Epilepsy is a severe chronic disease characterized by recurrent, spontaneous seizures. The disease can be of a traumatic nature (occurs as a result of injury) or diencephalic (appears as a result of damage to the diencephalic structure of the brain).
In modern neurology, there are a large number of qualifications for epilepsy, which are based on the clinical and electroencephalographic manifestations of epileptic seizures. To record them, EEG and video monitoring are used.
The Yusupov Hospital offers a comprehensive diagnosis of epilepsy using these and other studies. By accurately identifying the type of disease, epileptologists select an individual treatment regimen that is most effective for a particular form of epilepsy. Modern medical equipment, innovative therapeutic techniques and an individual approach provide high treatment results – patients’ health status significantly improves, and the development of new epileptic seizures is prevented.
Classification of the disease
Epilepsy can be congenital (idiopathic) or acquired (symptomatic).
Symptoms of congenital epilepsy appear already in childhood or adolescence. The disease is characterized by a benign course and a favorable prognosis. The right approach to therapy can ensure complete elimination of the need to take medications. This form of pathology is not accompanied by damage to the brain matter. The excitability of the brain is explained by an increase in the electrical activity of neurons. Seizures of congenital epilepsy can lead to complete loss of consciousness.
Congenital epilepsy develops due to genetic defects in brain structures. As a result, the brain is constantly in convulsive readiness, since an attack can happen suddenly at any moment. The development of congenital epilepsy can be triggered by the following factors:
- birth injuries;
- hypoxia, fetal asphyxia;
- intrauterine infections during pregnancy.
Acquired epilepsy is a more complex and severe illness that can occur in people of any age and is difficult to treat. The disease occurs as a result of pathological changes in the brain caused by exposure to certain external factors. During an epileptic seizure, the patient does not lose consciousness, but cannot control a certain part of the body that was affected by the attack.
Acquired epilepsy occurs as a result of the influence of unfavorable factors on the brain, which in turn leads to the formation of an epileptic focus that generates an excess electrical impulse.
Treatment for epilepsy
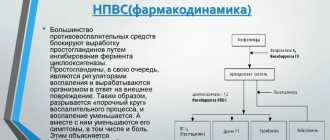
If you believe the results of modern drug therapy, then it, like no other, is the main and main way to combat epilepsy. The effectiveness of drug therapy is up to 69%, which can significantly reduce the threshold for the occurrence of epileptic seizures, as well as their further spread.
In addition, in the twenty-first century, surgical techniques have also found widespread use (in the treatment of epilepsy). Of course, intervention through brain surgery is most often used only in cases where medications are no longer effective.
According to highly qualified neurologists and psychiatrists, several other methods of treating the disease have also proven successful, namely:
A diet called Ketogenic. Today, this is one method to reduce the number of epileptic seizures, but this diet is prescribed exclusively for severe forms of epilepsy in cases where medications are no longer effective.
Alternative methods of treating epilepsy also include stimulation of the vagus nerve, as well as multiple subpial transsection. The latter was created with the aim of controlling or eliminating an epileptic focus in the brain, which can no longer be safely removed. That is why the surgeon makes small incisions on the brain tissue without disturbing its normal activity at all.
Local epilepsy
When diagnosing epilepsy, it is important for specialists to understand whether the seizure affects one of the brain hemispheres or the entire brain, thus identifying the type of seizure - partial or generalized.
Local (focal, partial) epilepsy can be simple or complex. With complex seizures, patients' consciousness is impaired, but with simple ones this does not happen. Simple seizures in local epilepsy are characterized by a variety of manifestations, which depend on the localization of epileptic activity in a particular area of the cerebral cortex. Simple focal seizures are characterized by the occurrence of clinical convulsions in a certain part of the body and their further spread to neighboring areas.
Simple partial seizures can be:
- tonic – they are characterized by the patient adopting a forced posture and muscle tension. After a seizure, the muscles involved are temporarily weakened;
- sensory – patients experience illusions, hallucinations, any part of the body may become numb or tingling;
- vegetative - during attacks, piloerection, sweating, rapid heartbeat, and a feeling of a lump in the throat appear. With such seizures, patients experience a variety of mental disorders.
During complex seizures, patients' consciousness is impaired and they do not respond to external stimuli.
The duration of such an attack is usually from 30 to 90 seconds, after which drowsiness and fatigue appear. Complex seizures of local epilepsy must be distinguished from absence seizures. In the first case, the source is a focus of pathological activity, and the other is a primarily generalized seizure. The duration of focal seizures is often longer and they are characterized by confusion. Absence seizures are not accompanied by a similar phenomenon. The development of local epilepsy seizures is caused by focal damage to the cerebral cortex; they require different treatment than absence seizures.
Classification of epilepsy
International League Against Epilepsy (ILAE) Working Group 2014 Practical Clinical Definition of Epilepsy.
Epilepsy is a brain disease corresponding to any of the following conditions:
- At least two unprovoked (or reflex) epileptic seizures > 24 hours apart.
- One unprovoked (or reflex) epileptic seizure and a probability of recurrent seizures corresponding to the overall risk of relapse (³ 60%) after two unprovoked epileptic seizures in the next 10 years.
- Diagnosis of epileptic syndrome.
Criteria for resolution of epilepsy include reaching a certain age in patients with age-dependent epileptic syndrome or being seizure-free for 10 years in patients who have not received anticonvulsants for more than 5 years.
Classification of epilepsy (International League Against Epilepsy (ILAE) 2021)
The classification of epilepsy is carried out after determining the criteria for diagnosing epilepsy (defined above). Classification is carried out using a three-level ranking - determining the type of seizures, the type of epilepsy and the epilepsy syndrome. Neuroimaging, EEG and other studies, when available, help improve classification at all three levels. Where possible, diagnosis should be made at all three levels. The etiology of epilepsy should be established from the very beginning and at each stage of the entire diagnostic path. Knowledge of etiology can help optimize classification and has important therapeutic implications for the patient.
Structure of the 2021 ILAE Classification of Epilepsy.
Note. *Assessed by the onset of the attack.
Avakyan G. N. Blinov D. V. Lebedeva A. V. Burd S. G. Avakyan G. G. Classification of epilepsy of the International League Against Epilepsy: revision and update 2021. Epilepsy and paroxysmal conditions. 2017; 9 (1): 6–25. DOI: 10.17749/2077–8333.2017.9. 1.006–025.
Epilepsy classification algorithm:
- At the first stage (level), the type of attack is determined: focal, generalized or with an unknown onset.
- At the second stage (level), the type of epilepsy is established: focal, generalized or combined focal and generalized, or unknown.
- At the third stage (level), the epileptic syndrome and comorbidity are determined. Epileptic syndrome is a set of characteristics, including the type of attack, EEG and neuroimaging data, often has an age-dependent nature, provoking factors, chronological dependence and, in some cases, a definite prognosis.
- At the fourth stage (level), the etiology of epilepsy is established: structural, genetic, infectious, metabolic, immune, or with an unknown etiology.
Generalized epilepsy
Patients with generalized epilepsy have generalized seizure types and may have typical interictal and/or ictal EEG patterns that accompany generalized seizure types (eg, generalized spike-wave). Concomitant family history of generalized seizure types or generalized epilepsy.
Genetic/idiopathic generalized epilepsy is epilepsy with generalized seizures associated with generalized epileptiform EEG patterns, such as generalized spike-wave activity, which is thought to have a genetic etiology. However, this does not always mean that these epilepsies are inherited or can be passed on to offspring, since the genetic etiology may be a spontaneous new mutation or inheritance may be complex. Thus, the term "idiopathic generalized epilepsy" is used as a synonym for genetic generalized epilepsy, and the clinician may choose which term to use depending on the importance of the emphasis on genetic inheritance for a particular patient. Genetic/idiopathic generalized epilepsies include childhood absence epilepsy, juvenile absence epilepsy, juvenile myoclonic epilepsy, and epilepsy with generalized tonic-clonic seizures.
Focal epilepsy
Patients with focal epilepsy have focal seizure types and may have typical interictal and/or ictal EEG patterns that accompany focal seizure types (such as focal sharp waves or focal interictal slowing). Neuroimaging demonstrates the focal structural brain abnormality and aids in diagnosis, although patients with a genetic etiology and normal imaging may also have focal epilepsy. Focal epilepsies can be unifocal, multifocal or hemispheric.
Combined generalized and focal epilepsy
Patients may have both generalized and focal seizure types, with interictal and/or ictal EEG patterns accompanying both seizure types. Patients with Dravet syndrome and Lennox-Gastaut syndrome may have generalized and focal epilepsy.
Unknown epilepsy
The term "unknown" is used to describe a situation where it is understood that a patient has epilepsy, but it is not possible to determine whether it is focal, generalized, or a combination of focal and generalized. This occurs when there is insufficient information to classify epilepsy, for example, if the EEG is normal/uninformative.
Epilepsy syndromes
While conceptualizing epilepsies by their etiology is important, epilepsies can also be organized (according to well-established conventional clinical and EEG characteristics) into epileptic syndromes. Such syndromes have a typical age of seizure onset, specific seizure types and EEG characteristics, and often other features that, taken together, allow the diagnosis of a specific epileptic syndrome. Identification of the epilepsy syndrome is useful as it provides information about what underlying etiologies should be considered and what anticonvulsants may be most helpful. Some epilepsy syndromes exhibit seizure aggravation with certain anticonvulsants, which can be avoided with early diagnosis of the epilepsy syndrome.
Epileptic syndromes
Neonatal and infant period:
- self-limited neonatal seizures and self-limited familial neonatal epilepsy;
- self-limited familial and non-familial infantile epilepsy;
- early myoclonic encephalopathy;
- Ohtahara syndrome;
- West syndrome;
- Dravet syndrome;
- myoclonic epilepsy of infancy, infantile epilepsy with migrating focal seizures;
- myoclonic encephalopathy in non-progressive diseases;
- febrile seizures, febrile seizures plus, genetic epilepsy with febrile seizures plus.
Childhood:
- epilepsy with myoclonic-atonic (formerly astatic) seizures;
- Lennox–Gastaut syndrome;
- febrile seizures, febrile seizures plus;
- absence epilepsy;
- epilepsy with myoclonic absence seizures;
- childhood occipital epilepsy with early onset (Panayotopoulos syndrome);
- late-onset childhood occipital epilepsy (Gastaut syndrome);
- photosensitivity occipital epilepsy;
- self-limited epilepsy with central temporal spikes;
- atypical epilepsy with central temporal spikes;
- epileptic encephalopathy with continued peak-wave activity during sleep;
- Landau-Kleffner syndrome;
- autosomal dominant nocturnal frontal lobe epilepsy.
Adolescence and adulthood:
- juvenile absence epilepsy;
- juvenile myoclonic epilepsy;
- epilepsy with isolated generalized tonic-clonic seizures;
- autosomal dominant epilepsy with auditory manifestations;
- other familial temporal lobe epilepsy.
Any age:
- familial focal epilepsy with variable focus;
- reflex epilepsy;
- progressive myoclonic epilepsy.
Etiology of epilepsy
Our understanding of the underlying causes of epilepsy has increased significantly in recent years, supported by advances in modern neuroimaging and genetic testing. Terminology such as "idiopathic", "cryptogenic" and "symptomatic" is no longer used. Epilepsies are now described more accurately by specific underlying causes.
Genetic etiology
The concept of genetic epilepsy is that epilepsy, as we understand it, is the direct result of a known or suspected genetic defect(s) in which seizures are the primary symptom of the disorder. A genetic defect can occur at the chromosomal or molecular level. It is important to emphasize that “genetic” does not mean the same as “inherited,” since de novo mutations are not uncommon. The presence of a genetic etiology does not exclude an exogenous influence on the occurrence of epilepsy.
The most important genetic causes of epilepsy that can be identified through clinical testing are:
- chromosomal abnormalities;
- gene abnormalities.
There are many ways that genetic factors can contribute to the development of epilepsy. Certain genetic factors may not have been inherited and may not be passed on to offspring. Here are some important genetic concepts used on this website and their definitions:
- inherited gene abnormalities, autosomal dominant, autosomal recessive and Mendelian inheritance;
- acquired gene abnormalities - de novo, sporadic, mosaicistic, germinal and somatic;
- polygenic/complex genetic etiology.
Structural etiology
Structural epilepsies are defined as having a significant structural abnormality of the brain that is associated with a significantly increased risk of epilepsy. A structural brain abnormality may be acquired (for example, due to a stroke, injury, or infection) or may be genetic in origin; however, as we currently understand it, a structural brain abnormality is a distinct disorder located between an acquired or genetic defect and epilepsy.
Neuroimaging
Magnetic resonance imaging (MRI) using a 1.5 Tesla machine is the minimum standard test to rule out structural abnormality. In this research, it is important to perform epilepsy-specific protocols that allow for the careful study of specific acquired abnormalities (eg, hippocampal sclerosis) and subtle cortical malformations such as focal cortical dysplasia. 3 Tesla imaging and the use of advanced software analysis techniques can help identify structural abnormalities not apparent with conventional MRI. Interictal and ictal EEG, along with complementary functional neuroimaging studies such as PET, SPECT, and MEG, help closely examine a specific brain region and identify subtle abnormalities. In young children under 2 years of age, subtle abnormalities cannot be detected due to incomplete myelination, and repeated examination is required over time.
Common structural brain abnormalities associated with epilepsy:
- malformations of the cerebral cortex;
- vascular malformations;
- hippocampal sclerosis;
- hypoxic-ischemic structural abnormalities;
- traumatic brain injury;
- tumors;
- porencephalic cyst.
Metabolic etiology
Metabolic epilepsies are defined as having a specific metabolic disorder associated with a significant risk of developing epilepsy. Metabolic disorders have a genetic origin; however, as we currently understand it, metabolic abnormalities represent a distinct disorder standing between the genetic defect and epilepsy.
Important metabolic epilepsies:
- deficiency of biotinidase and holocarboxylase synthase;
- cerebral folate deficiency;
- creatine disorders;
- attacks due to folate cycle disorders;
- glucose transporter 1 (GLUT1) deficiency;
- mitochondrial disorders;
- peroxisomal disorders;
- pyridoxine-dependent epilepsy.
Immune etiology
Immune epilepsies are defined as having a strong immune-mediated etiology with evidence of inflammation of the central nervous system, which has been shown to be associated with a significantly increased risk of developing epilepsy.
Important immune-mediated epilepsies:
- Rasmussen's syndrome;
- Antibody-mediated epilepsy.
Infectious etiology
The most common etiology of epilepsy worldwide is infectious, especially in developing countries. Infections in the central nervous system can cause both acute symptomatic seizures (which are closely related to the timing of the primary infection) and epilepsy. Infectious etiologies include tuberculosis, HIV, cerebral malaria, neurocysticercosis, subacute sclerosing panencephalitis, cerebral toxoplasmosis. These infections sometimes have a structural correlate, but the underlying cause of epilepsy is identified as an infectious process. Infectious etiologies may have specific treatment implications. There are also public health implications, as preventing such infections may reduce the burden of epilepsy, especially in developing countries. The most common of these infections are:
- bacterial meningitis or meningoencephalitis;
- cerebral malaria;
- cerebral toxoplasmosis;
- cytomegalovirus infection;
- HIV;
- neurocysticercosis;
- tuberculosis;
- viral encephalitis;
- subacute sclerosing panencephalitis;
- other infections (toxocaryosis, schistosomiasis, Lyme disease (neuroborreliosis).
Unknown etiology
“Unknown” etiology should be viewed neutrally and mean that the nature of the underlying cause of epilepsy is not yet known; it may be a fundamental genetic defect or a separate, as yet identified, disorder.
Epilepsy simulators
There are a number of conditions associated with recurrent paroxysmal events that can mimic symptoms and be misdiagnosed as epilepsy. It is important that these disorders are taken into account when assessing paroxysmal events, as the incidence of misdiagnosis in epilepsy is high worldwide. Medical history and video recording of attacks help establish the correct diagnosis. There are some conditions in which epileptic and non-epileptic events can coexist.
Syncopal and anoxic attacks
- vasovagal syncope;
- reflex anoxic attacks;
- affective respiratory apnea;
- hyperventilation syncope;
- self-induced fainting using the Valsalva method;
- neurological syncope (Chiari malformation, hyperexlexia, paroxysmal pain disorder);
- forced upper airway obstruction;
- orthostatic intolerance;
- QT prolongation and cardiac syncope;
- dyspnea-cyanotic fainting (with tetralogy of Fallot).
Behavioral, psychological and psychiatric disorders
- daydreaming/inattention;
- self-satisfaction;
- eidetic images;
- outbursts and reactions of rage;
- sensations outside the body;
- panic attacks;
- dissociative states;
- non-epileptic seizures;
- hallucinations in mental disorders;
- fictitious/fake disease.
Sleep-related conditions
- sleep-related rhythmic movement disorders;
- hypnotic shudders;
- parasomnias;
- sleep disturbances in the REM sleep phase;
- benign neonatal sleep myoclonus;
- periodic leg movements;
- narcolepsy-cataplexy.
Paroxysmal movement disorders
- tics;
- stereotypies;
- paroxysmal kinesiogenic dyskinesia;
- paroxysmal non-kinesiogenic dyskinesia;
- paroxysmal exercise-induced dyskinesia;
- oculogyric crisis;
- episodic ataxia;
- alternating hemiplegia;
- hyperexlexia;
- opsoclonus-myoclonus syndrome.
Migraine-associated disorders
- migraine with visual aura;
- familial hemiplegic migraine;
- benign paroxysmal torticollis;
- benign paroxysmal vertigo;
- cyclic vomiting.
Various events
- benign myoclonus of infancy and shaking attacks;
- Sandifer syndrome;
- non-epileptic head falls;
- spasmus nutans;
- increased intracranial pressure;
- familial rectal pain syndrome;
- spinal myoclonus.
Diagnosis of epilepsy
From a modern point of view, 5 stages are defined:
- description of the paroxysmal event, possibly based on medical history;
- classification of attack (history, clinic, EEG, video-EEG monitoring);
- diagnosis of a form of epilepsy (history, clinical picture, EEG, video-EEG monitoring, neuroimaging);
- establishing the etiology of epilepsy (MRI, karyotyping, biochemical studies, muscle biopsy, etc.);
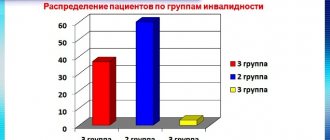
- diagnosis of concomitant diseases and determination of disability.
Generalized epileptic seizure
In a generalized epileptic seizure, both hemispheres of the brain are involved, so there are no precursors to its development. Generalized epileptic seizures are divided into the following types:
- typical absence seizures - they are characterized by short attacks of impaired consciousness, during which the patient’s gaze freezes or stops. At the end of the seizure, there is no confusion. Lack of treatment threatens multiple repetitions of absence seizures. As a rule, they begin to appear in childhood and continue into adulthood;
- atypical absence seizures - attacks are characterized by a pronounced beginning and end, long duration, mental retardation and motor impairment;
- clonic seizures – myoclonic jerks occur;
- myoclonic seizures – patients develop short, sudden convulsive twitches. The attack typically involves the head, neck, upper and lower extremities. Such attacks can be isolated or combined with other seizures;
- tonic seizures – bilateral short attacks of muscle tension develop in the limbs and torso;
- atonic seizures – the patient’s muscles suddenly and briefly lose their tone. There is a sudden drooping of the head or a fall of the patient. Despite the fact that consciousness is restored quite quickly, such seizures threaten to cause injury;
- generalized epileptic seizures - patients completely lose consciousness, their tonic tension in the muscles of the trunk, arms and legs disappears. Most often, the seizure is preceded by a piercing scream, the appearance of which is associated with the expulsion of air through the closed vocal cords. The muscles tense, after which a convulsive attack begins, which is characterized by severe muscle tension, which can be accompanied by fractures and dislocations. After an attack, a person has a headache and drowsiness.
The main symptoms of epilepsy in adults include:
Focal seizures . Most often, medical practice associates them with the occurrence of excess electrical discharge in one of the areas of the cerebral cortex. During these attacks, convulsions or sudden numbness or other sensations in the arms, legs, facial muscles, etc. are usually observed. Most often, the person remains conscious and clearly remembers his sensations. The duration of a focal attack lasts from 15-20 seconds to several minutes (rarely up to several tens of minutes).
Generalized seizures:
Convulsive. Often the first sign of epilepsy in an adult is tension in the muscles of the chest and larynx, a high-pitched cry, and even unnatural biting of the tongue. Within a few seconds, muscle tension occurs, followed by twitching and relaxation after 3-4 minutes (in this case, involuntary urinary incontinence or defecation can often occur). Next, a person may experience severe drowsiness, fuzzy and unclear consciousness, aching headache in the back of the head with rapid onset of sleep.
Non-convulsive (absence seizures). As mentioned above, these non-convulsive seizures occur more often in childhood or early adolescence. At the time of an epileptic attack, the child’s gaze suddenly freezes and is directed at one point, while his eyelids may twitch, his head may throw back, or slight nods forward are noted. The duration of these attacks is usually no more than 30 seconds.
Types of epilepsy. Seizure symptoms
The classic manifestation of epilepsy is the presence of seizures.
They arise unexpectedly and do not always depend on environmental factors. In certain cases, it is possible to predict the occurrence of an attack based on the patient’s complaints of general malaise. He may be tormented by headaches, poor sleep, lack of appetite, and irritability. During an attack, convulsions occur, during which the head is thrown back, the limbs and torso are stretched, breathing is held, and the veins of the neck swell. Such convulsions are called tonic, their duration is about 20 seconds. They are followed by clonic convulsions, which manifest themselves in jerking movements. This phase lasts up to 3 minutes. The patient may experience foaming at the mouth mixed with blood, this is due to the accumulation of saliva in the mouth and possible biting of the cheek or tongue.
Modern medicine knows many types of epilepsy. There are main types of epilepsy:
- absence epilepsy. Characterized by a lack of reaction to events happening around;
- Rolandic epilepsy. It is characterized by numbness of the skin, spasms of certain parts of the body, and excessive salivation. Mostly boys aged 8-10 years are affected;
- myoclonic epilepsy. Characterized by the presence of epileptic seizures, myoclonus (muscle contractions), sometimes mental disorders are noticeable;
- post-traumatic epilepsy. Characterized by the presence of seizures as a result of traumatic brain injury;
- alcoholic epilepsy. Typical for people suffering from alcohol addiction. Manifested by convulsions and loss of consciousness. After the seizure ends, the patient may fall asleep for several hours;
- epilepsy of newborns;
- temporal lobe epilepsy. It is chronic in nature with gradual progression;
- epilepsy in children. Seizures may not be related to epilepsy. Careful diagnosis is necessary;
- non-convulsive epilepsy. Characterized by the absence of symptoms expressed by convulsions. It manifests itself as a lack of reaction to external stimuli, a blank look, and loss of consciousness.
Epilepsy, regardless of type, requires careful treatment.
Diagnosis and treatment of epilepsy is carried out by epileptologists at the Yusupov Hospital. Make an appointment
Status epilepticus
Status epilepticus is said to occur when seizures are repeated multiple times, so often that consciousness does not have time to recover between them.
Patients experience impaired hemodynamics and respiratory function, and twilight consciousness appears. Convulsive attacks are accompanied by soporous and comatose states, seriously threatening the life of the epileptic. In the tonic phase, a spasm of the respiratory muscles occurs, and apnea appears with the characteristic symptoms listed above. There is an appearance of increased and shallow breathing associated with hypoxia, which is accompanied by hypocapnia. With this condition, epileptic activity increases and the duration of the seizure increases.
Patients who have fallen into a coma suffer from pharyngeal respiratory paralysis with loss of the pharyngeal reflex. In the respiratory tract, salivary secretion accumulates, as a result of which breathing worsens and cyanosis occurs. Hemodynamics change, heart rate increases, blood pressure increases, myocardial ischemia develops, metabolism is disrupted, resulting in metabolic acidosis, and intracellular respiration is disrupted.
Diagnostics
If you have epilepsy attacks, you should immediately seek help from a neurologist.
The Yusupov Hospital has an epileptologist who specializes in this disease. The doctor will conduct diagnostics using modern equipment. At the Yusupov Hospital, the following examination methods are used for this: encephalography, neurosonography, MRI, CT, Dopplerography of cerebral vessels, ultrasound if necessary. The doctor will determine the exact form and cause of the disease and prescribe appropriate treatment.
It is important to follow the exact recommendations of your doctor to achieve the maximum effect of treatment. According to statistics, with the correct course of treatment, attacks will soon decrease and soon disappear altogether.
Treatment
Epilepsy is a serious stress that is experienced by both the patient’s loved ones and himself.
A person experiences constant fear, waiting for each new attack, and as a result he develops depression. Therefore, neurologists at the Yusupov Hospital make every effort to help patients suffering from epilepsy, selecting treatment with the most modern antiepileptic drugs that can prevent the development of new seizures. In the fight against the disease, epileptologists at the Yusupov Hospital adhere to the following therapeutic principles:
- early start of treatment;
- continuity;
- complexity;
- continuity;
- individual approach.
Treatment of patients with epilepsy in the neurology clinic of the Yusupov Hospital is aimed at achieving the following goals:
- preventing the development of new epileptic seizures;
- relief of pain during attacks;
- reducing the frequency of epilepsy attacks;
- stopping medications or reducing side effects from their use;
- training relatives of an epileptic in the correct handling of the patient;
- conducting socio-neurological rehabilitation to improve the patient’s quality of life;
- the use of complex therapy for patients suffering from epilepsy and related diseases.
The Neurology Clinic of the Yusupov Hospital provides comprehensive, regular and long-term treatment for epileptic seizures.
It consists of dehydration, anticonvulsant, restorative and resorption procedures. Before starting treatment, a team of neurologists and diagnosticians at the clinic determine the type of epileptic seizures and the etiology of epilepsy. For drug therapy, the most optimal drug is selected, the dosage of which is constantly increased until the attacks completely stop. If taking the drug does not achieve the desired result, additional medications are prescribed.
The effectiveness of therapy largely depends on the actions of the patient himself - his compliance with all the recommendations of the attending physician. Interruption of the drug may result in status epilepticus.
In the neurology clinic of the Yusupov Hospital, during the treatment of epilepsy, doctors with extensive experience in treating all types of diseases use the latest technologies and the latest generation antiepileptic drugs. To conduct diagnostics and consult a neurologist or epileptologist at the Yusupov Hospital, you must make an appointment by phone or on the clinic’s website.
ICD-10 classification
Let's start with ICD-10 [1] - the leading official classification on which statistical recording, expert decisions, prescription of subsidized drugs, etc. are based.
First of all, it is surprising why in an official document for Russia, instead of the euphonious scientific term “attack,” the stigmatizing term “seizure” is used. Obviously, when ICD-10 was translated into Russian, such ethical nuances were simply not thought about.
In addition, in some points the epileptic syndrome, seizures, form of epilepsy, etiology of epilepsy, localization or generalization are brought together, i.e. there is an intersection of concepts. Thus, the general scientific principles of classification are violated. In the description of epilepsy, terms with unclear meaning are used that are difficult for a practicing physician to understand: “others,” “other specified forms,” “other types,” “special syndromes,” “specified,” “unspecified.” With this approach, the basis for classification is completely absent, opening up a wide field for arbitrary interpretation. How can you treat something if it is “unspecified”? This is similar to putting a criminal with an “unspecified appearance” on the international wanted list.
Thus, there is an overlap of concepts in ICD-10; the sum of the classification members does not equal the volume of the generic concept; subclassification is not continuous; there are no classification grounds, instead of which non-operational terms are introduced: “other”, “special”, “specified”, “unspecified”.