We usually don’t hear about epilepsy as often as, say, heart attacks and strokes. However, almost each of us, one way or another, is familiar with this disease, if not personally, then from the stories of others whose relatives or friends suffer from this disease. And this is no coincidence, because epilepsy is observed in almost 5% of the population of our planet, and in children this disease is registered three times more often than in adults. And the general term “epilepsy,” according to the conclusion of modern practicing neurologists, combines more than fifty diseases that differ in clinical manifestations and treatment, including the most common generalized epilepsy.
What is generalized epilepsy
Generalized epilepsy is a chronic pathology of the brain, which is characterized by the formation (in both hemispheres) of neural impulses of excessive intensity. During the resulting attacks (which become repeated), many of the patient’s organic functions are temporarily disrupted:
- motor
- vegetative
- sensitive
- mental
Generalized epilepsy today means all epileptic forms based on the stereotypical occurrence of epileptic seizures. The latter consist of absence seizures (short-term, literally for a few seconds, switching off consciousness), generalized myoclonic (associated with involuntary muscle tension) and tonic-clonic (associated with changes in muscle tension and intermittent muscle contractions) paroxysms.
What types of generalized epilepsy are known?
Depending on the nature of the origin, generalized epilepsy is usually divided into:
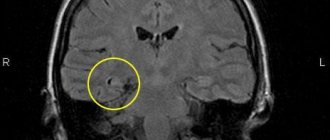
- idiopathic - genetically transmitted and, mainly, occurring in childhood or adolescence (or with possible manifestation in adulthood), characterized by the absence of pathologies of the nervous system and, in particular, structural changes in the brain (except for changes recorded using EEG and MRI);
- symptomatic – arising as a result of traumatic brain injuries (in most cases during childbirth), or as a result of extensive organic brain damage after neurointoxication, infectious diseases, as well as against the background of hereditary pathologies, neoplasms, and some dysmetabolic conditions (including intrauterine fetal hypoxia);
- cryptogenic – with unknown etiology.
Depending on the presence of seizures in attacks, generalized epilepsy is divided into:
- non-convulsive (characterized by the presence of absence seizures in attacks);
- convulsive (characterized by tonic-clonic phases of the attack).
Causes of GE
Epilepsy is a polyetiological disease that can be caused by any disease or injury to the central nervous system. Every structural damage to the brain causes an imbalance of inhibitory and excitatory neurotransmitters. Because of this, the neuron membrane becomes more permeable to Na+ and Ca2+ ions, and the number of channels for K+ and Cl-, on the contrary, decreases. As a result, neurons become hypersensitive to the discharges of other neurons, which leads to the formation of an epileptic focus.
Structural brain disorders can occur due to the following reasons:
- perinatal - viral infections of the mother during pregnancy (rubella, herpes), the mother's use of toxic drugs and medications prohibited for pregnant women, birth injuries;
- postnatal - concussions and other injuries, central nervous system infections (meningitis or encephalitis), tumors and hemorrhages.
If one of the parents has epilepsy, then the risk of it occurring in the child is no more than 10%.
Based on their appearance, epilepsy is divided into idiopathic, symptomatic and cryptogenic. Idiopathic - epilepsy with a known or possible genetic predisposition. Such patients do not have a history of head injuries, no brain damage is detected during examination, and there are no mental disorders before the attack occurs. Symptomatic - seizures occur as a result of exogenous factors leading to brain damage (trauma, infection, hemorrhage, ischemia, etc.) with manifestation. Cryptogenic is characterized by the absence of any cause; the epileptic syndrome occurs spontaneously.
Expert opinion
Author: Olga Vladimirovna Boyko
Neurologist, Doctor of Medical Sciences
According to the latest WHO data, epilepsy affects 4-10 people per 1000 population. Currently, doctors are registering an increase in incidence. This is due to various provoking factors. It has been proven that epileptic seizures occur more often in residents of countries with a low or average level of development, however, in Russia the disease accounts for 2.5% of cases of neurological pathology. Epilepsy ranks first in the structure of disability: 30% of patients become disabled in groups 1 or 2.
Epilepsy can manifest itself against the background of other diseases - this type of pathology is called symptomatic. Doctors at the Yusupov Hospital perform thorough diagnostics to determine the causes of seizures. This is necessary to prescribe the correct therapy. The examination is carried out using European equipment. The diagnosis is made based on MRI, CT, and EEG data. In a modern laboratory, blood diagnostics are carried out. Symptomatic epilepsy requires an individual approach to treatment. Neurologists at the Yusupov Hospital are developing a personal treatment plan, including new drugs with proven effectiveness.
What are the symptoms of generalized epilepsy
The symptoms of generalized epilepsy usually depend on its form.
IdiopathicSymptomatic
Age of first manifestation Childhood and adolescence (mainly up to 21 years). Any age period, but for congenital and hereditary pathologies manifestations in early childhood are typical.
Neurological status Symptoms are scattered, occasionally focal. Depends on the underlying disease, which determines general cerebral and focal symptoms.
Nature of attacks Epileptic paroxysms of a primary generalized nature: with myoclonic convulsions (short-term twitching of the limbs), absence seizures (with lack of attention), generalized tonic-clonic convulsions (muscle tension, followed by intermittent muscle contractions against the background of a lack of consciousness, which often ends in involuntary urination and muscle pain). relaxation).Generalized epileptic seizures (against the background of clinical manifestations of the underlying disease). They are characterized by general muscle tension with a short-term cessation of breathing, followed by convulsions that can last from 10 seconds to 20 minutes.
Cognitive manifestations Mental abilities are normal, although sometimes they may temporarily decrease slightly (in approximately 5-8% of patients). There is a decrease in intellectual abilities; mental retardation and cerebral palsy may develop in children.
There are generalized, focal (partial, local) and unclassified seizures (classification of the International League Against Epilepsy, 1981).
Generalized seizures include tonic-clonic, clonic, tonic, atonic, myoclonic seizures, as well as absence seizures, simple and complex (typical and atypical according to the EEG pattern). Clinically, generalized seizures are manifested by loss of consciousness (an obligate symptom), massive autonomic disturbances, and in some cases - bilateral convulsions, tonic, clonic or myoclonic. The EEG during a seizure reveals bilateral synchronous and symmetrical epileptic discharges.
Partial seizures are those whose clinical structure, as well as the EEG pattern, indicate pathological activation of an isolated group of neurons in one of the cerebral hemispheres. Partial seizures can develop into general - secondary generalized seizures. In the latter case, the partial discharge is the aura of the seizure. The clinical picture of partial seizures is characterized by symptoms of irritation (or loss) in one functional system: sensory, motor, autonomic, mental. There may be a disturbance or switching off of consciousness that occurs in various phases of the attack - complex partial seizures. Loss of consciousness is not an obligate manifestation of a partial seizure. Simple partial seizures are not accompanied by formal disturbances of consciousness.
Unclassifiable seizures cannot be described on the basis of the criteria adopted to distinguish the above-mentioned types of paroxysmal conditions. These are, for example, seizures of newborns with chewing movements, rhythmic movements of the eyeballs, hemiconvulsive seizures.
Seizures can be isolated, occur in series (temporarily increase their frequency, for example, up to six or eight times during the day), occur as status epilepticus (the debut of epilepsy, a special type of its course, a reaction to errors in anticonvulsant therapy, to high temperature and somatic diseases). Status epilepticus is a condition in which another seizure develops against the background of severe disorders associated with the previous one. The frequency of seizures during status is from 3 to 20 per hour (Karlov, 1990). In the status of generalized seizures, the patient does not regain consciousness.
Seizures are observed in epilepsy, in the clinical structure of current organic diseases of the brain - epileptic syndrome, and also as an expression of a nonspecific reaction of the body to extreme influences - epileptic reaction (Boldyrev, 1990). Epileptic syndrome (“symptomatic epilepsy” by some authors - H. G. Khodos, 1974) is observed in brain tumors, encephalitis, abscesses, aneurysms, hypertension and cerebral atherosclerosis, chronic mental diseases at remote stages of their dynamics, atrophic processes, parasitic diseases brain, metabolic disorders, chromosomal diseases. An epileptic reaction occurs in response to various factors: hypoglycemia, electrical trauma (a typical example is seizures during electroconvulsive therapy), intoxication (tetanus toxin), and medication, in particular Corazol. The cause of the epileptic reaction may be asphyxia. We have met teenagers who tried to induce euphoric states by mild asphyxia, and this was accompanied by seizures in some of them. One of the most common forms of epileptic reaction in children is febrile seizures (occurring against a background of high fever). Febrile seizures are more often observed in children (up to the age of five or six, there is a physiological increase in convulsive readiness). They occur during a high, especially “shooting” temperature reaction, are usually one-time, and do not have a focal component. In children suffering from epilepsy, seizures may become more frequent due to fever (this also happens in adult patients) or appear for the first time. Seizures of epilepsy are indicated by: their frequency, repetition with each rise in temperature, appearance at a low temperature (below 38°), the presence of a focal component, age over three or four years. Epileptic reactions occur especially easily with increased convulsive readiness. Their repetition can lead to the formation of epilepsy. Seizures of “reflex” epilepsy are also caused. The occurrence of a seizure is associated with sensory stimuli. The nature of the latter is reflected in the name of the attacks. Audiogenic seizures are triggered by sudden acoustic stimuli, while photogenic seizures are triggered by optical stimuli. Seizures can occur under the influence of tactile, proprioceptive and visceral stimuli (touching the body, sudden movement, pain). Rhythmically repeated stimuli can also lead to a seizure (flickering of oncoming train cars, electrical poles, zebra stripes on pedestrian sections of the road; images on a television screen - “television epilepsy”). Seizures are sometimes provoked by vegetative reactions (erection, defecation), complex but strictly defined actions (for example, a patient has seizures every time she goes to the sink, turns on the tap, and when the water starts to flow out, she loses consciousness). Sometimes seizures occur in connection with violent emotions - affective epilepsy. Probably similar to the latter are seizures associated with the perception of music - musicogenic epilepsy. Patients with reflex seizures can prevent, but sometimes, on the contrary, consciously cause them. Sometimes there are patients who experience an irresistible urge to cause seizures. This is due to affective disorders, auto-aggressive tendencies, or represents a special type of psychomotor seizure. Reflex seizures are more often observed in patients with epilepsy.
Here is a description of some epileptic seizures, initially generalized.
Tonic-clonic seizures. In the first, tonic phase, there is a sudden loss of consciousness, tonic tension of voluntary muscles, a fall, accompanied by a loud cry. There is cessation of breathing, increasing pallor of the skin and mucous membranes, followed by cyanosis. The pupils are dilated and do not react to light. Possible bites of the tongue, lips, cheeks. The tonic convulsions phase lasts 30-60 seconds. In the second phase, tonic convulsions are replaced by clonic ones. Breathing is restored, becomes noisy, intermittent. Foam comes from the mouth, often stained with blood. Involuntary loss of urine, feces, and semen is possible. Consciousness is deeply darkened. The second phase lasts up to two to three minutes. In the third, phase of epileptic coma, muscle hypotonia, pathological reflexes, mydriasis, and lack of pupillary response to light are detected. Coma gradually gives way to stupor, followed by deep, sometimes prolonged sleep. After an attack, post-ictal disorders are often detected: signs of stunned consciousness, dysphoria, fatigue, headache, lethargy, drowsiness. Sometimes there are episodes of twilight stupefaction. There are no memories of seizures. Before a seizure, its precursors may be observed (they should not be identified with an aura). Several hours and even days before a seizure, disturbances in sleep, autonomic regulation, general sensitivity, appetite, sexual need, and mood (subdepression, hypomania, dysphoria) occur. Depressive mood swings with anxiety and fears can cause painful anticipation and fear of a seizure. Patients are also afraid of attacks, after which subjectively painful post-ictal disorders remain - headaches, depression, fatigue, memory impairment, impoverished speech (oligophasia), post-ictal twilight episodes. The combination of affective and painful precursors with the absence of post-seizure disorders may explain why some patients look forward to seizures as relief, what exactly makes seizures so desirable. Before primary and secondary generalized seizures, there is an increase in absence seizures and focal paroxysms, respectively.
Individual phases of a tonic-clonic seizure may be omitted. Such seizures are called abortive. These include tonic, clonic seizures and non-convulsive seizures of epileptic coma (atonic or syncope seizures). The latter may be mistakenly regarded as fainting. Infantile, childish spasm.
West syndrome or West syndrome, infantile spasm, infantile myoclonic encephalopathy with hypsarrhythmia is manifested by propulsive seizures: convulsions of the eastern greeting, lightning-fast shudders and attacks in the form of nodding and pecking. The convulsions of the eastern greeting (tik salaam) occur in series, usually during the day. During a seizure, the body slowly leans forward, the head drops down, and the arms move to the sides and forward. Lightning-fast shudders - there is a sudden and sharp shuddering of the whole body, the head falls down, the arms are moved to the sides. Nods and pecks - the head quickly falls down and after a few fractions of a second returns to its previous position. The spasm is often accompanied by screaming, crying, play of vasomotors, dilation of the pupils, trembling of the eyelids, and grimaces. In children older than 10 months, retropulsive seizures may also occur (the head leans back, the torso extends). Seizures occur mainly in the morning. Infantile spasms occur against the background of severe encephalopathy and have an unfavorable prognosis. At the age of three years, infantile spasms are replaced by seizures of a different type, and an increasing delay in intellectual and overall personal development is revealed. The prognosis is especially depressing in cases of combination of propulsive seizures with others - clonic, tonic-clonic. On the EEG, against the background of depression of the main activity, high-amplitude asynchronous slow activity, sharp waves and multiple peaks are detected.
Absence
(minor seizure). Manifested by a short-term loss of consciousness. Clinically, simple and complex absence seizures are distinguished.
Simple absence is a short – up to 20 seconds – loss of consciousness. May be accompanied by paleness of the face and slight trembling of the eyelids. In isolated form, it occurs only in children. In childhood, absence seizures can occur in series - pycnolepsy or pycnoepilepsy, Friedman's syndrome. Seizure statuses are possible. It is observed between the ages of 4 and 10-11 years. During seizures of pycnolepsy, slight movements in the backward direction are sometimes performed - retropulsive seizures. The prognosis is favorable. There is no delay in mental development, although in some cases, upon reaching puberty, seizures do not disappear, but are transformed into others. On the EEG, against the background of normal bioelectrical activity, peak-wave complexes appear with a frequency of 3 discharges per second, as is typical for simple (typical) absence seizures.
Complex absence seizure is a short, in some types of attacks up to 1 minute, loss of consciousness, accompanied by the appearance of other disorders: hyperkinesis, changes in postural tone, autonomic disorders, and individual actions. In accordance with this, there are many types of complex absence seizures. Let's briefly describe some of them. Myoclonic absence - loss of consciousness is combined with shudders of the whole body in a rhythm of 3 discharges per second or myoclonic twitching of individual muscle groups. Consciousness may sometimes not be lost. Atonic absence (seizures of rapid fall) - loss of consciousness is accompanied by loss of muscle tone of the entire skeletal muscle or in individual muscle groups. The decline in postural tone can be gradual (slow subsidence of the body) or jerky at a rhythm of 3 discharges per 1 second or so. Such seizures are accompanied by a longer loss of consciousness—up to 1 minute—and are mistakenly regarded as short fainting spells. Akinetic absence seizure is a seizure with immobility, which can also result in falls. Hypertensive absence seizure (absence with tonic symptoms) - during an attack, an increase in muscle tone, retropulsive, rotational movements, flexion and extension of the limbs, etc. are observed. Absence with vegetative disorders: loss of urine, hypersalivation, paleness or redness of the face, etc. Absence with short-term elementary automatisms - individual simple movements are performed, actions started before the seizure are continued or completed.
The type of disturbance of consciousness during absence is, apparently, not established - there is no information in the literature on this matter, usually only the fact of switching off consciousness is indicated. Clinical data indicate, in our opinion, that the disturbance of consciousness during an absence seizure can be variable and ranges from mild stupor (nubilation) to stupor (for example, absence seizures with loss of urine). Clinically, a taxonomy of absence seizures depending on the depth of loss of consciousness would obviously be justified.
Lennox-Gastaut syndrome (epilepsy with atypical absence seizures, myoclonic-astatic epilepsy). It manifests itself as atonic, tonic seizures and attacks of atypical absence seizures (triad of Lennox-Gastaut seizures). Observed between the ages of two and seven years, the disease is based on encephalopathy of unknown origin. Seizures (sudden falls, freezing, absences with automatisms, myoclonus) occur serially, lasting from a fraction of a second to 2 seconds. Delayed mental development, regressive symptoms (loss of previously acquired skills) are observed, and dementia is possible. The EEG picture is heterogeneous. After seven or eight years, the mentioned triad of seizures is replaced by generalized and complex partial seizures. Considered within the framework of secondary generalized epilepsy.
Propulsive epilepsy of Janz (myoclonic epilepsy of adolescents and young men). It is characterized by massive bilateral myoclonus (mainly in the muscles of the arms and shoulder girdle), primary generalized tonic-clonic seizures (sometimes secondary generalized, following myoclonus) and absence seizures, including complex ones. It is differentiated from Unferricht-Lundborg myoclonus epilepsy. Progressive familial myoclonus-epilepsy of Unferricht-Lundborg is characterized by a consistent complication of the clinical structure: nocturnal tonic-clonic seizures are joined by myoclonus after a number of years, then personality changes (intrusiveness, explosiveness, demandingness), and then muscle rigidity and dementia occur. Myoclonus is asymmetrical, irregular, disappears during sleep, intensifies with excitement and sensory stimulation, and its intensity varies from one day to the next. On the EEG, against the background of the absence of alpha rhythm, short paroxysms of sharp, slow waves, peak-wave complexes, symmetrical in both hemispheres, are recorded. Janz epilepsy is usually observed between the ages of 12 and 18 years. It's going well. There is no mental retardation, but a delay in personal development is possible - infantilism. The EEG shows spike-wave complexes of 3 per 1 second (typical absences), 1-2 per 1 second (atypical absences), polyspikes with a frequency of 4-6 per 1 second and subsequent slow waves are characteristic. With age, myoclonic paroxysms disappear.
Rolandic epilepsy. It manifests itself as pharyngeal seizures (swallowing, chewing, licking, hypersalivation in combination with paresthesia in the throat and tongue, a feeling of suffocation), as well as unilateral facial seizures. It is observed between the ages of 4 and 10 years. Seizures are rare, secondary generalization is possible, and often occur during sleep. The prognosis is favorable, the development of children is not impaired. On the EEG, against the background of preserved basic rhythms, peaks and high-amplitude sharp waves of central temporal localization are noted. Refers to focal epilepsy.
Landau-Kleffner syndrome. The typical onset of the disorder is between the ages of three and seven years. After a period of normal speech development, there is a gradual or very rapid loss of both receptive and expressive language skills. Some children become mute, others are limited to slang-like sounds, fluency of speech, articulation, and prosodic aspects of speech are impaired. At the same time, paroxysmal deviations in the EEG (in the temporal and other parts) and epileptic seizures are detected. The onset of seizures may precede speech disorders.
Rett syndrome. Begins between 7 and 24 months of age and has been described in girls. A period of normal early development is followed by partial or complete loss of manual skills, slowing of head growth, loss of intentional hand movements, handwriting stereotypies, and shortness of breath. Social and play development is delayed in the first two or three years, although social interests are partially preserved. In middle childhood, trunk ataxia, apraxia, kypho- or scoliosis, and sometimes choreiform hyperkinesis occur. Epileptic seizures are often observed in early and middle childhood, resulting in severe mental disability.
Riley-Day disease. Convulsive syndrome is combined with dry mucous membranes, paroxysms of hyperthermia, and the absence of fungiform papillae on the tongue. Occurs in patients of Jewish nationality. Epileptic foci of primary generalized seizures are localized in the brain stem.
Partial or focal seizures.
They manifest themselves as paroxysms of isolated disturbances of any functions - motor, sensory, autonomic, mental. In this case, stunned consciousness or confusion may occur, that is, complex focal seizures occur. The following types of seizures are classified as partial. Bravais-Jackson somatomotor seizures - paroxysms of clonic convulsions are observed in the muscles of the limbs and face on one half of the body. Clonic jerks most often occur in the orofacial muscles. Convulsions spread in different sequences. With their transition to the face, generalization of the attack into a general seizure is possible. Adversive seizures are a tonic convulsion with a rotation of the eyes, head and torso in the direction opposite to the localization of the epileptic focus. As a rule, it is accompanied by secondary generalization of the attack. Oculoclonic seizures are clonic abduction of the eyeballs (epileptic nystagmus). Oculotonic seizures are tonic abduction of the eyeballs (epileptic gaze convulsions). Version seizures are rotation of the body around its own axis. Somatosensory seizures are paroxysms of paresthesia on half the face and limbs opposite to the lateralization of the epileptic focus. More often they generalize into a general seizure. Speech or phonatory seizures are paroxysms of speech disorders (pronunciation of individual words, phrases, sometimes meaningful, their iterative repetition, sudden loss of speech) and phonation. Sensory seizures are paroxysms of elementary or simple hallucinations (auditory, visual, tactile, olfactory, gustatory, vestibular) and senestopathic sensations. For the most part, generalization occurs into a general seizure. Somatosensory Jacksonian seizures are attacks of paresthesia on half of the body on the side opposite to the localization of the epileptic focus (postcentral gyrus). Autonomic seizures of isolated autonomic disorders (severe pain in the epigastrium, abdomen, heart area - “abdominal epilepsy”; “epileptic angina pectoris”; breathing disorders - “epileptic asthma”; dysuric disorders, vegetative-vascular disorders), observed when the epileptic focus is localized in cortical parts of the temporal lobe of the brain (orbitoinsulotemporal region). Autonomic seizures can only manifest as dilated pupils - “pupillary epilepsy.” Abdominal and epigastric seizures are more common in children aged three to seven years. They are accompanied by a deafening of consciousness, which makes memories of them unclear. General vegetative paroxysms, combined with stunned consciousness and tonic convulsions - diencephalic epilepsy - are distinguished from cortico-visceral vegetative seizures. It is not mentioned in modern classifications.
In addition to the above, focal seizures with various psychopathological phenomena (“mental equivalents”, “paroxysmal epileptic psychoses”, “mental epileptic seizures”) are observed. The epileptic focus is most often found in the temporal lobes of the brain - “temporal lobe epilepsy.” Epilepsy, manifested by isolated mental equivalents, is also referred to as “larved” or “masked” epilepsy. The question of the differences that exist between mental seizures and acute psychoses in epilepsy is not very clear - where is the border separating them from each other, or at least what is the duration of the seizure itself. If we accept that the cycle of a generalized seizure (precursors - attack - post-seizure disorders) lasts up to 6-7 days, then we must agree that the duration of mental paroxysm can fluctuate within the same limits. We use the term “mental equivalents” not in its original meaning, but in a conventional sense and rather out of habit.
Various clinical variants of mental equivalents are observed: attacks of stupefaction, psychomotor seizures, paroxysms with affective, delusional, hallucinatory and ideational disorders, as well as special states of consciousness.
Attacks of clouding of consciousness are manifested by twilight, oneiric and delirious paroxysms. Twilight states (see “Disturbances of consciousness”). Attacks of epileptic delirium develop and end suddenly, accompanied by more extensive amnesia than usual. Seizures of epileptic oneioid also occur suddenly, without the change in individual stages of development established for schizophrenia. An ecstatic state, hallucinations of mystical content, stupor, detachment from reality or its illusory perception, in tune with the mood, are observed.
Psychomotor seizures are characterized by aimlessly performed actions, the nature of which is determined by the depth of the disturbance of consciousness and the immediate environment in which the patient is at this time. Depending on the degree of complexity and type of actions performed, the following types of psychomotor seizures are distinguished.
Fugues are attacks of rapid flight, rotation around the axis of the body or running in a circle (so-called manege actions), lasting for several seconds.
Outpatient automatisms - attacks with automatisms of walking. Patients wander around the city, go to unfamiliar places, and when they wake up, they do not remember where they were or how they got here.
Trances are multi-day attacks during which patients travel long distances using modern types of transportation. Patients attract the attention of others, perhaps only by increased drowsiness, taciturnity, absent-mindedness, as if immersed in some kind of reflection, but in general, external behavior remains orderly. It seems that in trances ancient, in Jung's terminology, archetypal nomadic complexes are released.
Gesture automatisms are short-term seizures during which patients perform isolated and incorrect actions: rubbing their hands, moving furniture from place to place, taking contents out of pockets or putting everything that comes to hand there, undressing, pouring water on themselves, urinating in plain sight. everyone has. Thus, one of the patients, a pathologist by profession, broke instruments and cut telephone wires during seizures. During the autopsy of the corpse, he separated pieces of tissue and ate them. He opened the car doors and tried to get out at full speed.
Speech automatisms - phrases, monologues, curses are pronounced, poetry is recited. Seizures with speech automatisms are similar to partial speech seizures; it is hardly possible to differentiate them clinically, as are some other psychomotor and motor seizures.
Automatisms of expressive actions - during a seizure there is senseless, wild laughter (“fits of crazy laughter” by Jackson), sobs, screams, singing, dancing, grimacing, poses expressing joy, fear.
Complex automatisms are seizures during which complex, seemingly meaningful and appropriate actions are performed. There are reports according to which patients during such attacks are able to perform complex work and even creative work: create a work of art, pass an important exam, solve a mathematical problem, etc.
Along with the above, paroxysms of affective disorders may occur: dysphoria, manic and depressive states. Dysphoria is attacks of melancholy and angry mood against the background of clear consciousness. Mania and depression, also occurring paroxysmally, resemble circular affective shifts. For epileptic mania, ecstatically enthusiastic elation is more characteristic, for depression - a gloomy shade of mood and the possibility of the appearance of impulsive desires.
Special states of consciousness (similar paroxysms are described under other names: psychosensory seizures, dream-like states, temporal pseudoabsences) differ from absence seizures in their relatively slow onset and termination, longer duration (minutes, tens of minutes), and the presence of various psychopathological symptoms. The phenomena of autometamorphopsia (macrosomia, microsomia, etc.), metamorphopsia (macropsia, micropsia, porropsia, etc.), disturbances in the perception of time, derealization, the phenomena of “already seen, heard, experienced” and “never seen, heard, experienced” are observed. ", disturbances in the perception of color quality, isolated hallucinations, fragments of fantastic dream-like delirium, fear, melancholy, confusion, massive vegetative disorders. During the attack and after it, an understanding of the painfulness of the condition remains. Memories of subjective experiences of this period are quite complete, but memories of external events are fragmentary or absent. Amnesia is possible for part (at the beginning, in the middle, at the end) of the attack, which is associated with stunned consciousness. In this case, the seizure, according to currently accepted terminology, is designated as a complex partial seizure. Attention should be paid to the fact that in their reports patients sometimes only mention “outages,” which can create a false impression. absence seizure Complex partial seizures differ from absence seizures in their structural complexity, duration (several minutes, up to 10 or more), and the absence of typical discharges on the EEG - three peak-wave complexes per second.
Ideation seizures are attacks of violent flow or stopping of thoughts and memories. Amnestic seizures reflect limbic disorders and are manifested by short episodes of loss of memory for past events. Ecmnestic seizures are hallucinatory, violent memories of the real past.
Temporal seizures can occur in isolation, but their secondary generalization into a major attack is possible, after which the psychosis is self-limited. With high convulsive readiness, very rapid generalization occurs, the psychotic episode does not last long and, as already mentioned, is the aura of a seizure.
The above list probably does not exhaust the variety of mental attacks. In addition, it shows that there is no satisfactory classification. The taxonomy of mental seizures, according to the literature, is based on psychological criteria and is mostly carried out from the position of structuralist psychology. This implies both the terminology (“cognitive”, “emotional” seizures, seizures with disturbances of perception, etc.), as well as the inevitable difficulties with this approach in distinguishing between different paroxysms and the static nature of assessments. Modern psychopathology in the taxonomy of mental disorders uses a syndromic, that is, clinical-pathogenetic approach. It does not appear to have been applied to mental attacks. The resulting idea is that mental seizures can be classified according to the severity scale of productive mental disorders. Thus, it becomes possible to arrange seizures depending on the depth of damage to mental activity, to establish hierarchical relationships between them; perhaps identify yet unaccounted for types of paroxysms, or even suggest their existence; determine the severity and direction of the course of temporal lobe epilepsy, the effectiveness of drug therapy, based not only on quantitative criteria (frequency), but also on an analysis of the clinical structure of paroxysms; in cases of gradual development of an attack, evaluate the stages and “march” of pathological conditions that change during the attack.
Partial seizures with mental pathology, if you follow the syndromic principle, can be located in the following sequence (presentation is in order of increasing severity):
1. Seizures with symptoms of a psychosomatic level: disturbances of sleep, desires, general sensitivity, activity, autonomic regulation. These are seizures with episodes of drowsiness, reminiscent of narcoleptic paroxysms, attacks of epileptic dreams, paroxysms of sleepwalking and sleep-talking. Further, these are cortical vegetative paroxysms, seizures with various disorders of general sensitivity, in particular, senestopathies, drives (bulimia, increased libido).
2. Seizures with affective pathology - dysphoria, manioform and depressive paroxysms.
3. Seizures with symptoms of a neurotic level: depersonalization and derealization, mental anesthesia, obsessive, hysterical phenomena. Hysterical seizures can probably be actually epileptic, and in this case it is not advisable to distinguish them from seizures of epilepsy. Another thing is their difference from convulsive seizures. Hysteriform paroxysms in patients with epilepsy differ from actual hysterical (neurotic) seizures in greater severity: the absence of photoreaction of the pupils - Redlich's symptom, less contact between patients, and decreased responsiveness to external influences. It is more difficult to modify and abort the seizure. There may be biting of the cheeks, loss of urine, minor bruises, seizures are more stereotypical, last longer and leave behind fewer memories. Hysteriform seizures can also be combined with tonic-clonic ones or develop into the latter. Classic differential diagnostic tables of signs distinguishing hysterical and epileptic seizures seem to be built on a comparison of different classes of phenomena, and therefore have rather academic significance. As for hysteriform seizures in patients with epilepsy, they have been known for a long time and are described under different names (subcortical, intermediate, hysteroepileptic, severe hysterical seizures). The main difficulty in differential diagnosis is that they are phenomenologically similar to functional seizures.
4. Seizures with delusional-hallucinatory symptoms - delusional, hallucinatory, paranoid, hallucinatory-paranoid, paraphrenic. Perhaps there are epileptic paroxysms with catatonic symptoms.
5. Seizures with disturbances (confusion) of consciousness: oneiroid, delirium, twilight stupefaction, motor, expressive automatisms (fugues, trances, ambulatory automatisms).
Along with seizures, during which productive psychopathological symptoms occur, paroxysms with negative symptoms are observed. These are, for example, seizures with stunning seizures (absences, complex partial seizures), stupor and coma (non-convulsive seizures), amnestic seizures, and Sperrung-type seizures. This probably does not exhaust all the variants of “negative” epileptic paroxysms.
What is the diagnosis of generalized epilepsy?
Generalized epilepsy is diagnosed by a doctor based on:
- careful collection of anamnesis (including information about the presence of the disease in the family, the age of the patient at which the first attack was observed, the duration and nature of the attack, the presence of seizures)
- laboratory testing of blood and urine
- echoencephalography (including EEG monitoring)
Additionally, to clarify the diagnosis, you may need:
- CT
- NMRI
- biochemical examination of blood and cerebrospinal fluid
- consultations with other specialists (neurosurgeon, infectious disease specialist, pediatric ophthalmologist)
Introduction
The rapid development of neuropharmacology in recent decades, the synthesis of new highly effective antiepileptic drugs (AEDs), a radical revision of many principles of treatment of epilepsy, has now made it possible to classify epilepsy as a curable disease. According to generalized data from the leading antiepileptic centers in the world, a pronounced therapeutic effect is achieved in 75-85% of patients suffering from epilepsy. Epilepsy is one of the most pressing problems in pediatric neurology. According to foreign data, the frequency of epilepsy in the pediatric population is 0.5-0.75% of the child population, and febrile seizures up to 5%. There are no exact statistics on this disease in Russia. Firstly, not all doctors are widely familiar with the modern International Classification of Epilepsy. In this regard, the statistics of epilepsy did not include such diagnoses as “epileptiform syndrome”, “convulsive syndrome”, which are not used in any country in the world and, in fact, are the same disease - epilepsy. Secondly, in our country, epileptic people are observed by both neurologists and psychiatrists, which significantly distorts the statistics. In all countries of the world, epilepsy is a neurological disease.
Over the past decade, there has been a very rapid accumulation of new knowledge on the problem of epilepsy. Both experimental and clinical studies have contributed to a better understanding of the underlying pathophysiological mechanisms of the disease. New research methods have significantly changed our ability to diagnose epilepsy and identify etiological factors of the disease. In addition, great advances have been made in the development of medical and surgical treatment approaches.
What is the treatment for generalized epilepsy
Effective treatment of this type of epilepsy directly depends on the form of the disease, as well as the nature of the attacks. And if it does not always allow the patient to forget about his illness, ideally it should be aimed at maximizing the reduction in the frequency and severity of attacks.
Anticonvulsant therapy for generalized epilepsy is usually recommended to begin no earlier than the second attack and only if an accurate diagnosis has been established. It is usually started by prescribing a base drug specifically for this epiform (for example, valproate, etc.), starting with a dose that is approximately a quarter of the standard therapeutic dose. Over the next two to three weeks (with the indispensable condition of good tolerability and the absence of a therapeutic effect), the starting dose is increased by another half, further bringing it to the average therapeutic dose. Such monotherapy is usually quite effective in the case of idiopathic generalized epilepsy.
If no positive dynamics are observed as a result of treatment, or the condition is worsened by various side effects, the doctor may replace the drug with another one. Therapy can be considered successful when complete remission occurs (without attacks) within three years from the start of treatment, after which a dosage reduction is possible.
Generalized epilepsy today is not a death sentence for the patient, because a timely correct diagnosis and effective therapy allows the patient to significantly improve the quality of his life already in the first stages of treatment. Are you or your loved ones concerned about this disease? Experienced medical specialists are always ready to provide you with the necessary assistance and give you the opportunity to look into the future with confidence!
Idiopathic partial epilepsy with occipital paroxysms.
Idiopathic partial epilepsy with occipital paroxysms - benign occipital epilepsy (BOE) - is a form of idiopathic localization-related epilepsy of childhood, characterized by simple partial seizures with visual disturbances and the presence of specific peak-wave activity in the occipital leads on the EEG. The disease begins at the age of 2-12 years with two peaks of onset - around 3 and 9 years. Simple partial sensory paroxysms with visual disturbances are typical. Characteristic are simple visual hallucinations, photopsia, visual illusions (macro-, micropsia). Transient amaurosis and homonymous quadrant hemianopsia may occur. During an attack, a versive component with forced turning of the eyes and head is often observed. A focus in the occipital lobe often radiates excitation anteriorly (to the temporal and frontal lobe) with the appearance of complex structural hallucinations; switching off consciousness and the occurrence of secondary generalized convulsive attacks. Typically, attacks occur during sleep, especially when patients awaken. Attacks are often accompanied by migraine symptoms: headache and vomiting. The first attacks in young children are the most severe and lasting (up to several hours or even days). The EEG determines the appearance of high-amplitude peak-wave activity in one of the occipital leads or bioccipital leads independently. The morphology of the patterns resembles that of rolandic epilepsy. Characteristic is the disappearance of epiactivity when recording EEG with eyes open. Differential diagnosis. It should be differentiated, first of all, from symptomatic occipital epilepsy, which occurs with structural damage to the occipital lobes. With symptomatic occipital epilepsy, the age of onset of seizures is not limited; complex partial and secondary generalized seizures are more often observed. The morphology of peak-wave complexes on the EEG is different than in idiopathic occipital epilepsy, and it does not change with eye opening. Neuroradiological examination reveals morphological changes in the occipital lobes of the brain. The prognosis is less favorable. Treatment. The drugs of choice are carbamazepine derivatives. The average daily dose is about 20 mg/kg. If ineffective, valproate is used - 30-50 mg/kg/day. Reserve drug phenytoin – 3-7 mg/kg/day. Treatment is carried out only with monotherapy. Resistant cases must be differentiated from symptomatic occipital epilepsy. Complete therapeutic remission is observed in 95% of cases. At the same time, attacks are more difficult to stop and the doses of AEDs are higher than for rolandic epilepsy.
part-1 part-2