Causes
Physiological factors
Burning usually occurs in people with sensitive skin, even in the absence of a pathological factor. An unpleasant symptom is provoked by wearing itchy clothing or things made of synthetic materials. Women may experience a burning sensation on their face after applying skincare or decorative cosmetics, even if these products do not cause allergies. A typical cause of tingling and burning sensations on the skin of the legs is fatigue after a long walk.
Burns
Most often, symptoms are caused by exposure to high temperature or solar radiation. Any burn is accompanied by a severe burning sensation of the skin, which begins even during the action of the damaging factor and lasts from several days to several weeks. The skin appears pink or bright red in color; with deeper lesions, blisters filled with clear or cloudy contents form.
A burning sensation constantly bothers a person. The symptom becomes more noticeable when touching the affected area, applying medicinal ointments and sprays. The discomfort is greatly aggravated if the burn area comes under warm or hot water (for example, when swimming). As healing progresses, the burning sensation subsides and is replaced by periodic tingling and itching of the skin.
Chemical and electrical burns are characterized by deep penetration of the damaging agent - right up to the hypodermis, muscles and underlying tissues. With such injuries, burning fades into the background, since the main complaint is unbearable pain in the area of the destroyed epidermis and dermis. Burning sensations in the skin occur immediately at the moment of injury, when massive tissue destruction has not yet occurred.
Burning skin
Allergy
Skin hypersensitivity reaction is the second most common cause of burning skin. The symptom is determined in predisposed people upon contact with allergens: plant pollen, cosmetics, animal hair, food. Allergic burning is combined with urticaria, itchy skin rashes in the form of papules and vesicles. Watery eyes, sneezing, and discharge of clear mucus from the nose are often associated.
A burning sensation can be one of the components of seasonal allergies (hay fever). Sometimes this symptom becomes a harbinger of an attack of bronchial asthma: in this case, unpleasant manifestations are localized in a limited area and are accompanied by the presence of red spots on the skin. Often, burning sensations accompany pseudo-allergies when taking histamine liberators (chocolate, citrus fruits, strawberries).
Contact dermatitis
Burning skin is typical of the acute erythematous form of contact dermatitis, provoked by exposure to an irritant. The patient experiences painful and burning sensations, tingling, itching in the affected area. The skin takes on a bright red tint. In the bullous version of the disease, the burning sensation is complemented by the formation of blisters filled with clear liquid. Insignificant severity of the symptom occurs in the chronic form of dermatitis.
Psoriasis
Moderate itching and burning of the skin develops with the exudative form of the disease, which is manifested by the formation of scales and pronounced weeping. A burning sensation in the affected areas is disturbing during exacerbation of psoriasis. Symptoms intensify when scratching damaged skin or bathing. As a rule, the exudative process is detected in those suffering from endocrine pathologies (diabetes mellitus, hypothyroidism).
Herpes
Painful symptoms with apparently intact skin are characteristic of herpes zoster. Patients complain that the skin constantly burns, in order to reduce discomfort, they want to scratch it. Unpleasant sensations arise suddenly, last 12-24 hours, then specific vesicular rashes form at this site. In this case, severe burning pain persists until recovery, and can bother a person for a long time after the rash disappears.
With herpes simplex, the burning sensation of the skin is not so intense. Symptoms develop simultaneously with the appearance of vesicles filled with clear exudate. Patients note itching and an unpleasant tingling sensation in the affected area. The pain is moderate, unlike shingles. The burning stops when the rash heals and disappears.
Skin infections
Burning is one of the main symptoms of bacterial (impetigo, erysipelas), viral (molluscum contagiosum, HPV) or fungal (dermatophytosis, rubromycosis) skin lesions. Taking into account the etiology of the disease, burning sensations are accompanied by various local symptoms: vesicular and pustular rashes, peeling, lichenification.
Senestopathies
Pathology is observed in mental disorders: Kandinsky-Clerambault syndrome, hysterical neurosis, bipolar psychosis. Patients feel an intense burning sensation, sometimes feeling as if the whole body is “burning.” To cope with painful symptoms, the patient constantly scratches the skin and tries to apply ice. In some cases, the burning is so intense that the person rushes around the room, screaming or moaning.
Complications of pharmacotherapy
A burning sensation of the skin occurs with drug-induced dermatitis. Unpleasant symptoms develop both when drugs are applied externally (ointments, gels) and when drugs are administered orally or parenterally. Areas of rash or weeping form on the skin, which are accompanied by an unpleasant burning sensation. With each subsequent use of allergenic drugs, the affected area increases.
Rare causes
- Congenital diseases
: Hartnup disease, porphyria. - Connective tissue damage
: scleroderma, systemic lupus erythematosus, Shulman's disease. - Vascular disorders
: rosacea, rosacea, obliterating atherosclerosis. - Malignant neoplasms
: squamous cell skin cancer, basal cell carcinoma, melanoma.
Associated symptoms
This symptom manifests itself in different ways. The tip of the tongue often burns, but sometimes the entire tongue or just the base burns. Often, with a burning sensation in the mouth, other accompanying symptoms are also noted. These include sore throat, dry mouth, difficulty swallowing, the appearance of white spots on the tongue, and others. The patient may also experience tingling, tingling, or rawness in the mouth. The nature of pain can be acute or chronic. If a symptom bothers you irregularly, then it is important to understand under what circumstances it develops. For example, if your tongue begins to burn whenever you eat pineapples, mangoes or other allergenic foods, then the cause is most likely food.
Diagnostics
A specialist in the field of dermatology will determine the cause of the symptom; if necessary, doctors of other specialties will be involved in the examination. The dermatologist conducts a visual examination of the areas of the skin where the patient feels a burning sensation, after which he takes material for laboratory tests. Diagnostic search includes the following research methods:
- Dermatoscopy.
Under a microscope, the doctor examines the structures of the skin and identifies the initial stages of pathological changes. This is a simple and non-invasive method, which is indicated if the patient has a burning sensation in the area of new growths or suspiciously changed areas of the skin. - Luminescent diagnostics.
Inspection of the affected area using a Wood's paw allows you to quickly confirm ringworm, pityriasis versicolor, and erythrasma. The technique is used for rapid diagnosis of pseudomonas infection and acne. - Scraping examination.
The upper layer of the epidermis from the affected area is taken for microscopic examination. This method is informative in the diagnosis of fungal and bacterial infections. If a dermatologist needs to clarify the nature of the pathological process, a histological examination of a skin biopsy is prescribed. - Blood tests
. A clinical test is performed to detect signs of inflammatory or autoimmune diseases. An increase in eosinophils in the hemogram indicates the allergic nature of the burning sensation. To assess the activity of dermatological diseases, a biochemical analysis with acute phase indicators and a proteinogram is prescribed.
During the period of remission of allergic dermatoses, prick tests are recommended to determine provoking factors and select ASIT. If there is a burning sensation in the lower extremities in elderly patients, duplex scanning of the peripheral arteries and arteriography must be performed. If complaints of burning skin are combined with inappropriate behavior of the patient, a psychiatric examination is prescribed.
Dressing for skin burns
How to avoid burning skin: tips
To avoid skin burning, it is not necessary to use pharmaceutical preparations. To do this, you can follow some rules:
- Wear comfortable cotton clothing that will not irritate your skin. If you still have a burning sensation because you often feel stressed or nervous, then you need to take antihistamines, as well as sedatives.
- It is worth constantly monitoring what you are doing. Do not scratch your skin under any circumstances. Because this will cause the connection of a secondary bacterial infection.
- During bright sunshine and hot weather, try to avoid going outside, or wear clothes that will protect you from the sun's rays.
- Be sure to wear comfortable shoes. If the burning sensation is associated with vascular diseases, tight shoes can provoke an exacerbation of ailments.
The skin bakes
We do not recommend self-medication. Only a qualified specialist can choose the right drug.
Treatment
Help before diagnosis
If the burning sensation is caused by a slight burn of the skin (only redness, no blisters), it can be treated with dexpanthenol sprays. Medicines quickly relieve symptoms, soothe the skin and promote its healing. If you experience severe burns, rashes or other symptoms, consult a doctor. To quickly relieve burning sensations, experts prescribe gels and sprays with a soothing and cooling effect.
Conservative therapy
Therapy is determined by the underlying disease. Often, burning skin is caused by dermatological pathologies, to eliminate which an integrated approach is practiced. For mild cases of the disease, local remedies are sufficient: lotions and wet-dry dressings for weeping, ointments and rich creams for peeling. They use medications with antiseptics and antibiotics, topical steroids, and antimycotics.
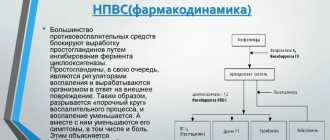
For allergic dermatoses, systemic detoxification therapy is prescribed: antihistamines, sedatives, methods of extracorporeal hemocorrection. Antifungal drugs in tablets are recommended for the treatment of common mycoses. Herpes zoster requires intravenous or oral acyclovir.
Physiotherapy methods are effective in a comprehensive treatment regimen. To eliminate rashes, accelerate skin healing and stimulate immune defense, laser therapy, magnetic therapy, and ozone therapy are prescribed. In the remission phase of chronic dermatoses, skin irradiation with ultraviolet light and mud therapy are used. With senestopathies, patients require the help of a psychiatrist.
Folk remedies for burning skin: recipes
The simplest antihistamines, like Fenistil, are absolutely safe to use. Perhaps you were bitten by an insect and you simply didn’t notice. In this case, the ointment will help, the itching will go away within a short period of time. You can cope with the means that our grandmothers used.
Traditional recipes:
- Butter and onion. You need to boil 250 ml of vegetable oil and immerse 6 chopped small onions in it, wait until they turn brown and strain. After this, add a spoonful of finely grated beeswax, boil for 5 minutes over low heat, strain again, cool and store in the refrigerator. The product in the form of an application is applied directly to the area that burns.
- Melissa relieves burning sensation well . This fragrant herb can be used both internally and externally. For oral administration, just add a pinch of lemon balm to a cup of regular tea.
- Dill . Pour 10 g of seeds into a glass, pour boiling water over them, let it brew, then strain. Take 120 ml three times a day.
Burning in the back area
Preventive measures
Preventive measures against a “burning” tongue include the following:
- Proper dental and oral hygiene.
- Clean your tongue daily with a special cleaner (but not with a brush!).
- Compliance with drinking regime.
- Avoiding allergens, in particular food ones.
- Controlling blood sugar levels.
- Timely treatment of the gastrointestinal tract.
- Compliance with the principles of balanced nutrition.
- Regular preventive examinations with a dentist (at least 2 times a year).
Burning in the left side of the chest
According to medicine, there may be a stove there due to many reasons. It may become hot due to dysfunction of the pancreas - with this pathology, the burning sensation is limited to the left hypochondrium. Inflammation of the duodenum also manifests itself with similar symptoms. A burning sensation in the chest on the left is also a symptom of a stomach ulcer or gastritis. Separately, it is worth mentioning such a pathology as acute pancreatitis - this disease is quite capable of triggering an intolerable syndrome and leading to peritonitis.
From the editor: Is it possible to drink alcohol after a stroke?
Burning sensation in the left sternum in women
Hormonal imbalance in the weaker sex often manifests itself in negative conditions. Tingling and burning in the left sternum in women often indicate latently developing mastopathy of the mammary glands. Many ladies experience severe discomfort before menstrual bleeding, which is regarded as a completely natural condition. Women often experience a burning sensation in their chests due to hormonal changes. Ladies during menopause are especially sensitive to this kind of manifestation.
Pathogenesis
The burning sensation is accompanied by irritation and injury to the mucous membranes due to increased acidity of gastric juice, peptic enzyme activity and the formation of ulcers. It can “burn with fire” when a person is very hungry and acidic gastric juice reaches erosive areas.
Irritation of the mucous membranes can occur not only due to acidic gastric contents, but in more rare cases it is caused by alkaline reflux . In this case, the mucous membranes are exposed to the action of bile acids , which enter the stomach through the duodenogastric reverse flow of bile.
The pathological process begins with an imbalance in the ratio of “aggressive” and “protective” factors of the digestive system. The main aggressive effect is to increase the activity of proteolytic enzymes and the level of acidity secreted by gastric juice, along with a deterioration in the motility of the digestive organs. Protective properties are reduced if:
- less mucus is produced;
- the processes of natural physiological regeneration of the epithelial surface slow down;
- local blood circulation, innervation and trophism are disrupted.
For example, this can occur under conditions of prolonged or repeated psycho-emotional stress against a background of negative emotions.
A separate predisposing factor, along with heredity and family history, are deficiencies in diet and nutrition, smoking and alcohol abuse.
The pathological process is based on proteolytic destruction of tissue by gastric juice in an area with deteriorated trophism, which is most often observed in the lower parts of the stomach. A decrease in the alkaline component and prolonged contact with acidic gastric juice is possible with spasm of the gastric sphincter - the pylorus. In addition, the level of mucin contained in mucus, the state of the apical membranes of enterocytes, and nervous and vascular trophism are important .
When the mucous barrier and the protein-lipid complex of the apical membranes are destroyed, reverse diffusion of hydrogen ions into the cell membranes occurs, which activates the kinin-kallikrein inflammatory system and increases the permeability of the capillary network. This leads to microcirculation disorder, then lipid peroxidation products as a result of oxidative degradation of lipids under the influence of free radicals, damaging lysosomes.
The negative neuro-emotional effect on the gastrointestinal tract is carried out through the anterior parts of the hypothalamus , along the path of the vagus nerve, acetylcholine, histamine and gastrin receptors in glandular tissues. The formation of acid and the proteolytic activity of the gastric glands increases under the influence of thyroid-stimulating and adrenocorticotropic hormone - the glucocorticoid effect of the adrenal glands increases and the mineralcorticoid effect of the adrenal glands decreases, the production of hydrochloric acid is stimulated and the protective and reparative properties of the mucous membranes of the stomach and intestinal tract are reduced.
Local protective mechanisms are implemented by mucoid cells that produce glycoproteins , sialoproteins and fucopolyproteins , as well as mucus coming from the oral cavity. It is alkaline and can neutralize hydrochloric acid (HCl). In general, the gastrointestinal tract is a very vulnerable system of the body, but it has good regenerative abilities.
When to see a doctor
If this is not the first time a burning sensation in the mouth has occurred, and the culprit is NOT spicy food, then this is a reason to consult a doctor. Based on the above reasons, doctors of various specialties can deal with this problem. First of all, these are therapists. A general practitioner, based on the history taken, will be able to exclude a number of pathologies and refer the patient to the right specialist. Among them are dentists, endocrinologists, infectious disease specialists, gastroenterologists and others.
Important! During the interview, the doctor should tell you about all concomitant diseases, lifestyle and medications you are taking. This information will help the doctor rule out a number of diseases and quickly identify the cause of the symptom.