (blue arrow) and the traumatic AVM (red arrows) draining into the external jugular vein to form an aneurysm (orange arrow). Knowledge of this option is important when planning therapy.
Abbreviations:
- A1: Horizontal segment of ACA
- A2: Vertical segment of ACA
- ACA: Anterior cerebral artery
- Acom: Anterior communicating artery
- AICA: Anterior inferior cerebellar artery
- AVM: Arteriovenous malformation
- BA: Basilar artery
- CBF: Cerebral blood flow
- CBV: Cerebral blood volume
- CoW: Circle of Willis
- DSA: Digital subtraction angiograph
- ECA: External carotid artery
- ICA: Internal carotid artery
- IoA: Incidence of aneurysms
- M1: Sphenoidal segment of MCA
- MCA: Middle cerebral artery
- MMA: Middle meningeal artery
- MTT: Mean transit time
- PCA: Posterior cerebral artery
- Pcom: Posterior communicating artery
- PDOA: Persistent dorsal ophthalmic artery
- PICA: Posterior inferior cerebellar artery
- PPHA: Persistent primitive hypoglossal artery
- PPOA: Persistent primitive olfactory artery
- PTA: Persistent trigeminal artery
- SCA: Superior cerebellar artery
- sVAD: Spontaneous vertebral artery dissection