Features of the disease
In medical practice, epilepsy is a complex neurological disease accompanied by sudden seizures and seizures. The disease is characterized by the fact that during an attack a person does not realize what is happening to him. As a result, patients do not remember the seizures, do not understand the degree of their intensity and are not able to describe what happened to them.
Temporal lobe epilepsy is one of the most common forms of the disease. This type of disease is accompanied by partial epileptic seizures of varying severity. The progression of pathology in the absence of adequate therapy threatens the occurrence of generalized seizures, as well as the development of various mental disorders and deformations.
There is also a classification of temporal lobe epilepsy, according to which there are 4 types of pathology, depending on the location of the epileptic focus:
- amygdala;
- hippocampal;
- lateral;
- opercular.
Epilepsy with myoclonic-astatic seizures.
Myoclonic-astatic epilepsy (MAE) is one of the forms of cryptogenic generalized epilepsy, characterized mainly by myoclonic and myoclonic-astatic seizures with onset in preschool age. The debut of MAE varies from 10 months. up to 5 years, averaging 2.3 years. In 80% of cases, the onset of attacks occurs within the age range of 1-3 years. In the vast majority of patients, the disease begins with GSP, followed by the addition of myoclonic and myoclonic-astatic seizures at the age of about 4 years. Clinical manifestations of MAE are polymorphic and include various types of seizures: myoclonic, myoclonic-astatic, typical absences, DBS with the possibility of partial paroxysms. The “core” of MAE are myoclonic and myoclonic-astatic seizures: short, lightning-fast twitches of small amplitude in the legs and arms; “nods” with slight propulsion of the body; “kicks to the knees.” The frequency of myoclonic attacks is high, especially in the morning after patients awaken. GSP is observed in almost all patients, absence seizures – in half. The addition of partial seizures is possible in 20% of cases. An EEG study is characterized by a slowdown in the main activity of the background recording with the appearance of generalized peak and polypeak wave activity with a frequency of 3 Hz. In most patients, regional changes are also observed: peak-wave and slow-wave activity. Treatment begins with monotherapy with valproic acid. Average doses are 50-70 mg/kg/day with a gradual increase to 100 mg/kg/day if there is no effect. In most cases, only polytherapy is effective: a combination of valproate with lamotrigine or benzodiazepines or succinimides. Seizure control is achieved in most patients, however, complete remission is possible only in 1/3 of cases. The addition of partial paroxysms significantly worsens the prognosis; These attacks are the most resistant to therapy. Transformation of MAE into Lennox-Gastaut syndrome is possible.
Causes of temporal lobe epilepsy
As is the case with other forms of the disease, the main reason for the development of temporal lobe epilepsy is the formation of an epileptic focus in the brain. In this case, the pathological area is a certain area of the temporal lobe. An epileptic seizure is triggered by a sudden surge of excessive neuronal activity in the temporal lobe of the brain.
Today, doctors identify a lot of factors that predispose to the development of temporal lobe epilepsy, dividing them into two broad groups:
- Perinatal - have a negative effect on the brain during intrauterine development or labor. The group of perinatal factors includes various forms of fetal hypoxia, injuries received during childbirth, infectious diseases suffered by the mother during pregnancy, asphyxia in newborns, etc.
- Postnatal – acquired factors of a postnatal nature are much more numerous and varied. Among the most common are traumatic brain injuries, consequences of ischemic or hemorrhagic stroke, brain tumors, abscesses, aneurysms and various neuroinfections).
Alpha Rhythm
Kirillovskikh O. N., neurologist-epileptologist, Ph.D.
Symptomatic temporal lobe epilepsy is a form of the disease in which the focus of epileptiform activity that triggers the seizure is located within the temporal lobe of the brain. The most common cause of the development of temporal lobe epilepsy is sclerosis of the median (medial) structures of the temporal lobe (ammon's horn, hippocampus) - the so-called mesial (medial) temporal sclerosis. This form of temporal lobe epilepsy is called mesial temporal lobe epilepsy . This is the most common type of epilepsy in children and adults, its prevalence reaches 25% among all forms of epilepsy, and among symptomatic forms of epilepsy, in which epileptic seizures are a manifestation of the so-called background disease (consequences of brain injuries, vascular diseases, etc.), is 60%.
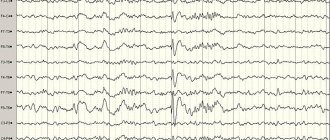
Rice. 1 Girl, 15 years old, right-handed, history of febrile convulsions, at the age of 12 - a nocturnal grand mal attack. Then attacks of déjà vu, freezing, decreased responses to stimuli, lip smacking, dystonic posture of the left hand, fiddling with the fingers of the right hand, and postictal confusion began to occur. MRI shows mesial temporal sclerosis on the right, EEG is normal.
Mesial temporal lobe epilepsy has 3 peak age of onset - at 6, 15 and, less often, at 27 years. The reasons for the development of this form of epilepsy are not fully understood. It is known that 15-30% of patients have ever, often long before the manifestation of typical epileptic seizures, experienced so-called febrile seizures, i.e. convulsive, similar to epileptic seizures, manifesting themselves against the background of high body temperature in children. In patients with hippocampal sclerosis detected by MRI, atypical febrile seizures were observed in 78% of cases. Febrile convulsions are usually observed in children under the age of 6 years, then a so-called “light interval” occurs, lasting from 2 to 7 years, during which there are no epileptic seizures, but mildly expressed intellectual disorders can be observed, i.e. memory and intelligence, and behavioral disorders. In such cases, the EEG may reveal individual epileptiform elements or regional epileptiform activity . In some cases, signs of pathology may be completely absent in the clinical picture and on the EEG. The light interval ends, as a rule, with the development of afebrile, that is, epileptic seizures not associated with a rise in temperature.
The onset of mesial temporal lobe epilepsy may be invisible to the patient and surrounding people, for example, if the disease begins with an isolated aura (a harbinger of an attack). The most typical are vegetative-visceral auras in the form of an “ascending epileptic sensation” - pain in the stomach, heartburn, nausea, rising to the throat with a feeling of a lump in the throat, reaching the head, causing a feeling of “lightheadedness”, weakness. The attacks occur first with preserved consciousness, then they can end with a short-term switching off of consciousness. Also, mesial temporal lobe epilepsy is characterized by auras with impaired mental functions, manifested by derealization and depersonalization - feelings of unreality and illusoryness of the environment. Objects seem to the patient to be endowed with a special meaning, a soul; they flash with a ray of light and bright colors, or, conversely, the world around them becomes dull, pale, joyless and frozen. Often these phenomena are combined with the states of “deja vu” and “jamais vu”: “previously seen (heard, experienced)” and “never seen (not heard, not experienced).” With the “previously seen” syndrome, the place where the patient is for the first time seems very familiar to him. With never-before-seen syndrome, a familiar environment becomes alien, frightening, and perceived as if it were the first time.
As the disease progresses, the isolated aura is replaced by complex partial attacks occurring with loss of consciousness. They are divided into dialeptic and automotor. Dialeptic seizures or temporal pseudoabsences are manifested by an isolated loss of consciousness without convulsions, a sudden stop of motor activity, “freezing”, “freezing” of patients; the eyes are wide open, the gaze expresses amazement or fear (“staring gaze”). This may cause paleness or redness of the face, dilated pupils, sweating, and palpitations. Automotor seizures are characterized by a similar clinical picture with the addition of involuntary movements - automatisms. Mesial temporal lobe epilepsy is characterized by oroalimentary automatisms - chewing, swallowing, sucking, licking with the tongue, spitting. Gesture automatisms are also common - fast stereotypical unilateral movements - patting, scratching, fingering or stroking clothes, clapping hands, rubbing hands together, washing movements with hands, etc. In addition to gestural automatisms, movements of the head and body may occur - marking time, rotating around its axis, squatting or getting up from a lying position.
Complex partial seizures may result in generalized seizures. Often, only a generalized seizure is the reason for visiting a doctor; isolated auras and even complex partial seizures are often ignored by patients and their relatives. Diagnosis of mesial temporal lobe epilepsy before the development of a generalized convulsive attack is difficult even for specialists - neurologists and epileptologists. This is due to the fact that this form of epilepsy does not have such characteristic EEG changes as, for example, most idiopathic, hereditary forms of the disease. Epileptic activity on the EEG in mesial temporal lobe epilepsy may be absent or only indirect conditional epileptiform elements may be recorded. Studying the bioelectrical activity of the brain during EEG sleep monitoring significantly increases the likelihood of diagnosing pathological epileptiform activity. However, for the correct interpretation of the sleep EEG in mesial temporal lobe epilepsy, a highly qualified neurologist is needed - an epileptologist who can evaluate the complex of clinical and EEG symptoms and establish the correct diagnosis.
Mesial temporal lobe epilepsy is the most difficult to treat form of epilepsy in adults and children over 12 years of age. The difficulties of drug therapy for this disease are due to the structural and functional characteristics of the neurons that make up the so-called old temporal cortex or mesial temporal complex - the hippocampus, amygdala, and parahippocampal gyrus. The neural network that forms these structures has an increased ability to generate pathological electrical activity, which is the cause of an epileptic seizure. Treatment of mesial temporal lobe epilepsy requires the administration of large doses of antiepileptic drugs; as a rule, there is a need for a combination of them. However, the effectiveness of drug therapy for symptomatic temporal lobe epilepsy is low. The proportion of patients achieving complete remission, i.e. absence of epileptic seizures for a long period ranges from 11 to 25% (of which 48% - when using monotherapy, 52% - when using polytherapy with several antiepileptic drugs simultaneously). A reduction in the frequency of attacks by a factor of two or more is observed in 60%. Absolute resistance to drug treatment, i.e. a complete lack of effect from treatment is recorded in 6-40% of patients according to the results of various studies. According to Panayiotopoulos (2005), for example, seizures can generally be controlled only in 25-42% of patients with temporal lobe epilepsy. Despite the use of more and more new forms of antiepileptic drugs, over time, mesial temporal lobe epilepsy becomes pharmacoresistant, the phenomenon of “escape” from therapy is observed - a new drug has only a temporary therapeutic effect, then seizures resume again. In addition, long-term mesial temporal lobe epilepsy causes the development of epileptic dementia (dementia) and disability in patients.
In this regard, along with drug therapy, various non-drug treatment methods, in particular neurosurgical ones, are used for the treatment of mesial temporal lobe epilepsy.
Neurosurgical treatment of mesial temporal lobe epilepsy includes 2 main types of intervention - anterior temporal lobectomy with resection of the mesial structures of the temporal lobe and selective amygdalohippocampectomy. Neurosurgical treatment is indicated for patients with an established pharmacoresistance factor, confirmed by high-resolution MRI with unilateral mesial temporal sclerosis and with a short duration of the disease. The operation is preceded by a thorough preoperative examination; in most cases, out of 10 candidates, no more than 2 are selected. Such careful selection is likely responsible for good results of neurosurgical treatment - complete remission of attacks occurs, according to the Bethel Medical Center (Bieliefeld, Germany), in 73% of cases.
One effective non-drug treatment for mesial temporal lobe epilepsy is vagus nerve stimulation, or VNS therapy. This treatment method is non-invasive, therefore all surgical risks associated with neurosurgical intervention are almost completely eliminated. VNS therapy can be used in patients with a long history of the disease and bilateral mesial temporal sclerosis. Medical professionals have successful experience in treating severe drug-resistant forms of symptomatic temporal lobe epilepsy using VNS therapy.
Currently, symptomatic temporal lobe epilepsy is no longer an absolutely unfavorable form of the disease leading to disability. The use of rational pharmacotherapy and various non-drug treatment options allows, in most cases, to achieve remission of epileptic seizures and significantly improve the quality of life of patients.
Clinical picture
The main clinical sign of temporal lobe epilepsy is epileptic seizures. They arise suddenly and are expressed in the patient’s unconsciousness, loss of orientation, muscle cramps, etc. In this case, a characteristic feature is the fact that during a seizure the patient turns his head and squints his eyes towards the temple in which the area of epileptic activity is concentrated.
Other symptoms of temporal lobe epilepsy include:
- frequent, even systematic dizziness;
- headaches and migraines;
- visual and auditory hallucinations;
- olfactory paroxysms;
- squeezing or bursting sensation in the heart area;
- coordination problems;
- various forms of mental disorders;
- automation of gestures and sounds;
- personality distortions, etc.
Focal epilepsy: what is it?
This pathology is characterized by epileptic seizures caused by a clearly localized limited zone of increased paroxysmal activity. Most often they are secondary in nature. Paroxysms can be partial complex or simple. The clinical picture depends on the location. Diagnosed by clinical data. EEG and MRI are also indicated. Therapy includes antiepileptic drugs and treatment of the primary disease. According to indications, resection of the epi-zone is possible.
Diagnostics
To make an accurate diagnosis, the doctor must compare a lot of factors. The primary diagnosis of temporal lobe epilepsy includes recording symptoms, frequency of attacks, drawing up a detailed medical history, and identifying possible causes or factors in the development of the disease.
Based on the data obtained during the initial diagnosis, the doctor determines the necessary laboratory and hardware tests:
- MRI of the brain;
- PET CT;
- electroencephalography;
- polysomnography.
Surgery
In case of ineffectiveness of conservative therapy, intolerance to basic antiepileptic drugs even in the smallest permissible doses, or an increase in epileptic seizures that maladapt the patient, surgical treatment is resorted to. For surgical intervention, a mandatory factor is the presence of a clear epileptogenic focus. Surgical treatment is highly effective: about 80% of patients experience a significant reduction in the frequency and severity of attacks after surgery. In half of the operated patients, seizures disappear completely, social adaptation improves, and intellectual functions return. It is not recommended to resort to surgical intervention in case of severe general condition of the patient, severe mental and intellectual disorders. Temporal lobe epilepsy, the treatment of which is a complex and controversial procedure, requires constant monitoring by doctors.
Preoperative examination involves all possible types of neuroimaging (electrocorticogram, video-EEG monitoring, passing tests to identify the dominance of the cerebral hemisphere).
The neurosurgeon’s task is to eliminate the epileptogenic focus and prevent the movement and spread of epileptic impulses. The essence of the operation is to perform a temporal lobectomy and remove the anterior and mediobasal parts of the temporal region of the brain, the uncus, and the basolateral amygdala. There are risks with this type of surgery, and the patient should be informed about possible complications. Complications include Klüver-Bucy syndrome (hypersexuality, loss of feelings of modesty and fear), hemiparesis, mnestic disorders, complications after anesthesia.
Treatment
A complete recovery of the patient, that is, a complete absence of epileptic seizures throughout his life, is extremely difficult to achieve, and in some cases impossible. When resorting to conservative therapy, the main task that doctors set for themselves is to reduce the frequency of attacks and other manifestations of the disease to a minimum.
Conservative treatment of temporal lobe epilepsy involves the prescription and administration of antiepileptic drugs.
During drug therapy, the doctor systematically monitors the patient’s condition and progress from taking the prescribed medication. If undesirable side effects occur, treatment is adjusted, the drug is replaced, or additional symptomatic therapy is provided.
If no positive dynamics are observed from conservative therapy over a long period of time, surgical treatment of temporal lobe epilepsy may be required. For this purpose, experienced neurosurgeons are involved; the following operations for temporal lobe epilepsy are performed:
- temporal resection;
- focal resection;
- selective hippocampotomy;
- amygdalotomy.
Our clinic has everything necessary for accurate diagnosis, effective and comfortable treatment of patients with epileptic seizures. Patients with attacks of loss of consciousness are treated by neurologist-epileptologist Maxim Anatolyevich Palagin.
Secondary generalized seizures
Observed as the disease progresses. During such attacks, the patient loses consciousness and is paralyzed by convulsions in all muscle groups. As temporal lobe epilepsy progresses, it leads to complex mental and intellectual disorders. There is memory deterioration, slowness in movements, emotional instability, and aggressiveness. The frequency and severity of seizures in temporal lobe epilepsy are variable and varied, characterized by spontaneity. The female body can react with menstrual irregularities. Symptoms of temporal lobe epilepsy can manifest themselves as symptoms of other diseases, which makes diagnosing the disease more difficult.
Our specialists
Yushina Maria Alexandrovna
Head of the Center for Epilepsy and Paroxysmal Conditions.
The doctor is a neurologist. Epileptologist. Ozone therapist. Physiotherapist Experience: 7 years.
Kordonskaya Irina Sergeevna
Pediatric neurologist of the highest category. Epileptologist. Neurophysiologist (EEG diagnostic doctor). Experience: 24 years.
Volkova Svetlana Anatolevna
Head of the Center for Parkinsonism and Extrapyramidal Diseases.
The doctor is a neurologist of the highest category. Epileptologist. Ozone therapist. Physiotherapist. Experience: 26 years.
Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
general information
Focal epilepsy refers to all cases of epileptic paroxysms if they arise due to a local focus of increased epi-activity in cerebral structures. The source of excitation begins focally. Gradually spreads to the surrounding brain tissue. This provokes secondary generalization of the attack. It should be differentiated from paroxysms of unrealized epilepsy with a primary diffuse nature of excitation. There is a multifocal form. It is distinguished by the presence of several local zones of excitation.
FE accounts for approximately 82% of all epileptic syndromes. In 75% of cases, the onset occurs in childhood. Most often, the root cause is a violation of brain development of infectious, traumatic or ischemic origin. Such secondary focal epilepsy appears in 71% of patients.
Read also
Alcoholic epilepsy
In accordance with the International Statistical Classification of Diseases developed by the World Health Organization, alcoholism is considered a “dependence syndrome” and is included in the section of behavioral,…
Read more
Epilepsy and pregnancy
Managing patients with epilepsy and pregnancy is incredibly complex and challenging. What are the features of pregnancy in patients with epilepsy? In 1-2% of cases there is a chance of developing epileptic...
More details
Treatment of epilepsy in Samara
Epilepsy therapy is a long process and requires interaction between the epileptologist and the patient. Currently, it is possible to stop attacks and achieve remission in 60%! How to do it? Basic…
More details
Symptoms of epilepsy
How does epilepsy manifest? The most “famous” epileptic attack is a convulsive one, as the most “bright” one, this attack includes general tonic-clonic seizures, blueness of the face, salivation, ...
More details
Causes of epilepsy
“Where did my seizures come from? There are no epileptics in our family!” - the most common phrase at the reception, we will tell you about the causes of epilepsy. Indeed, up to 70% of all epilepsies are genetically predetermined...
More details
Epilepsy with myoclonic absence seizures.
Epilepsy with myoclonic absence seizures (EMA) is a form of absence epilepsy characterized by frequent absence seizures accompanied by massive myoclonus of the muscles of the shoulder girdle and arms, and resistance to therapy. The onset of attacks in UAE varies from 1 to 7 years (on average, 4 years); Boys predominate by gender. Myoclonic absence seizures are the first type of seizure in most patients. In some cases, the disease may begin with GSP followed by absence seizures. Complex absence seizures with a massive myoclonic component constitute the “core” of the clinical picture of UAE. Absence seizures are typical with intense myoclonic twitching of the shoulder girdle, shoulders and arms, usually of a bilaterally synchronous and symmetrical nature. In this case, a slight tilt of the torso and head anteriorly (propulsion), abduction and elevation of the shoulders (tonic component) may be observed. Most patients also experience myoclonic jerks of the neck muscles (short serial nods), synchronous with jerks of the shoulders and arms. A high frequency of absence seizures is characteristic, reaching 10 attacks per hour or more. The duration of the attacks ranges from 5 to 30 seconds, and long absence seizures are typical - more than 10 seconds. Attacks often become more frequent in the morning. The main factor provoking the occurrence of absence seizures in UAE is hyperventilation. In most cases (80%), absence seizures are combined with generalized convulsive seizures. A rare frequency of GSP is characteristic, usually not exceeding 1 time per month. EEG changes in the interictal period are detected in almost all cases. Slowing of the main background recording activity is observed infrequently, mainly in patients with intellectual deficits. A typical EEG pattern is a generalized spike (or, less commonly, polyspike) wave activity with a frequency of 3 Hz. Reliable for establishing the diagnosis of EMA is the appearance of discharges during electromyography in response to myoclonic muscle contractions that occur synchronously with peak-wave activity on the EEG (polygraphic recording). Treatment. Initial treatment is carried out with monotherapy with drugs derived from valproic acid. The average dosage is 50-70 mg/kg/day; if well tolerated, gradually increase to 80-100 mg/kg/day. In most cases, monotherapy reduces attacks, but does not lead to sufficient control over them. In this case, it is recommended to combine valproate with succinimides or lamotrigine.
In almost all patients, when using polytherapy in adequately high dosages, it is possible to achieve good control over attacks, however, remission occurs only in 1/3 of cases. Most patients have serious problems with social adaptation.
Forecasting
The most important rule for making a further forecast depends solely on its causes of development. When using medications, only 35% of patients manage to cope with the disease. Most often, conservative treatment only helps to reduce seizures, but not completely eliminate them.
As a result of surgical procedures, recovery occurs in almost 50% of cases, and 70% of patients experience a decrease in the frequency of epi-symptoms. In some situations, surgery can cause speech disorders, alexia, mental disturbances and other complications.